Guilherme Godoy, MD, MPH, presented “Prostate Cancer Early Diagnosis Screening” during the 23rd Annual Innovations in Urologic Practice on September 14, 2018 in Santa Fe, New Mexico.
How to cite: Godoy, Guilherme. “Prostate Cancer Early Diagnosis Screening” September 14, 2018. Accessed [date today]. https://grandroundsinurology.com/prostate-cancer-early-diagnosis-screening/
Prostate Cancer Early Diagnosis Screening – Summary:
Guilherme Godoy, MD, MPH, details the controversies surrounding the evolving United States Preventive Services Task Force (USPSTF) recommendations on PSA screening. He then emphasizes the need for individualizing risk assessment in clinical decisions-making for prostate cancer.
Abstract:
Particularly in the United States, there has been much controversy surrounding prostate cancer screening. Exacerbating this controversy is the binary analysis of PSA tests, with either a positive or negative result. While the standard cutoff point for these results is 4ng/mL, new proposals argue for a 2.5ng/mL cutoff point. This binary approach leads to unnecessary biopsies, overdiagnosis, and overtreatment that subjects patients to needless side effects.
As a result of these controversies, the USPSTF released a statement in 2008 assigning a grade “D” recommendation to PSA screening. The USPSTF then released an update to this in 20112. These statements had a basis in data from the ERSPC and the PLCO. However, there are many valid criticisms concerning both the trials’ designs and the USPSTF recommendations.
Urologists overall opposed the recommendations, as PSA can be valuable tool for detecting prostate cancer. A multitude of urologic societies responded to the USPSTF recommendations, arguing not to discard PSA altogether. Screening in the PSA-based era lead to fundamental changes in the natural history of prostate cancer. The advent of PSA screening marked a deflection in the projected curve of prostate cancer deaths, as well as mortality rates, from the early 1990s to 2015. Fortunately, the USPSTF revised their PSA screening recommendation to a “C” grade in 2018.
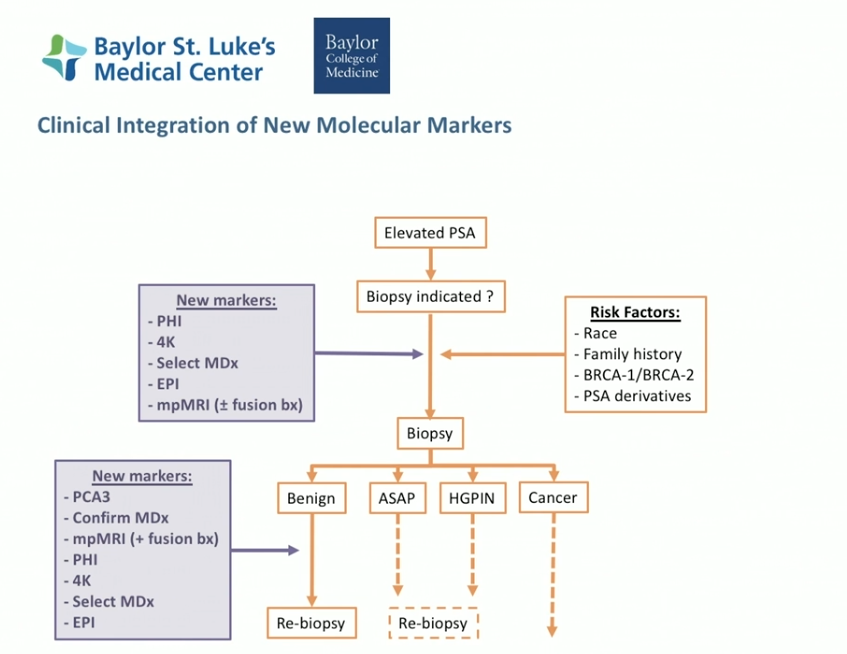
Because overdiagnosis and overtreatment are significant issues, clinicians must be judicial when analyzing PSA. It is important to individualize risks and personalize assessment through approaches such as PSA derivatives and utilizing risk calculators. Urologists currently have access to multiparametric MRI, MRI/ultrasound fusion, new molecular tests, and new PET agents to aid risk-stratification. Integrating these methods into clinical decision-making can ultimately mitigate unnecessary biopsies, overtreatment, and undertreatment without discarding PSA testing.
About Innovations in Urologic Practice
Innovations in Urologic Practice (IUP) is an annual CME-accredited conference devoted to updating urologists on the rapidly changing healthcare environment. Topics focus on innovative diagnostic and treatment strategies, controversies, new and currently developing technologies, and challenges in today’s urologic practice. Dr. Godoy presented this lecture during the 23rd IUP in 2018. Please visit this page in order to learn more about future IUP meetings.
ABOUT THE AUTHOR
Guilherme Godoy, MD, MS, serves as assistant professor of urology at the Baylor College of Medicine (BCM) in Houston, Texas. He joined the faculty of the Scott Department of Urology at BCM in 2012 and has been the chief of the urology service at Ben Taub General Hospital (Harris Health System), since 2017.
Dr. Godoy earned his medical degree from Fundacao Universitaria do ABC in Sao Paulo, Brazil. His training includes an internship and residency in urology at Santa Casa De Sao Paulo in Vila Buarque, Brazil, and a fellowship in urologic oncology at BCM. Dr. Godoy has also completed urologic oncology fellowship training at Vancouver General Hospital, New York University, and Memorial Sloan-Kettering Cancer Center. He earned his MS in clinical investigations at BCM and has remained active in clinical research, translational studies, and clinical trials, mostly focused on prostate, urothelial (upper and lower urinary tract), and testicular cancers.
Dr. Godoy’s expertise includes early diagnosis, minimally invasive approaches (endoscopic and robotic), utilization of molecular and genetic tools for personalized decision-making, management of hereditary cancers, and surgical management of complex/large genitourinary (GU) tumors. His clinical areas of interest include adrenal and kidney tumors, urothelial cancers (upper and lower urinary tract including ureter, renal pelvis, bladder, and urethra), prostate cancer, penile cancer, and testicular and paratesticular cancers. Dr. Godoy also specializes in the utilization of intestinal segments for urinary tract reconstructions, and coordination of multidisciplinary approaches to manage complex intra-abdominal, retroperitoneal, and pelvic tumors. Dr. Godoy is responsible for and moderates the GU Tumor Board Meetings at Baylor St. Luke’s Medical Center as well as the St. Luke’s International GU Tumor Board Meetings.