Patrick W. McLaughlin, MD, presented “The Modern Definition of Successful Cancer Treatment – Cure with Quality of Life” during the 24th Annual Southwest Prostate Cancer Symposium on April 14, 2019 in Scottsdale, Arizona.
How to cite: McLaughlin, Patrick W. “The Modern Definition of Successful Cancer Treatment – Cure with Quality of Life” April 14, 2019. Accessed Apr 2024. https://grandroundsinurology.com/the-modern-definition-of-successful-cancer-treatment-cure-with-quality-of-life/
The Modern Definition of Successful Cancer Treatment – Cure with Quality of Life – Summary:
Patrick W. McLaughlin, MD, discusses the balance of cure versus quality-of-life when treating prostate cancer patients. He details his approach to ensuring optimal patient-preferred outcomes using physician-as-advocate decision-making, as well as individual anatomical and tumor characteristics in guiding treatment planning.
Abstract:
When treating prostate cancer in the modern era, it is essential to take an individualized approach to every case. This means factoring in preferences and previously-held convictions regarding treatment choices, functional anatomy, and tumor characteristics of each specific patient to guide therapy decisions.
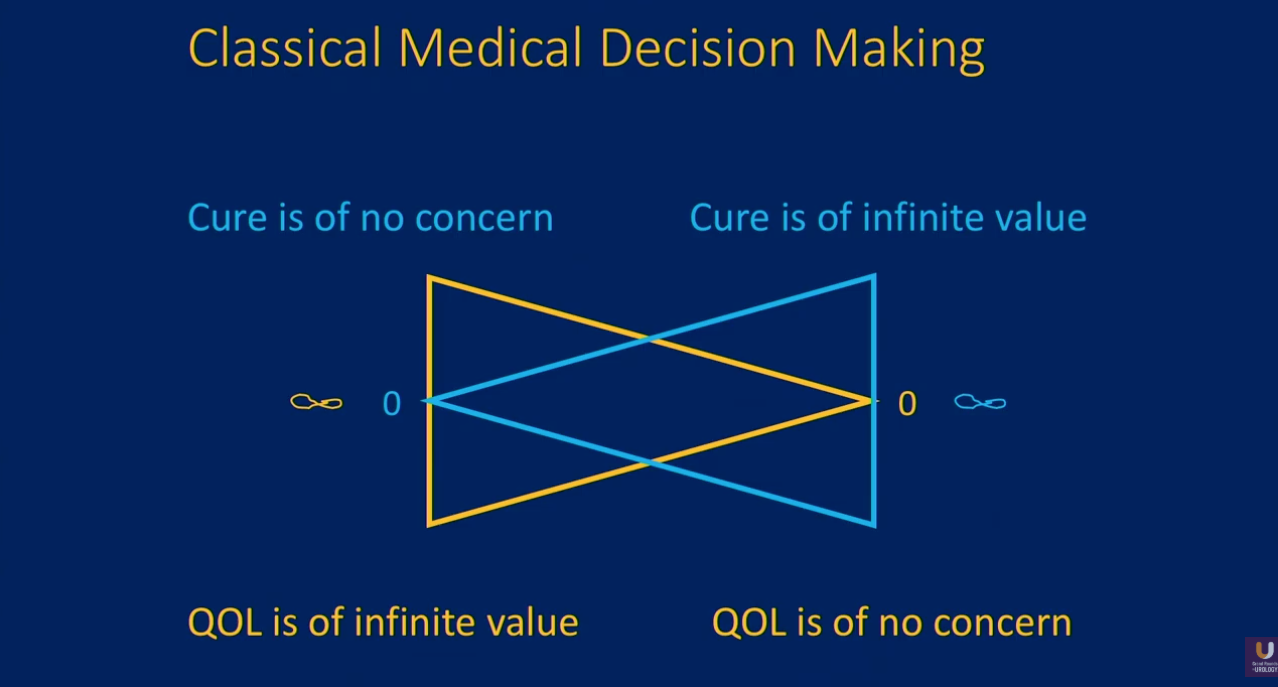
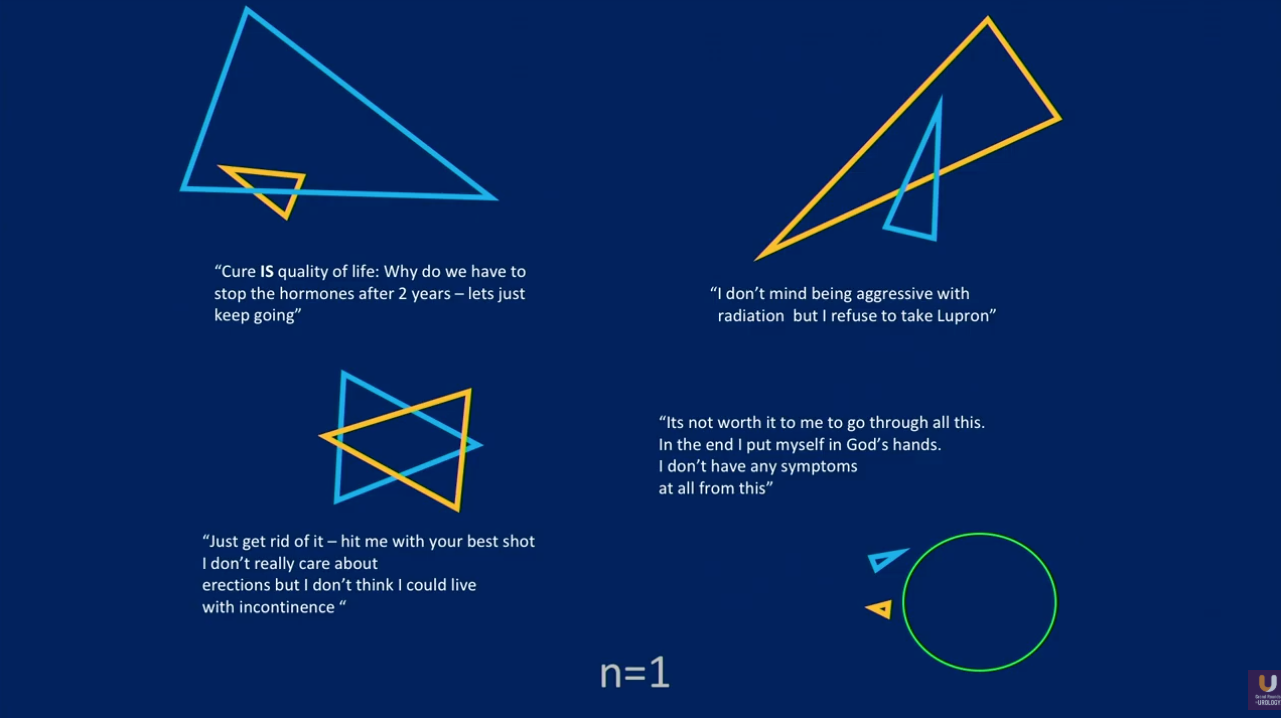
A contextualized structure of patient preferences in classical medical decision-making is a static, binary spectrum that sets the value of cure and the value of quality of life (QOL) in opposition. In other words, a patient may be infinitely more concerned with avoiding the adverse effects of certain procedures than receiving curative therapy, and visa versa. However, in practice, patients’ opinions on their care are much more nuanced and varied.
Navigating patient preferences presents a unique challenge for every case, but equally as important is the manner in which physicians counsel patients. While some patients may embrace a neutral attitude, in which physicians allow patients as much autonomy in their treatment decisions as possible, others may resent a physician’s lack of expert input on that decision.
Furthermore, physicians must maintain mutual multidisciplinary respect and avoid disparaging or extolling certain modalities based on their own personal specialty when counseling patients. Above all, physicians should advocate for treatments that will objectively offer the greatest likelihood of achieving patients’ desired outcomes given the individual characteristics of each case.
This presentation illustrates the application of individualized decision-making through case studies. The conversation analyzes the role of specific patient factors, such as sphincter length, nerve bundle configuration, and tumor extent and extension, and their role in predicting continence, sexual function, and curability outcomes. It also stresses the use of MRI, rather than relying on D’Amico risk information, in pre-treatment planning to refine the decision-making process.
About the Southwest Prostate Cancer Symposium
The Southwest Prostate Cancer Symposium (SPCS) is a multi-day conference that seeks to educate urologists, radiation oncologists, medical oncologists, and other healthcare professionals involved in the treatment of prostate cancer. The topics focus on current technical aspects of diagnosis and treatment of localized and advanced disease, particularly regarding imaging, technology, and training in the related devices. Dr. McLaughlin presented this lecture during the 24th SPCS in 2019. In 2020, the 25th SPCS will also offer training sessions involving imaging, scanning, and prostate cancer treatment-related devices on site. Please visit this page in order to register for future SPCS meetings.