Contemporary Brachytherapy: A View from the ABS
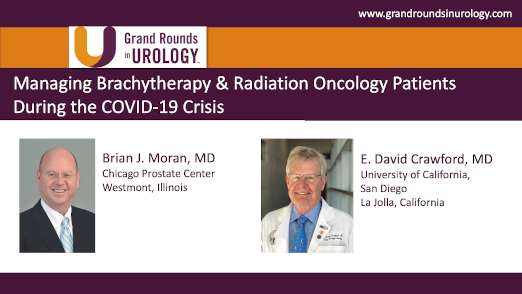
Brian J. Moran, MD, the Medical Director for the Chicago Prostate Cancer Center and the Director of Radiation Oncology at DuPage Medical Group, outlines how improved diagnostics have led to better-targeted brachytherapy treatment for localized prostate cancer. He begins by asserting that the debate is over—low-dose rate (LDR)/high-dose rate (HDR) brachytherapy is an effective treatment for localized prostate cancer, and he argues that the focus should shift to innovative brachytherapy techniques. Dr. Moran explains that improved diagnostics such as MRI and fusion biopsy, transperineal mapping biopsy, and genomic analysis allow urologists to better differentiate cancer types and better understand risk groups. He then presents the American Brachytherapy Society guidelines for various treatment groups. Despite this, Dr. Moran cites a decline in the use of brachytherapy due to competing treatments such as robotic surgery, intensity-modulated radiation therapy (IMRT), and proton therapy and due to low active brachytherapy volumes in most training programs in the United States. Dr. Moran says there is robust patient demand for brachytherapy because it offers patients a single-treatment option vs. nine weeks of external-beam radiation therapy (EBRT) or surgery, producing excellent patient outcomes while maintaining quality of life. Dr. Moran differentiates LDR and HDR brachytherapy and then reiterates the importance of urologists being able to understand the precise location of a malignancy and to target therapy to that location, highlighting a book, Focal Therapy in Prostate Cancer. Dr. Moran expounds on this notion by contrasting transperineal prostate mapping biopsy (TRPB) with stereotactic transperineal prostate biopsy (STPB), asserting that, unlike TRPB, STPB allows doctors to map the precise location of the samples taken. Dr. Moran then outlines methods of focal brachytherapy and identifies which patients are candidates for it, including those with low-risk, low-volume disease; intermediate-risk, low-volume disease; and high-risk, low-volume disease, provided it was accurately identified. Dr. Moran asserts it would be irresponsible for urologists not to explore brachytherapy, citing patient demand, low cost, and efficacy. He concludes by addressing recurrence and treatment options for previously-treated focal brachytherapy patients who may develop a new cancer.
Read More