Frances M. Alba, MD, presented “An Assessment of Research Training Among US Urology Residency Programs, Including Characteristics, Resources, and Barriers Associated with Outcomes” during the 24th Annual Innovations in Urologic Practice on September 13, 2019 in Santa Fe, New Mexico.
How to cite: Alba, Frances M. “An Assessment of Research Training Among US Urology Residency Programs, Including Characteristics, Resources, and Barriers Associated with Outcomes” September 13, 2019. Accessed Apr 2024. https://grandroundsinurology.com/an-assessment-of-research-training-among-us-urology-residency-programs/
An Assessment of Research Training Among US Urology Residency Programs, Including Characteristics, Resources, and Barriers Associated with Outcomes – Summary:
Frances M. Alba, MD, reviews the findings of a survey-based study she conducted to assess the current state of American urology residency programs, which she presented at the 98th Annual Meeting of the South Central Section of the American Urological Association. She emphasizes the importance of research training and scholarly activity for the well-being of residents and faculty, as well as for the overall advancement of urology.
Abstract:
The Accreditation Council for Graduate Medical Education (ACGME) requires urology residency programs to “advance knowledge of the basic principles of research.” Residents must “participate in scholarly activity.” Faculty “should…support residents in scholarly activities.” They “should demonstrate scholarship…by publication of original research and presentation at professional and scientific meetings.” However, these requirements do not define factors associated with effective scholarly activity training for urology residents and barriers to achieving these goals.
Dedicated research time has repeatedly been shown to correlate with increased resident publication in urology and in other medical specialties. Months of protected research time and number of publications before residency are significantly predictive of the number of manuscripts submitted during residency. Lack of time, money, and mentorship are associated with decreased resident scholarly activity. However, there has been a rapid trend away from offering dedicated research time in urology residency programs.
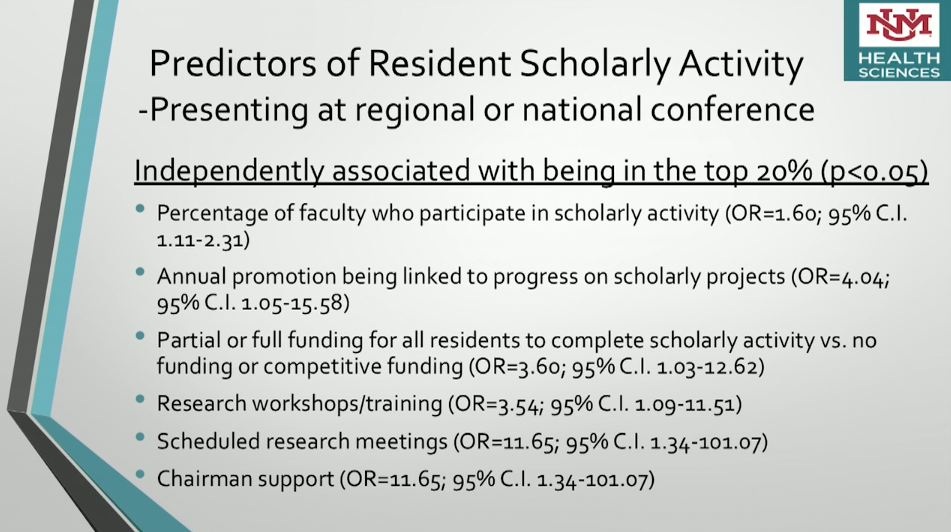
The combination of a dedicated research program/curriculum for residents, increased funding, and access to research support staff improved both resident and faculty scholarly activity and productivity. Research requirements, supportive program directors, and faculty mentorship are all associated with increased resident scholarly activity. This suggests the culture of research at the institution is a major factor.
We identified and presented the results of a survey of urology program directors. The resources and barriers to faculty and resident scholarly productivity were reviewed. Recurring themes were research curriculum, faculty attitudes and experience, chairman support, the lack or presence of a research director, and funding. Manuscript preparation and publication are important aspects of the training process. Scholarly activity impacts acceptance into fellowship, career in academic medicine, and faculty promotion.
The advancement of research in urology and the maintenance and growth of surgeon scientists is critical for continued improvements in patient care.
About the 24th Annual Innovations in Urologic Practice
Innovations in Urologic Practice (Innovations) is an annual, multi-day, CME-accredited conference devoted to innovative diagnostic and treatment strategies for and controversies related to some of the most common urologic problems in the current era. The topics covered include oncological management of the bladder, kidney, and prostate. The conference also emphasizes general urology topics in pelvic reconstruction and trauma, men’s health, and infections in the urology patient. Dr. Alba presented this lecture during the 24th Innovations in 2019. Please visit this page in order to register for future Innovations meetings.