Steven P. Rowe, MD, PhD, presented “Prostate Cancer Initial Staging and Evaluation of Recurrent Disease with PSMA-Targeted PET” during the 4th Global Summit on Precision Diagnosis and Treatment of Prostate Cancer on October 3, 2019 in Boston, Massachusetts.
How to cite: Rowe, Steven P. “Prostate Cancer Initial Staging and Evaluation of Recurrent Disease with PSMA-Targeted PET” October 3, 2019. Accessed Apr 2025. https://grandroundsinurology.com/current-and-emerging-role-of-radiogenomics/
Prostate Cancer Initial Staging and Evaluation of Recurrent Disease with PSMA-Targeted PET – Summary:
Steven Rowe, MD, PhD, gives an overview of current data on prostate-specific membrane antigen (PSMA)-targeted PET imaging for initial staging of prostate cancer (PCa) and evaluation of recurrent disease. He emphasizes PSMA’s limited sensitivity for initial diagnosis and high sensitivity for recurrent disease, while also noting potential strengths and weaknesses of PSMA that are independent of sensitivity.
Abstract
PSMA-targeted PET is a promising new imaging tool for PCa and the subject of a significant body of recent research, although much remains to be learned about it. Transmembrane carboxypeptidase is highly expressed on PCa cells and has been observed in more than 95% of PCa tumors. There is also a direct correlation between expression levels and tumor aggressiveness. Therefore, it is a good target for imaging. So far, most researchers looking at PSMA have used gallium-68 (68Ga) labeled PSMA, although fluorine-18 (18F) labeled PSMA may also be useful.
In the area of staging PCa, the scope of PSMA-PET’s utility is not yet clear, and it appears to have some limitations. For instance, 68Ga-PSMA uptake does not correlate with Gleason score, and while there is a trend toward higher uptake with higher-grade tumors, it does not reach statistical significance. Therefore, there is no clear cut-off where someone has clinically significant disease and where someone does not. However, using PSMA-PET with MRI does improve diagnostic accuracy. When looking outside of the prostate, PSMA has a high level of specificity for occult nodal metastatic disease, but some researchers have found its sensitivity to be as low as 33.3%. Other researchers have found PSMA to have a level of sensitivity between 60 and 70%, perhaps due to having more skilled readers.
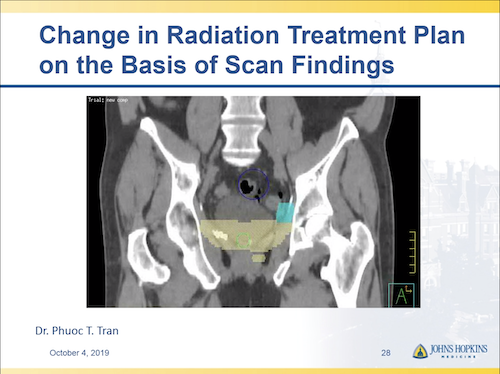
PSMA-PET has also proven to be excellent at finding sites of recurrent disease, even in patients with low-serum PSA, and can have a demonstrable effect on treatment plans. PSMA-directed radiation therapy allows for 100% local control of treated sites and a drop in PSA. Questions remain, however, regarding whether it is necessary to catch and treat all oligometastases, and systems also need to be put in place to make sure urologists are not getting false positives with PSMA and treating unnecessarily.
About The 4th Global Summit on Precision Diagnosis and Treatment of Prostate Cancer:
The Global Summit on Precision Diagnosis and Treatment of Prostate Cancer is a multi-day, multi-disciplinary forum dedicated to informing healthcare stakeholders about topics including in-vitro fluid- and tissue-based molecular diagnostics, novel observation strategies such as active surveillance, and novel therapeutic interventions. Along with this forum’s efforts to form a consensus on the future of prostate diagnostics and precision care, it aims to create an educational and research strategy for its realization. Dr. Rowe presented this lecture during the 4th iteration of this Summit in 2019.
ABOUT THE AUTHOR
Steven P. Rowe, MD, PhD, is an Associate Professor of Radiology and Radiological Science at Johns Hopkins University in Baltimore, Maryland. He clinically practices both diagnostic radiology and nuclear medicine, and his research work focuses on applications of novel molecular imaging agents for positron emission tomography (PET) and single-photon emission computed tomography (SPECT). He is particularly interested in the use of prostate-specific membrane antigen (PSMA)-targeted PET agents in prostate cancer and renal cell carcinoma, as well as the clinical utilization of 99mTc-sestamibi SPECT for non-invasive characterization of renal masses. He and his colleagues recently developed and validated a structured reporting system for delineating and codifying findings on PSMA PET known as PSMA Reporting and Data System (PSMA-RADS).
