Tobias S. Kohler, MD, MPH, presented “From PROPPER to EROS: Lessons Learned from Penile Implant Registry” at the Jackson Hole Seminars on February 7, 2018 in Jackson Hole, Wyoming.
How to cite: Kohler, Tobias S. “From PROPPER to EROS: Lessons Learned from Penile Implant Registry” February 7, 2018. Accessed [date today]. https://grandroundsinurology.com/From-PROPPER-to-EROS/
Summary:
Tobias S. Kohler, MD, MPH, discusses limitations and biases in literature regarding inflatable penile prosthesis (IPP), and how they led to the development of the Prospective Registry of Outcomes With Penile Prosthesis (PROPPER) study and the upcoming Erectile Restoration Outcomes Study (EROS). He describes best practices when performing penile implant surgery, such as infection control, reservoir replacement, wound closure, and patient selection.
From PROPPER to EROS: Lessons Learned from Penile Implant Registry – Transcript
Click on slide to expand
Objectives
What I’d like to share with you today is I want you to understand the paucity of evidence of round penile implants. I want to review the research that attempts to address this paucity, and finally share with you the many complications, which I have experienced and hopefully you can avoid them in the future.
How should one describe the current quality of scientific research concerning IPPs?
So, how should one describe the current quality of scientific research concerning IPP’s? The answer is suboptimal. I like that word. It can be used a lot. It can be very bad or just kind of bad, but the point is that if you look at the evidence surrounding penile prostheses, when we recently published Oxford recommendations based on what to do, 57% are based on grade C recommendations. There is very, very scant high quality literature surrounding penile prostheses. Now, you’ll see the reference here in the bottom corner. Any reference which is in green is something that I was involved in. The reference in white is something that I was not involved in writing, and I will point out the important references as we go, in case you want to forget everything else about this talk. There are two references that we’ll have you look up, not specifically related to penile prostheses.
Okay, so why does it matter that the literature is poor? Well, if you have poor literature, let’s say that people wrongly think that the penile prosthesis infection rate is 1% when, in fact, it’s 5%. What does that lead to? Well, it leads to a lot of problems. Number one, you tell the patient the wrong data, so he’s disappointed if he gets an infection, because you said it was going to be great, but it wasn’t. Next, you can have discouraged surgeons, because you start out, you get infections. Why am I getting infections? This doesn’t make sense. All of my peers are getting zero infections. So, that discourages them, and then finally, payers, if they get a hold of the literature and they start to pay us based on our outcomes, if they have the wrong numbers, they’re not going to pay us, we have too many complications, right?
Why is existing research suboptimal for IPPs?
So, what’s the source of bad literature? Well, first of all, 75% of all implants put in are done by surgeons who do less than four a year. Are these guys publishing results? Probably not. So, a lot of literature that we have published is biased towards the high-volume guys who may or may not reflect reality of what their true infection rates are. Another thing is that if you were to try to prove some kind of technique as a superior infection reduction protocol, it would take 34,000 study subjects to show improvement from 3 to 2.5%, so it’s not going to happen. So, we don’t have any randomized, controlled studies to prove any of this stuff, so we have to go with other data. Well, the data that we have right now is really suboptimal because one, there’s a publication bias for positive results. Nobody is going to publish their horrible results, number one. Number two, high-volume surgeons are more likely to publish. Number three, and this is a big one, attrition bias. If you look at the literature, you start with 100 implants, of the 60 that came back and saw me, they were doing great. What happened to the other 40? Well, maybe they went to another surgeon, they have infection, et cetera. So, this is a huge problem in our current literature and finally, PIF form. These are product information forms that the device company reps fill out in implant cases. They are, like, they’re not on the case, so they probably are not filling out forms, so when you look at the industry data, they are missing a lot of data.
Here’s a personal example of attrition bias. So, I’m a member of the PROPPER Study, which I’ll talk about in a second. Basically, we published an abstract of the AUA, saying we have zero percent infections in our first 466 patients. Aren’t we awesome? Yeah, wait longer is the bottom line, right? So, after six months we had about a 3% infection rate, but that’s the problem with data. If you don’t have good long-term follow up, if you don’t follow these patients long term, you’re going to miss them. So, a personal example from IM literature that, yes, these problems do occur.
PROPPER Registry
Okay, so what is the PROPPER Registry? The PROPPER Registry was originally constructed by AMS back in June, 2011 and there were 11 sites, specifically targeted high – – implanters, and it was originally supposed to be both company’s products going to a database for comparison, and the data was supposed to be controlled by the investigators. It evolved into not that, so basically, now, it’s just 11 investigators with only AMS products. But, what is good about it is that it is prospective and has 1000 patients, and we get the best information that we have so far. But, it is flawed. Why is it flawed? Well, first of all, only 11 implanters. They are high volume, so I mean, it does not reflect reality. Number two, in the PROPPER database, you could include who you wanted and exclude who you wanted, so, there is the possibility that you basically don’t include the diabetics and the high-risk guys in your series, so that’s a big flaw and, of course, there’s attrition lost to follow up. So, of the 1100 patients that we have in our series, 1200, we’ve got follow up on 900 in the first year, and then less and less for each subsequent year. So, it’s better, but not great.
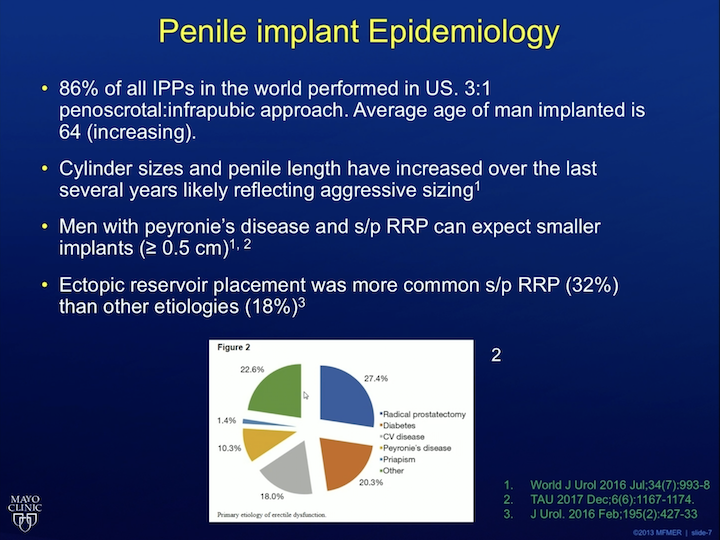
Penile Implant Epidemiology
So, a lot of these studies now are basically, we learn from doing the PROPPER registry, or from doing, I learn from doing implants, some involved in PROPPER, some leading to the EROS Registry which I’ll talk about in the last couple of slides.
So, what about epidemiology implants? Well, 86% of IPP’s in the world are performed penoscrotally. The average man who gets a penile implant is 64 years old. This age is increasing. Very interesting also cylinder sizes that are being put in are increasing over the last several years. This is likely reflecting sizing. We’d like to think that maybe penises are getting bigger. That’s probably not true. The other thing that you have to tell patients, that if you have Peyronies disease and you are status post-prostatectomy, you are likely to have a smaller implant compared to those who don’t have those conditions. We found that in two separate studies. The other thing that the PROPPER study found was that ectopic reservoir placement was more common after prostatectomy. Now, the standard reservoir goes into the space of Retzius next to the bladder. You have to puncture through the transversalis fascia. Ectopic reservoir avoids this, which we’ll talk about in a second, and so what we found that, in the study, it’s much more common after prostatectomy to put it in the ectopic location. Interestingly, Coloplast, the competitor of – – used this data to get FDA approval for an ectopic location of their reservoir for their product, but AMS/Boston Scientific now did not. And finally, the pie graph basically shows you why men get implants. Most of the time, it’s either diabetes, or vascular disease, or prostatectomy.
What are the satisfaction rates with IPP & what causes dissatisfaction?
Okay, based on the PROPPER data now, which we have about five years of data on, satisfaction, so people are satisfied with this. It’s great. At three years, 94% are very satisfied, satisfied or neutral, 6% are unhappy. Why are these guys unhappy? Well, most of the time, it’s because they think their penis is too small, or there’s problems with the surgery, they got an infection or device problem or they have problems with the pump. Ten percent of all patients in our series don’t actually use their implant. They just kind of leave it sit there, but they are happy they got it regardless, because it gives them the confidence to go out and do the stuff that they want to do. What are predictors of dissatisfaction? Well, if the patient was depressed in the first place, the ultimate penile girth that ended up being significant based on satisfaction, surgical problems, if they had problems, they were like, they would be dissatisfied, and in our initial perturbations of data if they had LUTS. That actually predicted things. That has fallen out of the model so far. And then, in a recent finding, IPP insertion improved depression. That’s actually a paper written by Dr. Cara, which is in press for the Journal of Sexual Medicine.
What about the IPP reservoir?
Okay, so let’s talk about the reservoir. So, you’re putting the reservoir in space of Retziu, and then you see this. What do you do? So, that is audible bleeding, people running around the operating room because you’ve got likely an iliac injury. So I always ask my residents, you know, “What would you do in this situation?” Well, the answer is stay calm, let anesthesia know, call the vascular surgeon for help, et cetera. But, because of that fear, that’s the main reason why a lot of people don’t do penile prosthesis, because they are afraid of this catastrophic injury. So, this ectopic reservoir placement is a game changer. Basically, you can avoid potentially injuring the iliacs by putting the reservoir in a separate space, and the PROPPER data showed that an ectopic reservoir placement has the same amount of complications as the standard reservoir placement in terms of herniation. But, the risk of causing a catastrophic injury, like iliac injury or a bowel injury, is zero with the ectopic placement if done properly. We also learned that what we can do is if you have an old reservoir in place, sometimes taking out the old reservoir is the cause of as much mischief as putting a new one in. So, in a non-infected setting, it is perfectly legitimate to leave that old reservoir sit there. It’s called a drainer retain strategy, and put a new one in on the other side.
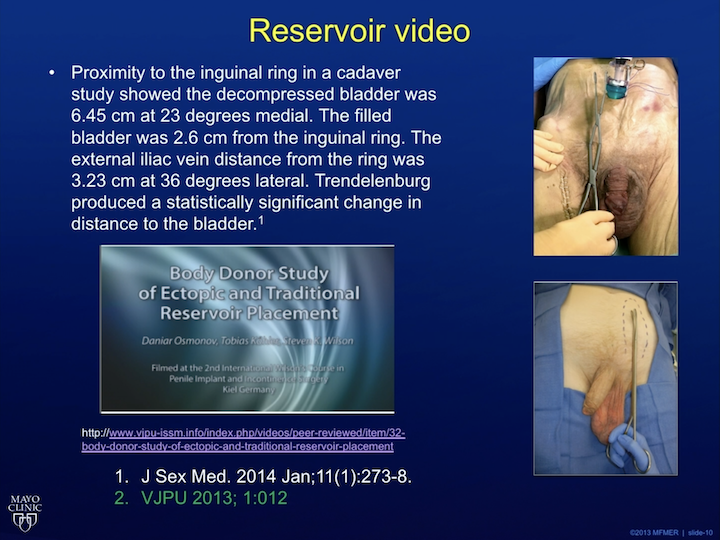
Reservoir Video
Okay, so basically what this video showed was a cadaver study of people using a scissors to place, to make a spot for the reservoir in the space of Retzius, and you see from a laparoscopic camera, the scissor coming down and, like, puncturing in and missing the iliac vein by, like, that much, and missing the bladder by that much. If you look at a nice study done by Gerrard Henry, he basically measured how far away the iliac and the bladder was from the typical puncture site, and it’s really close. The fact of the matter is that most high volume implanters have had an iliac injury because there is aberrant anatomy, and sometimes you just can’t avoid these things. You don’t know who has aberrant anatomy. So, what we do is we take this long green clamp here, and we kind of just put it above the fascia, and that’s where the ectopic reservoir goes. So, that’s the ectopic reservoir placement that you need to know how to do if you want to be a modern implanter. Now, the other thing that you need is this. This is the best instrument to put a reservoir in, right? So, I’m a Viking’s fan and very depressed that they lost to the Eagles, but I’m happy that the Eagle’s won, but this is all you need to put a reservoir in. If you use an – – track and you get it in the external ring, you can perforate the fascia with your finger every time. And if you can’t perforate it with your finger every time, then you can use a ring clamp to place it ectopically and you will never have an injury. Moving on.
What’s new in IPP infection?
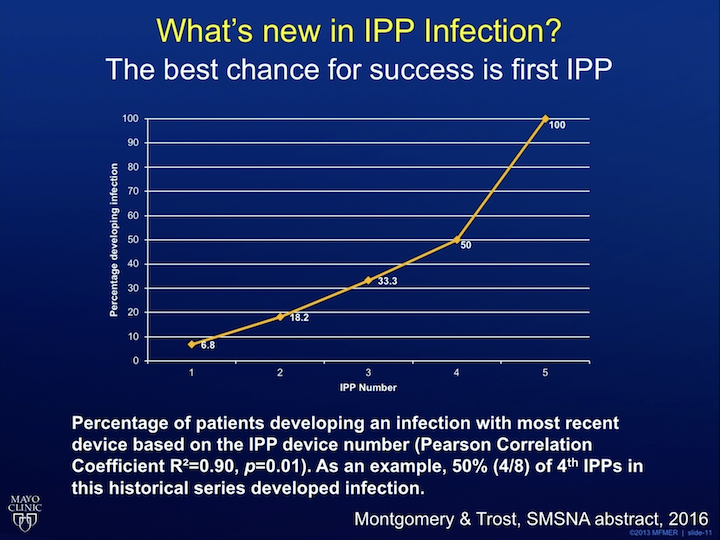
What’s new in IPP infection? Well, the best chance for success is your first prosthesis. This is some data from my partner, Dr. Trost. Basically, he had all these patients come in for revision or referral surgery. The numbers of surgeries that they had was direct proportional to the likelihood of infection. By the time they’ve had their fifth implant, all of them had an infection at one point or another, so your best chance for success is the first try, and every subsequent one is more and more likely to have problems.
Infection Control “Be PACIFIED”
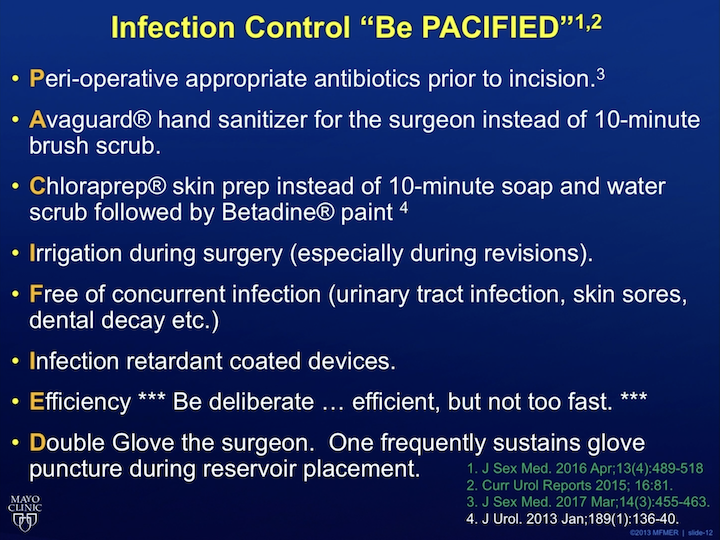
When we look at infection control, the literature is not awesome, but this is a mnemonic that I created called, Be PACIFIED, for what I think are the most important steps to help prevent infection. Use appropriate peri-operative antibiotics. Use Avagard instead of the standard hand prep. It’s proven to be just as good. Chloraprep on the skin is proven superior. A study that I love out of WASU with this – – group is they swabbed the penile implant site right after using the standard betadine prep. Dr. Stoller, give me a number between 31 and 33.
Dr. STOLLER: 32.
32% of the patients had culture positive swabs when you used standard betadine. That’s just absurd right? One third of the patients still had bacteria on the skin after using the prep. Dr. Mohl, what percentage of patients do you think have positive cultures after using Chloraprep
Dr. MOHL: You told me to say 8%.
Eight percent is correct, so you decrease the infection rate by 75% by using Chloraprep instead of standard betadine. Use irrigation during surgery. This is proven to prevent infections or revision and make sure they don’t have other infections like UTI’s, skin sores, dental decay. Use infection retardant coatings. These, all devices come coated now. Be efficient, but not too fast, and then double glove. That’s the Be PACIFIED mnemonic.
What’s new in IPP Infection?
What else is new in IPP infection? Well, this is a crazy thing. If you look at the bottom picture here, this is a patient that came to me. He was in his deer stand, and he said he kept scratching his scrotum after his implant, right? He’s like, doc, I think something’s wrong. I’m like just, I think you’re right, something is wrong with that picture. He doesn’t have any infectious signs. He’s not on antibiotics. He doesn’t have fever, he doesn’t have pus drainage. He’s fine. What is going on? Why is this guy not get infected where some other diabetic guy gets infection? We don’t know. So, there is this other thing called Biofilm. It’s whenever you put an implant in, when you revise it, you see this stuff on the device. It’s the same thing you get in your teeth, it’s the same thing that goes in oil pipelines. This Biofilm created by bacteria is basically like an agent, a shield for the bacteria to be protected, and when you do a revision surgery, sometimes that Biofilm, that bacteria will get activated, and you get a raging infection, and you get all the problems. Now, why, sometimes, you get an infection with Biofilm and sometimes you don’t get an infection when the pump is coming out the scrotum- I have no idea. If you can figure out, this Biofilm issue, you will be a billionaire because, like I said, it clogs oil pipelines. So, if you can prevent the oil pipelines from being clogged, you can make a lot of money. All right.
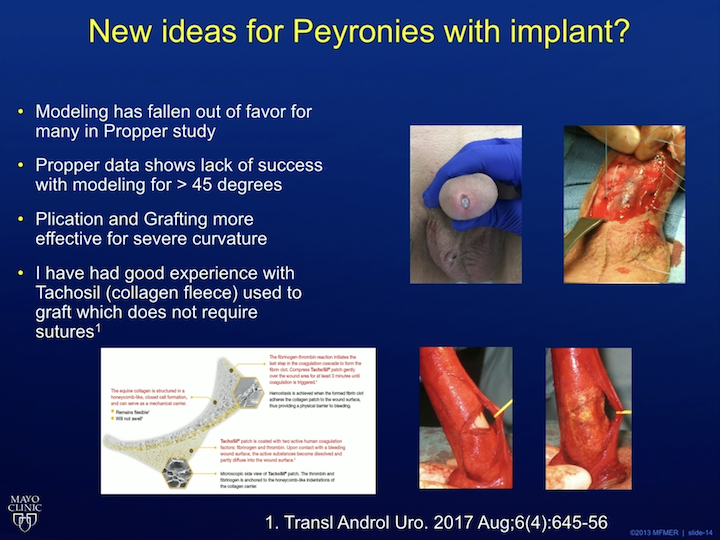
New ideas for Peyronie’s with Implant?
What else is new? Well, from the PROPPER study, we realize that, of the high volume guys, when treating Peyronie’s disease, a concurrent curvature with implants. A lot of us have stopped doing penile modeling. Here’s a picture of a patient of mine with the implant coming out the urethra. That’s a result of penile modeling. So, I stopped doing that and now we have different types of grafts we can use. I’ve had success with Tachosil. My partner, Dr. – – , a friend in Munich he started doing this, and basically, it was like a postage stamp that you can put on the implant instead of having to sew a graft in place for Peyronie’s. It cuts the surgical time and it works very, very well.
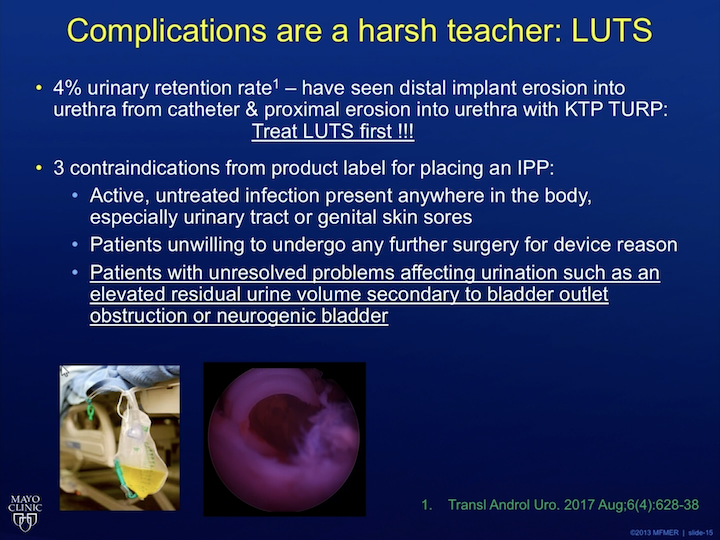
Complications are a harsh teacher: LUTS
Okay, let’s get into some other complications specifically. So, of my first 100 patients, my number one complication was urinary retention. If you look at the product insert for the implant, which I didn’t do until I was, like, sitting in the OR one day, watching my fellow operate, I saw that the third contraindication for putting in a penile implant, according to the Coloplast literature, is patients with unresolved problems affecting urination, such as an elevated PVR, secondary bladder outlet obstruction or neurogenic bladder. So, don’t put an implant in until you have addressed their LUTS first, because what happens, you end up having a catheter in place, then you get catheter erosion, et cetera. Or like, in this picture here, this is a guy who had an implant and then got a green light, and this is what we saw in his urethra, part of the implant tubing, so treat the LUTS first.
Complications are a harsher teacher: Wound closure
All right, wound closure. So, we know that guys complain about their penises being too short after implant surgery, so we started doing this scrotoplasty where we get rid of the scrotal skin between the scrotum and the penis, and some patients have such a bad scrotal like web that if it blows in the OR, the bed actually moves because there is, like, this scrotal sail. So, what we do is we take that sail down by doing a Heineke-Mikulicz like closure, and low and behold, some data showed that the patients thought their penis looked long and they were happier. I did about 104 of these, and then I found that a lot of them were dehiscing because I was having too much tension on the closure, so I learned the hard way that yeah, be careful with scrotoplasty, especially in diabetics and guys with small scrotums, because you end up with something like this. You get tubing sticking out of the scrotum and you end up having to do a revision or something else fancy.
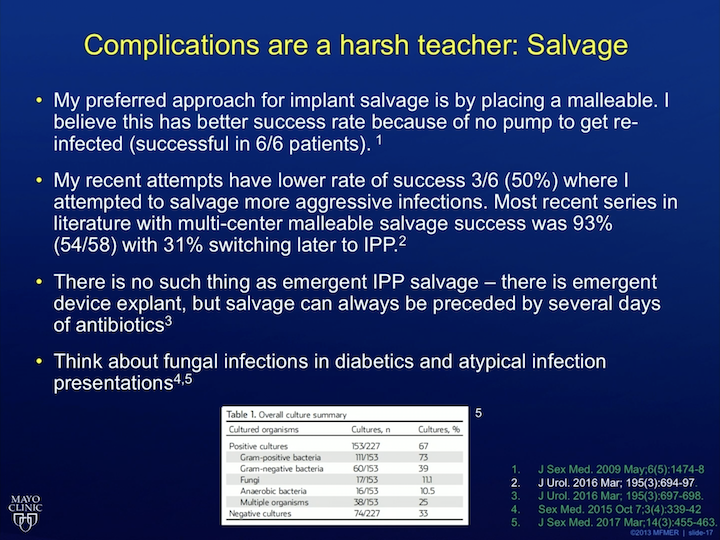
Complications are a harsh teacher: salvage
What about salvage? So, sometimes a patient will come to you with an infection. What do you do? Twenty years ago – – introduced a salvage technique where you can basically wash out the implant and put a new device in. I like to use a malleable approach for this where I put a malleable in, because I feel it gets less infected and it was very successful. In my career now, I’ve gotten more aggressive with even more aggressive bacteria, and low and behold, it doesn’t work. So, if they come in very sick, just take the device out. If they come in kind of sick, if they are kind of doing okay, then you can maybe get away with a malleable salvage. The other thing we learned recently is that the amount of fungus and atypical infections is going up, so the antibiotics that we currently use are not covering fungus and atypicals, so it’s highly recommend that in immunocompromised patients and diabetics, you increase your antifungal use and change your antibiotics.
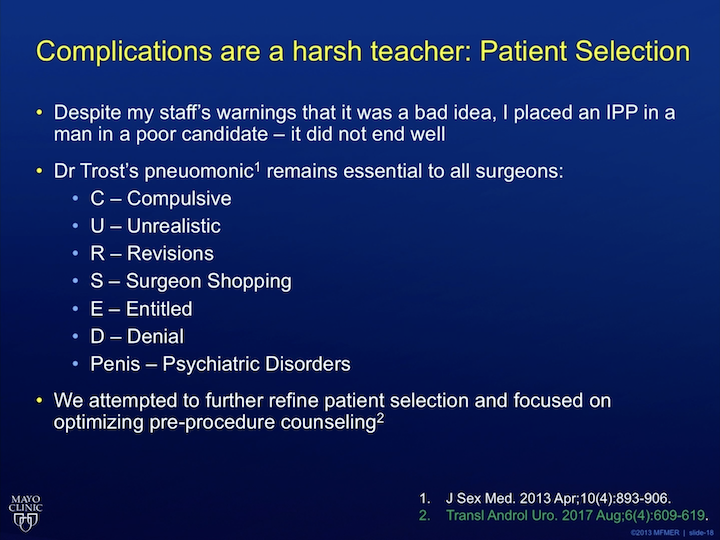
Complications are a harsh teacher: Patient Selection
Now, here are the two most important papers I want to call your attention to. Number one, patient selection. So, Dr. Trost, a good friend of mine, now a current partner at the Mayo Clinic, he wrote this paper and was called initially cursed penis. That was the name of the paper, but then he chickened out, and then he changed it to cursed patient, because he didn’t want to have cursed penis as the mnemonic in literature, but basically it’s a mnemonic stated the type of characteristics of patients that you want to avoid putting an implant in. I would argue to avoid doing any kind of cosmetic surgery in. So, this is a good one to read because it talks about counseling the patient’s properly beforehand, giving everybody in your office staff veto power to say, “This is not a good candidate, et cetera.” I’ve learned the hard way that, sometimes, if you implant the wrong patient, you end up with a lot of misery.
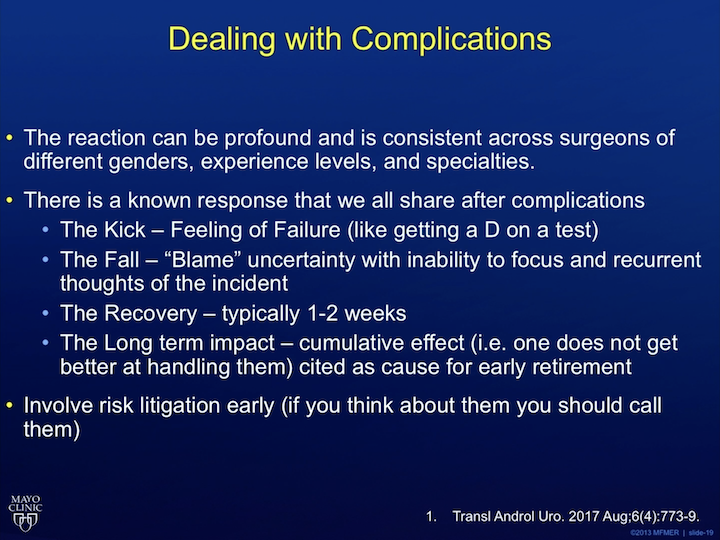
Dealing with Complications
Okay, now, the most important, that was the second most important. The most important paper I want you to look up on your own time is this one. So, did you guys know that there was literature on dealing with complications? So, Carol Ann Bolton, she’s a gastric surgeon from Canada. She came and spoke at my institution. Amazing stuff, so there’s a whole body of science about how surgeons react to complications. We’re never taught this, right? But, regardless of gender, age, experience, we all experience things the same way. One, complications happen. We get what’s called “the kick” by getting a D on the test. Two, next, we blame ourselves. We have these recurrent thoughts like, “What happened? What was wrong?” We’re having an okay day, all of a sudden, crack, we think about that complication again. It happens again and again and again. The data shows that we probably shouldn’t be operating heavy farm equipment during this one to two week period when we have these complications, because we don’t think straight. So, look up this article. It’s very important that we argue that any surgeon who has, does enough operations is going to get complications. Any resident needs to read this and learn the signs of what is going to happen when bad things happen, okay?
Finally, long term impact of complications, if you, you never get better at adjusting to these things. This is a career shortener. The more complications they have, the more likely you are to retire early.
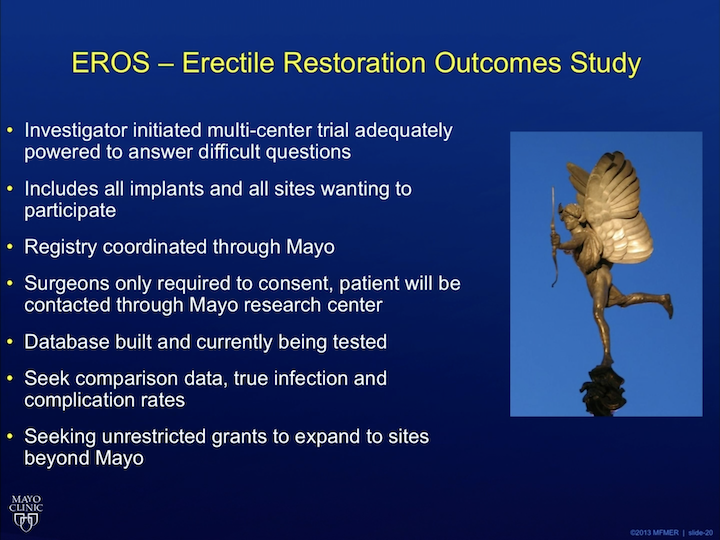
EROS – Erectile Restoration Outcomes Study
All right, this has lead to the EROS site, so this is something that I pitched to the industry four or five years ago. Finally, it’s coming to fruition. This will be a multi-centered trial, basically involving both device companies, products, you can put your data in as you see fit and then once you enroll a patient to study, everything else is taken care of for you. The Mayo registry will call the patients on your behalf, so there’s no attrition. So, look for this to come out in about six months when it will be done. Thank you so much for your attention and I hope you enjoyed the talk.