Fernando J. Kim MD, MBA, FACS, presented “Culture of Patient Safety” at the Jackson Hole Seminars on February 7, 2018 in Jackson Hole, Wyoming.
How to cite: Kim, Fernando J. “Culture of Patient Safety” February 7, 2018. Accessed [date today]. https://grandroundsinurology.com/Culture-of-Patient-Safety/
Summary:
Fernando J. Kim MD, MBA, FACS, explains the evolution of patient safety culture since the 1980s, when public concerns arose regarding anesthesia complications. He highlights points from the American Urological Association’s (AUA’s) University Core Curriculum “Ethics” webpage, emphasizing organization, environmental control, and communication.
Culture of Patient Safety – Transcript
Click on slide to expand
The Culture of Patient Safety
What I’m going to talk about is the culture of patient safety. While this seems very intrinsic to our profession, a lot of things change, a lot of things we learn, particularly from other industries and this has been triggered by the American Board of Medical Specialties, almost a decade ago.
It was recommended to all of the boards of specialties, including the American Board of Urology, to develop a culture of safety among surgeons. And how to do that? Well, create a core curriculum, which I was involved with – – average about eight years ago. We started to go to courses. And there are several of them, but few that you can say it’s really worthwhile. We put a core curriculum, and we published under the AUA University Core Curriculum under “Ethics” tab. I’m pretty sure not a lot of people saw that. There is a 2.0, a new version, and now there is the Quality Improvement and Patient Safety committee. We’re writing a white paper about certain things that are important for you to prepare when you’re recertifying, and there’s going to be some questions asked and trying to understand exactly what we’re trying to identify as important topics.
Hippocrates Recognized the Potential for Injuries…
Like I said, it is very natural in our profession, the culture of patient safety. How we apply and how we communicate is maybe something that we could refine and be better. Since the medical school, since the old times, – – we do not want to harm anybody. We want to cure diseases. We want to be improving their life. We want to save lives. But, if you see what triggered all this in 1982, the TV ABC channel had this program about The Deep Sleep. The people had complications with anesthesia and they would even die. Then, you go to across the ocean, the British Royal Society, very close to that year, with Harvard Medical School, they put some statistics about deaths and injuries caused during or after anesthesia, or by [anesthesia]. So in 1984, everybody knows the ASA score, the anesthesia society, they tried to come together as specialists and created the foundation of Anesthesiologists and Patient Safety, and then, they started to grade, also, the types of ASA one, two, three, four, that everybody’s aware. And also at the same time in Australia, there was a big movement from that group.
Patient Safety is Now Recognized in Many Countries
What happened is that patient safety, currently, is very well-recognized in many countries, especially ours, that it is an important topic. The World Health Organization identifies this as something that is important, required to be paying attention by hospital administrators, by the different associations, and this triggered associations to create the American College of Surgeons has an AS-QIPS, NQIPS, and even the American Urological Association has, and one of the speakers here, Dr. Chris Gonzales, can tell you a lot about – – improvement and all the issues related to that.
Patient Safety is Now a New Healthcare Discipline
Patient safety became a new healthcare discipline. Actually, there are patient safety officers, quality officers, in some hospitals. Some people say, “Oh yeah, that’s the internal affairs guy.” And it’s something that brings a little bit of more attention, red flag, and it is very important to have one person that knows what surgical procedures are for our specialty, and also understands the medical side, like hospitals and so on, to understand how the patient safety issues are different.
So, what happened during this period, the decades of the 80s and 90s, is that this boom of information, people researching how many people were getting hurt with medical errors, or getting killed.
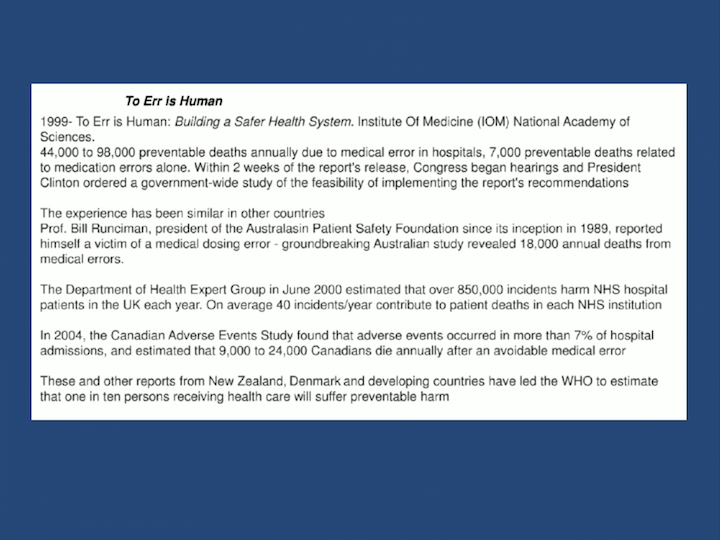
To Err is Human
This created a huge body of literature, and at the end of the 1990s, the Institute of Medicine created the report, To Err is Human, that demonstrated that 44,000 out of 98,000 preventable deaths annually were due to medical errors in hospitals. 7,000 preventable deaths related to medication errors alone. And this really triggered to the end of the spectrum from observation to political action. When Bill Clinton was president, they had a special commission and reports and recommendations given. So from that, what triggered globally, other countries like Britain, with NHS, National Health Services, and the Australian government, Australasian including New Zealand, they started to study all that. And if you see what the Department of Health Expert Group in June 2000, recently, estimated that over 850,000 incidents harm in the National Health Services hospitals in the UK each year, you can, on average 40 patients a day contribute for patients’ death. So, that’s a huge number. If you try to save one patient, and you have another 39 that are contributing to the death of one patient, this number is huge. It’s incredible.
So, these are reports that demonstrated what the problem is, and even how the number of patients are getting hurt, and the magnitude of the problem. What do you do with that information? Well, people have been studying several things since the beginning.
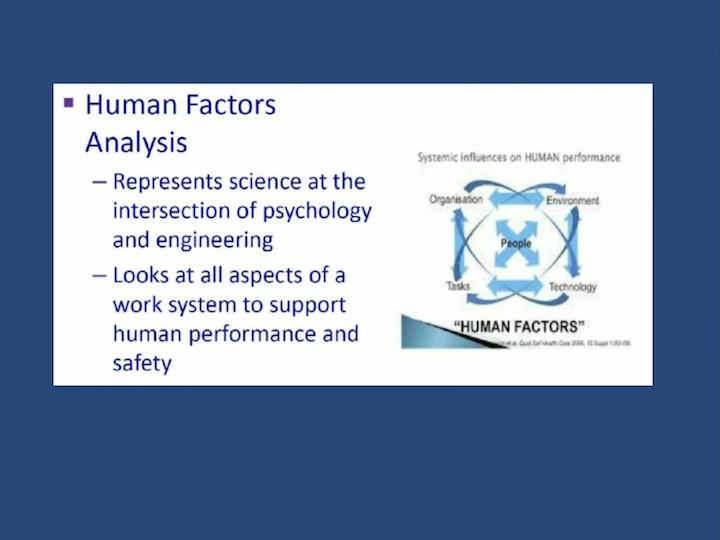
Human Factors Analysis
There are different ways that you can approach the problem, and safety has been an issue in all other industries, like aviation, car industry, any kind of industry where patients have to, construction, people can get harmed, employees can get harmed. So, psychology, psychiatrists, workman’s comp, all those different specialties, started to study. Human factors is a very important thing, as you know. For example, we know that a very important Korean flight that killed more than 290 patients, because in Korea, you have three years of military school. The pilot was most senior, and all men go to military service, and the co-pilot was more junior. He knew that the pilot was doing some big mistakes, but he didn’t say anything because of the culture of hierarchy, and more than 290 lives were lost. So, if you study all that, and they started to study all those incidents and accidents, and they found out that the human factor is very important.
So, what the analysis of this issues, it started to intersect with how a person thinks, what they learn, how they perceive things, and how they can interact with the technology and the services, that he has, or she has, to provide.
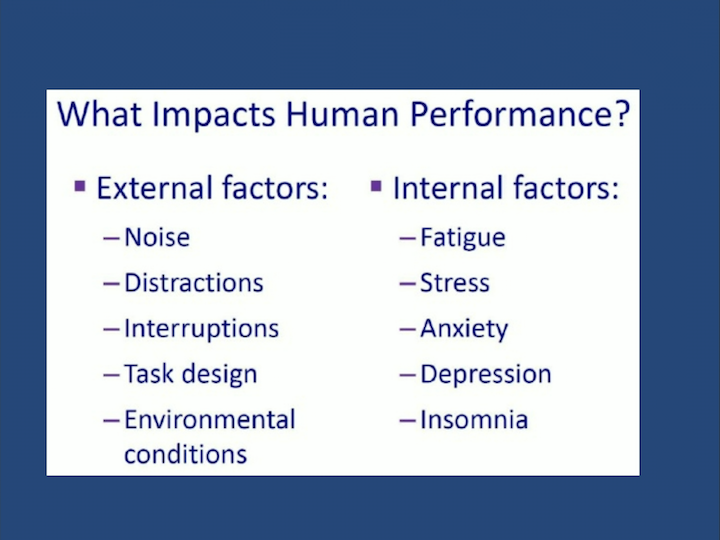
What Impacts Human Performance?
So, what impacts human performance, is we usually tend to underestimate our abilities, right, or overestimate? So, we are all probably guilty of this. No, don’t worry, I’ll do this case, yeah, you can book the other one on the other case, in the other room and I’ll follow up and I’ll run to the clinic, do a quick biopsy, come back, and, oh yeah, I’ll pick up my kid between the biopsy, the cysto, and a partial nephrectomy. But I will have time. But there’s traffic, where do you live? Oh, I live in New York. Oh, that’s okay, don’t worry, I’ll take an Uber. No, we’ve got to know our limitations. We cannot overestimate things, bad things can happen during that time. And right now, the next slide, I’d like you just to take a look, and try to read the color, not the word.
Quickly, Say the Color Not the Word
I know, it’s very early in the morning. So, it is a little bit tricky, because first you have to speak English. Second, you can’t have color blindness, I think. But it’s very difficult, because you’re trained with one thing, when you see the word’s pink, you think you’re seeing the color pink. But this is not pink, it’s purple, I think. But this is a clear example that I can show, in real time, that what you see sometimes, is not what you see. There are so many factors that influence that perception.
What Impacts Human Performance?
So, what impacts human performance? External factors. Now we are in the operating room, and there are general surgeons working on that, orthopedic surgeons, even urologists, and in the operating room, for example, if you have external factors like noise, distractions, interruptions, the task design is so complicating, environmental conditions—it’s too hot, too cold—can decrease your performance. Internal factors: if you are fatigued, running around, not sleeping well, stressed because of your RVUs, or your manager that is a pain in the neck, you’re having depression because you’re going through a very difficult time, those have to be taken care.
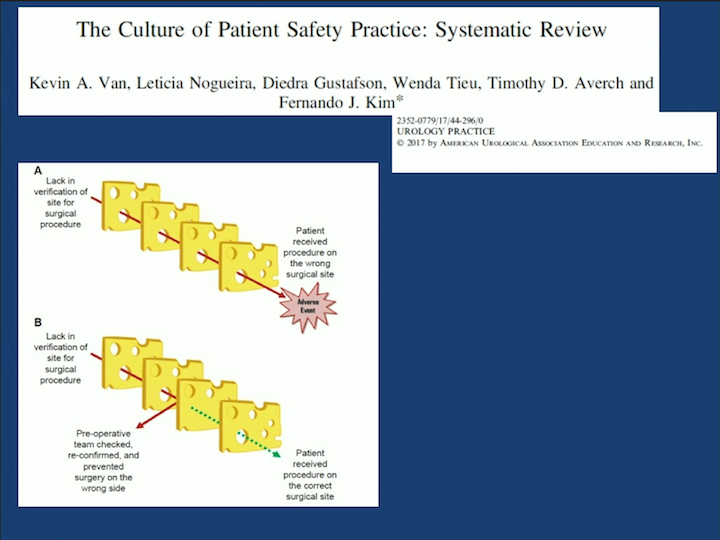
The Culture of Patient Safety Practice: Systematic Review
So, we did a systematic review and this June we put on the cover of Urology Practice, the James Reason’s cheese model. The cheese model, if you stacked up slices of cheese, of Swiss cheese, there are holes, right? If the hole is all the way through, if you start a problem here, and there’s several mistakes, there’s nothing that can block that. It will go through. But, if the hole has any kind of blockade there, that’s your first way that you can avoid a problem that was small, to be large. An example in the operating room.
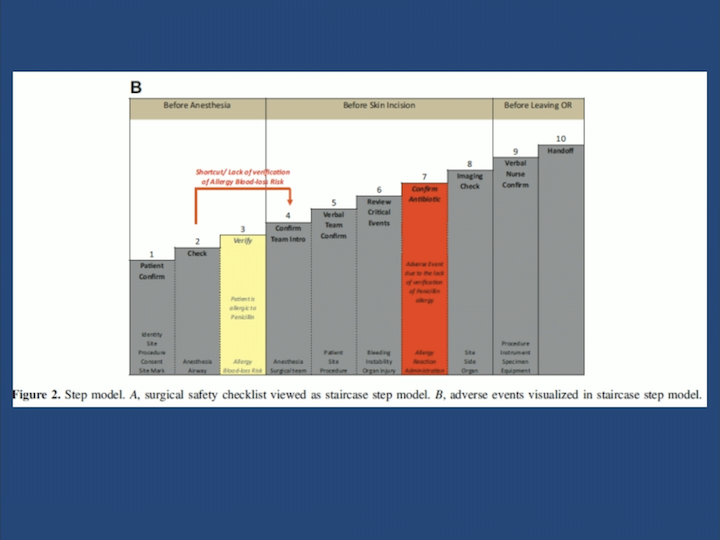
Before Anesthesia
There is the preparation from the OR, the operating room, and after. Simple case. Antibiotic allergy. So, the antibiotic allergy, if you see, on the pre-op, and you tag, and in the operating room it’s given, whatever protocol, thirty minutes before or during, but if it’s not seen and you give then, penicillin that the patient is allergic to, and have a bad reaction, if you didn’t have this red flag here, you would not be able to attend to this problem and avoid any complications. This is the Swiss cheese model. It means if this was not done, the hole would be all the way through, and this and this would not be alert sufficient to that.
System Thinking
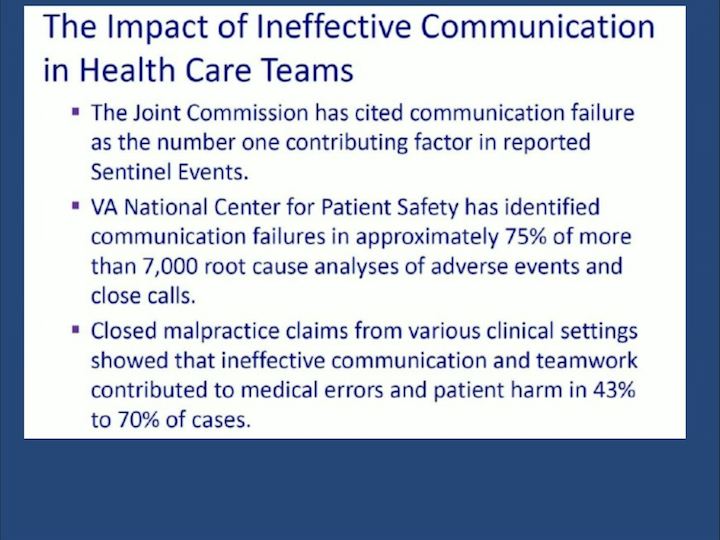
So that created the word “System Thinking.” It’s the new ways of thinking the work you do. It depends on habits, it depends on the events that you’ve experienced, patterns of behavior, systems structures, and mental models. But the most important message is to take that opportunity to learn. The most important, communication. Even your deep feelings, and gather feedback, and don’t think that feedback is against you. It’s probably taking you to a different level, so you can communicate better.
AUA University Patient Safety
So, this is the AUA University Core Curriculum under “Ethics,” that you can check. There are some things that we tried to put, specific for urology. Endourology, radiation safety, and so on, that can increase the patient safety, but also your safety.
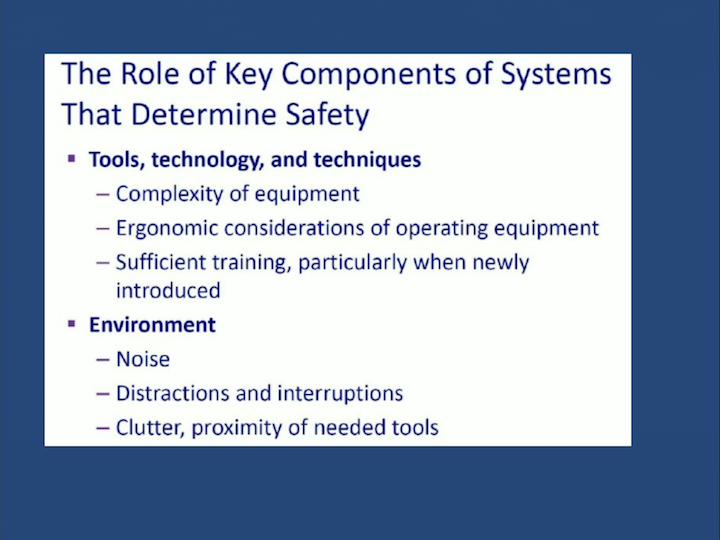
The Role of Key Components of Systems That Determine Safety
And the key role components that determine safety is how you use your tools, technology. Ergonomics is very important for you also, because if you’re having anesthesia because of a C-spine, your ergonomics is important. The environment: if you can not operate with rock music, don’t do that. But, you’ve got to align with your organization. Talk with your patient safety. Get to know that guy that wears the patient safety hat in your organization, makes financial decisions, tell them that it’s not about only money, but now we’re going to value based care. Operational decisions, how many people are we going to cut on this part, that part. And be involved with policies and procedures.
Organization
And we can talk about other things: about SPAR, D-MAC, Toyota LEAN, and Six Sigma that are coming for you to learn about health care. The AUA is preparing a bunch of stuff for urologists to understand and trying to get a different way of thinking, because now you really have to be aware of patient safety to protect yourself. And, it is very important to really align with the organization you work with, because now, I think everybody is an employee of somebody.
ABOUT THE AUTHOR
Fernando J. Kim, MD, MBA, FACS, is president of the South Central Section of the American Urological Association (SCSAUA), editor-in-chief of AUA NEWS in Portuguese, and associate editor of the Journal of Urology Plus and the Patient Safety in Surgery Journal. Dr. Kim previously served at Denver Health Medical Center where he was chief of urology and has also played a pivotal role in enhancing urological resident rotations by serving as the site residency director and significantly enhancing diversity and inclusion. Dr. Kim earned his MD from the University of São Paulo School of Medicine in São Paolo, Brazil. He was a trauma research fellow at the University of Colorado (CU) Health Sciences Center in Denver and completed an internship in general surgery at the CU Health Sciences Center. Dr. Kim also completed general surgery training at Loyola University's Stritch School of Medicine in Illinois and a fellowship in endourology and laparoscopy at the Brady Urological Institute at the Johns Hopkins University School of Medicine in Maryland.
Dr. Kim is active in the AUA as part of their leadership program, served as their host country liaison, and was awarded their Presidential Citation for his international relations and contributions to minimally invasive urological surgery. Dr. Kim served as president of the SCSAUA. He also received the Presidential Juscelino Kubitschek Medal from the Society of Brazilian Urology, the Ernest E. Moore Trauma Award, and the Societá Italiana di Urologia International Guest Recognition.