Ryan P. Terlecki, MD, FACS, presented “Association of BHP with Overactive Bladder: The Plumbing or the Pump?” during the 26th Annual Perspectives in Urology: Point-Counterpoint, November 10, 2017 in Scottsdale, AZ
How to cite: Terlecki, Ryan P. “Association of BHP with OAB: The Plumbing or the Pump?” November 10, 2017. Accessed Oct 2025. https://grandroundsinurology.com/prostate-physiology-diseased-organ
Summary:
Ryan P. Terlecki, MD, FACS, discusses concomitant treatments of overactive bladder and benign prostatic hyperplasia (BPH), properly diagnosing sources of lower urinary tract symptoms (LUTS), and when it is appropriate to order urodynamics for a patient.
Association of BHP with Overactive Bladder: The Plumbing or the Pump?
Edited Transcript:
Matt T Rosenberg has a fantastic talk, “How to Differentiate the Causes of Lower Urinary Tract Symptoms,” that overlaps with what I’m talking about now. If you listen to that first, you’ll have a better understanding of this lecture. To cite Alan Wein’s metaphor about storage and emptying, I tell patients that the bladder can be a pump, the plumbing, or a combination thereof. A lot of times, I’ll use the analogy of a water pump, like in a car. In this analogy, the prostate would be the hose clamp. I try to use as many automotive analogies as I can, coming from Detroit. They really help when trying to grasp these concepts.
Quickly, here are the objectives for this lecture. I’ll go over some of the data showing the relationship between BPH and overactive bladder, the urodynamic data, and the symptomatology. We’re going to review some outcomes data based on combination therapies, or concomitant pharmacological treatment of OAB and BPE. Lastly, we’re going to discuss the rate of persistent dysfunction after surgical therapy, because I know that can frustrate a lot of us in practice.
Pre-Test Your Knowledge:
Question 1) For the male presenting with lower urinary tract symptoms, all of the following are reasonable triggers to order urodynamic evaluation EXCEPT:
- Post-prostatectomy SUI
- Urge incontinence
- Age below 40
- Age above 80
- Multiple sclerosis
Most people in the audience chose D, age greater than 80. Well, we’ll see if I can change their minds by the end of this lecture.
Question 2) Compared to controls, bladder histology among men undergoing TURP shows all the following EXCEPT:
- Higher rates of CIS
- Increased type I collagen
- Increased type III collagen
- Increased M2 receptors
- Increased M3 receptors
Almost everybody in the audience chose A, higher rates of CIS. Well, they can’t all be hard questions.
You’ve probably already heard the definition of overactive bladder (OAB), with or without incontinence.
There’s a clear overlap of OAB symptoms with male LUTS symptoms. If you look at men with bladder outlet obstruction, the majority of them have OAB. Not just some of them, the majority of them. While women are more likely to express urge incontinence in the setting of OAB, men are more likely to suffer from urgency, frequency, and nocturia.
I think the point of Matt’s talk, about considering other solutions, especially those that don’t involve giving medication, is very important. I think time voiding is important. Nowadays, I diagnose a lot of pelvic floor dysfunction cases. A lot of times, I’ll see patients with nocturia, which is a very bothersome symptom, and diagnosed them with cases of sleep apnea.
In North Carolina, like many other states, there is an obesity epidemic. When I’m there, a ton of people come into my clinic. If a patient is with his wife, I ask his wife, “Does he snore?” She will answer, “Oh, yeah, it’s terrible. I push him over on his side.” In those cases, they can’t tell whether they’re waking up because they have to urinate, or they’re urinating because they’re waking up so frequently. This could be related to oxygen.
When I try to explain the theory behind increased urine production at night to patients, I ask them, “When you’re making that snoring noise, what do you think is happening? What’s causing that noise?” Then, I’ll explain that, with obstructive sleep apnea, their tongue is falling back. They’re blocking their own airway. Then, I say, “Well, how do you take a breath?” A lot of the men I see are hunters. They know what the diaphragm is.
So, I go on to explain that the diaphragm contracts, creating negative pressure and a vacuum in your chest. If you’re blocking the flow of air that is supposed to satisfy that vacuum, and offset that negative pressure, what’s the only thing left in your chest to puff out or expand? Eventually, the patients will figure out the answer – which is the heart. This situation can mimic CHF.
Anyway, with sleep apnea, the stretch receptors releasing ANP, or atrial natriuretic peptide. Then, the ANP dumps sodium into your bladder, and water’s going to follow. So, make more urine at night. Because of that, I end up ordering a lot of sleep studies.
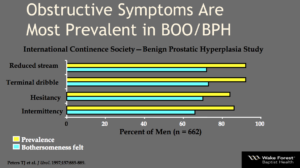
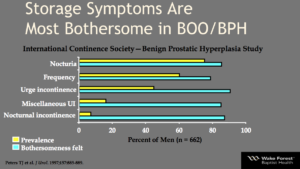
Let’s not get too far off-topic. Now, we usually categorize LUTS between storage symptoms and voiding symptoms. But, we should also keep post-voiding symptoms in mind. They are also important for a lot of guys. People don’t like having that dribbling after they walk away, especially if they’re not wearing a pad. The majority of men and women with OAB deal with storage symptoms, such as frequency, urgency, nocturia, and UI. Voiding symptoms, such as slow FOS, split stream, intermittency, hesitancy, and straining, tend to run a bit higher in men, as you can imagine, because we have prostates, and some men may have urethral disease.
Post-void dribbling can be very bothersome. If you’ve maximized your medical therapy, or even surgical therapy of the prostate, that last bit of urine that leaves the bladder doesn’t have enough momentum behind it. It can’t get through the curve of the bulbourethra, then up and out through the penis. That’s when we start to talk about perennial milking, or basically pressing and sweeping forward to get that last bit out while the man is still standing or sitting to urinate, before he goes on his merry way.
So, we’ve talked about the pump and the plumbing, or the detrusor and outlet in male LUTS. Now, we often see alpha blockers prescribed first line. Also, 5 ARIs are still prescribed pretty heavily. However, a lot of men will still have symptoms on those medications. OAB meds tend to be used less in men than in women, because of fear of retention. This is despite the similar prevalence of storage LUTS in women. Numerous placebo controlled trials have shown that antimuscarinics and drugs like Myrbetriq, either alone or in combination, improve storage symptoms without negatively impacting your maximum flow, your residual, or your chance of retention.
LUTS and BPH both increase with age. But, it’s important to point out that, while voiding symptoms may be more common, the storage symptoms can be more embarrassing. When Matt imitated the dance to get to the bathroom at the airport – that is a situation people with storage symptoms experience often. This is a quality of life issue. A lot of guys will come into my clinic with urgency as as their main symptom. A lot of those men will be taking alpha blocker due to the perception that benign enlargement is the cause. But two-thirds of those men still have bothersome symptoms.
However, if you look at what’s most bothersome, incontinence, nocturia, frequency prove to be the worst symptoms.
What about urodynamics?
When should you order urodynamics for your patient? You don’t have to order this on everybody. It’s not routine first line for men with urinary symptoms. You don’t need to set them up with an invasive study. There is no pre-op randomized trial for patients using urodynamics for their BPH. The results poorly correlate with clinical OAB, anyway.
We see detrusor overactivity in about 50% of OAB cases. That presence is larger when you look at cases where urge urinary incontinence is present, or in other words, you observe spasms and contractions. Severe urgency appears to be a negative predictor for obstruction. Urodynamics appears to be indicated in the setting of urge incontinence in men, in extreme ages of either over 80 or less than 40 (because you want to be careful about operating on someone who’s an octogenarian or higher), and in possible neurological disease patients. Those include Parkinson’s patients, MS patients, and even advanced diabetics with extreme neuropathy.
What about after TURP?
Older data suggests that there’s a 20% persistence of OAB symptoms following TURP. Recent data, taken from 1-year post-op outcomes, suggests older patients and those with a capacity less than 250 cc see worse outcomes. These patients have over 83% persistence of symptoms at 1 year. That’s a lot.
The GOLIATH study showed that OAB symptoms improved similarly, whether patients were treated with laser vaporization or TURP. I know a lot of people are concerned with laser vaporization and its irritative symptoms. In the long-term follow-up, there didn’t seem to be a significant difference between the two treatments.
In terms of OAB pathophysiology, we mostly draw our understanding from animal studies. First, obstruction can lead to overactivity and decreased compliance. Initially, there is smooth muscle hypertrophy. Later, collagen increases within the bladder. We see so many trabeculated bladders because of these extra bundles of collagen.
Next, big potassium channels decrease. Some data suggests that ischemic-induced changes happen in response to neurotransmitters. The nitric oxide pathway becomes implicated. We can relate that to daily Cialis and the value of nitric oxide.
When we’ve compared bladder histology between patients undergoing TURP versus control patients, we’ve seen collagen I, collagen III, and both M2 and M3 receptors increase in TURP patients.
Why is this important?
Only half of the men that have pre-operative detrusor hyperactivity will have resolution after TURP. 20% to 30 % of men have resolution after simple prostatectomy. This data becomes important when you’re trying to set expectations for your patients in the office and they ask, “Am I going to be fixed after this, doc?”
Now, let’s talk about traditional medical therapy.
How much does the prostate shrink with drugs like finasteride? That question stumps some of my residents. The answer is that it shrinks 15% after 6 months.
One of my partners, John McConnell, was involved with the MTOPS trial. We reviewed that data together. The drugs from the trial, statistics aside, were not great. They didn’t cause a lot of improvement. What’s more important, statistical significance or clinical relevance?
PDE5 inhibitors, or the daily Cialis, seem to work well when you look at the data from voiding studies, but it’s not well studied for storage symptoms. When the MTOPS trial looked at improvements in symptom scores, they didn’t differentiate between voiding and storage, so we don’t know what those improvements affected.
We’re well aware of the medical therapy options for OAB. Botox is a big one. There is one beta-3 agonist option. Then, there are numerous antimuscarinics, which, for the most part, are fairly similar to each other.
In the past, it was considered blasphemous to prescribe an antimuscarinic for an older gentleman who had urinary symptoms. Around the time this was the case, I was a resident. Tim Boone was a visiting professor. He told me that he kept a $20 bill in his office for any resident that put a man into retention with a starting dose of an OAB med. Apparently, that money had been sitting in his office for quite some time, collecting dust.
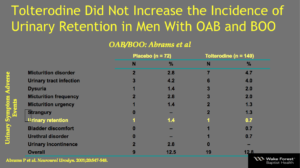
Detrol, or tolterodine, in urodynamic-proven bladder outlet obstruction did not significantly alter the maximum flow, or the voiding pressure, compared to placebo. However, It did improve the volume to first contraction and the capacity. The PVR did go up, which scares a lot of us. It went from 0 to 25. But, that was not considered meaningful. The only retention case in that study, which was done by Sender Herschorn, by the way, was in the placebo arm.
Similar studies have been done, this one by Abrams. Here, you can see that patients were split 2:1 in terms of who received the drug versus the placebo. The adverse event rate was so low. There was one episode of retention in each group, which was not significant at all.
What about antimuscarinic monotherapy?
We rarely do a great job at dialing back medications. Think about polypharmacy in older folks. Once they are on a medication, it seems like they are on it for good, right? We doctors just add something more, and something more, and something more. If we were to really sit down and look at all the medications an older patients is taking, we might question the necessity of a few of them. For example, perhaps some of these men never needed the 5 ARI. Maybe they didn’t need the alpha blocker. Maybe that 5 ARI or alpha blocker could help in conjunction, but what if the patient could’ve gotten by and been satisfied on one medication?
Well, the risk of anticholinergics is less than 1%. The most commonly prescribed drug is oxybutynin, because it appears to be the cheapest, and formulary coverage is favorable.
Moving on – Myrbetriq, the beta-3 agonist, can be a bit tougher to get approved. Myrbetriq comes in 25 mg and 50 mg. Vic Nitti looked at studies showing some improvement when Myrbetriq was involved, but the results weren’t stratified by gender in each analysis. He did perform a placebo control trial in 200 men, in which urodynamics showed non-inferiority to placebo. But, the trial didn’t evaluate storage LUTS. Myrbetriq isn’t a “home-run” treatment. It’s more of a “base-hit” improvement.
A recent analysis of five phase III studies showed that Myrbetriq 50 was better than placebo for frequency. This was called the BEYOND trial. Similar improvements were seen in urgency, frequency, and urgent incontinence, as compared to solifenacin, which is also marketed as VESIcare.
What about antimuscarinic and alpha blocker combination therapy?
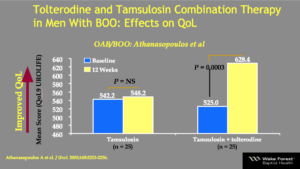
Several studies have looked at this. They showed a tolterodine and alpha blocker combination improving quality of life, while tamsulosin, or Flomax, by itself did not show these improvements. The combination also showed improvements in flow, voiding pressures, and symptom score, and had little to no chance of retention. You will find similar results when you use Flomax with solifenacin or darifenacin, which is marketed as Enablex, I believe.
Here is a study looking at that tolterodine and tamsulosin combination. It is from one of our Greek colleagues, Athanasopoulos. The study used a questionnaire to assess quality of life and looked at 25 men in a tamsulosin group and 25 men in a tolterodine and tamsulosin group, then compared baseline data to results after 12 weeks. Flomax alone did not show not significant change in terms of quality of life. However, if you give patients the combination, there was a significant improvement. That’s what we want. We want happy patients.
Now, let’s look at Meta-analyses. Hao et al reviewed 18 randomized trials, with 1978 men on just alpha blockers and 2106 men on the combination therapy. In this case, the combination therapy wins. There were significant improvements in the symptom score, quality of life, number of times the patients voided in 24 hours, and urgency episodes, without any significant differences in flow, total score, or voiding.
Another meta-analysis, Gong et al, compared Flomax alone versus a Flomax and VESIcare or solifenacin combination. In 7 studies with over 3,000 men, again, combination therapy won, with similar adverse events. Episodes of retention were rare. Therefore, there were no clinically significant changes and no significant drop in maximum flow rates.
Who is a good candidate?
Some suggest good candidates already have a good flow, predominantly storage symptoms as opposed to other LUTS, and a residual less than or equal to 50. You want to use some caution with antimuscarinics in the elderly. Why is this? It is because of the changes, especially in cognition, dry mouth, and constipation, that can be bothersome. There was marketing for Sanctura, which is the name brand for trospium, that is somehow a quaternary amine. Sanctura might be safer and involve less crossing of the blood-brain barrier. But, it’s still lumped in with the anticholinergics.
Beta-3 may also be better than antimuscarinics. Insurance companies might not cover beta-3 if the patient hasn’t failed with other drugs before, though. Also, more data is needed. Initial trials showed that beta-3 could cause a 2 or 3 point rise in systolic blood pressure, which doesn’t sound like a whole lot. Still, because of that, beta-3 is not recommended if patients have severely uncontrolled hypertension.
Botox is another option to consider. I’ve certainly used neuromodulation in the past in men, when I was in fellowship. Those results weren’t great when you compare them to the results in women. The results weren’t great, either, if the patient’s main complaint was retention, as opposed to overactivity. Other options are NSAIDs and analgesics, depending on the case.
Test What You Have Learned:
Question 1) For the male presenting with lower urinary tract symptoms, all of the following are reasonable triggers to order urodynamic evaluation EXCEPT:
- Post-prostatectomy SUI
- Urge incontinence
- Age below 40
- Age above 80
- Multiple sclerosis
Excellent, most people in the audience chose A, post-prostatectomy SUI. That is correct.
Question 2) Compared to controls, bladder histology among men undergoing TURP shows all the following EXCEPT:
- Higher rates of CIS
- Increased type I collagen
- Increased type III collagen
- Increased M2 receptors
- Increased M3 receptors
Everybody aced this question the first time, but I wanted to make sure people didn’t get less intelligent by hearing me speak. Everybody chose A, higher rates of CIS, this time around, which is correct, so I guess I didn’t.
In conclusion, treat the most bothersome symptoms first, if that’s why a patient has come to you. That applies if you’re talking about overactivity, as opposed to retention. If they’re in a critical situation, that’s a little bit different. Alpha blockers are a good first choice for voiding symptoms, but you should consider antimuscarinics when the storage symptoms predominate. This is included in the EAU guidelines. Both monotherapy and combination therapy within antimuscarinics are accepted options in men with storage LUTS.
The adverse event rate, especially that of acute urinary retention, of using these drugs in BPH is low. There is minimal negative impact on the urodynamic parameters, as I mentioned multiple times. More research is still needed when it comes to beta-3. Don’t be afraid to try to take men off some of these drugs if they’re eligible. Thank you.
ABOUT THE AUTHOR
Ryan P. Terlecki, MD, FACS, is a reconstructive urologist for Atrium Health Wake Forest Baptist Medical Center, an academic Level 1 trauma center in Winston-Salem, North Carolina. Dr. Terlecki holds the rank of Professor and the title of Vice Chair of Research for the Department of Urology. In addition, Dr. Terlecki is Director of the Men’s Health Clinic, Director of Medical Student Education, and Fellowship Director for Reconstructive Urology. He holds a joint appointment in the Department of Obstetrics and Gynecology.
Dr. Terlecki earned his medical degree from Wayne State University School of Medicine and completed residency in general surgery and urology at Detroit Medical Center. Following his residency, Dr. Terlecki completed two separate fellowships in reconstructive surgery. He completed a fellowship at the University of Colorado’s Denver School of Medicine and at UT Southwestern Medical Center in Dallas, Texas.
Dr. Terlecki’s publications cover multiple areas of trauma and reconstruction and his research is focused primarily on models of wound healing and regeneration in the lower genitourinary system. Dr. Terlecki’s areas of expertise include urethral stricture disease, male sexual dysfunction, male incontinence, Peyronie’s disease, chronic testicular pain, hypogonadism, and infertility. He is a member of the Society of Genitourinary Reconstructive Surgeons (GURS), a member of the American Urological Association (AUA), and past president of the North Carolina Urological Association (NCUA).