Michael S. Cookson, MD, MMHC, presented “Debate: Neoadjuvant Chemotherapy Prior to Cystectomy | Con Argument” during the 27th Annual Perspectives in Urology: Point Counterpoint on November 9, 2018 in Scottsdale, Arizona.
How to cite: Cookson, Michael S. “Debate: Neoadjuvant Chemotherapy Prior to Cystectomy | Con Argument” November 9, 2018. Accessed Nov 2025. https://grandroundsinurology.com/mri-in-the-enhanced-detection-of-prostate-cancer-what-urologists-need-to-know/
Debate: Neoadjuvant Chemotherapy Prior to Cystectomy | Con Argument – Summary:
Michael S. Cookson, MD, MMHC, argues that neoadjuvant chemotherapy (NAC) is not appropriate or necessary for all patients with muscle invasive bladder cancer (MIBC) prior to cystectomy. Instead, physicians should use a selective approach to NAC to avoid unnecessary harms, toxicities, and delays in local therapy.
This presentation is the “con” or negative installment of a debate over the use of neoadjuvant chemotherapy prior to cystectomy for MIBC. The rebuttal to this argument is “Debate: Neoadjuvant Chemotherapy Prior to Cystectomy | Pro Argument” by Daniel P. Petrylak, MD.
Abstract:
Level 1 evidence from the SWOG 87-10 trial does demonstrate improved survival with NAC in patients with MIBC undergoing cystectomy. The most dramatic improvement in this study was in patients with locally advanced disease.
However, there is no proven benefit to non-cisplatin based NAC in bladder cancer. This means patients who are ineligible, for reasons such as poor performance status, impaired renal function, or comorbidities, or may not tolerate cisplatin must proceed to cystectomy or seek a clinical trial. Physicians must carefully screen patients for cisplatin eligibility based on consensus factors such as glomerular filtration rate (GFR) and Eastern Cooperative Oncology Group (ECOG) Performance Status.
Currently, European Association of Urology (EAU) guidelines recommend platinum-based NAC for invasive tumors. However, they recommend against NAC when there is a contraindication, and to discontinue NAC in cases of progression.
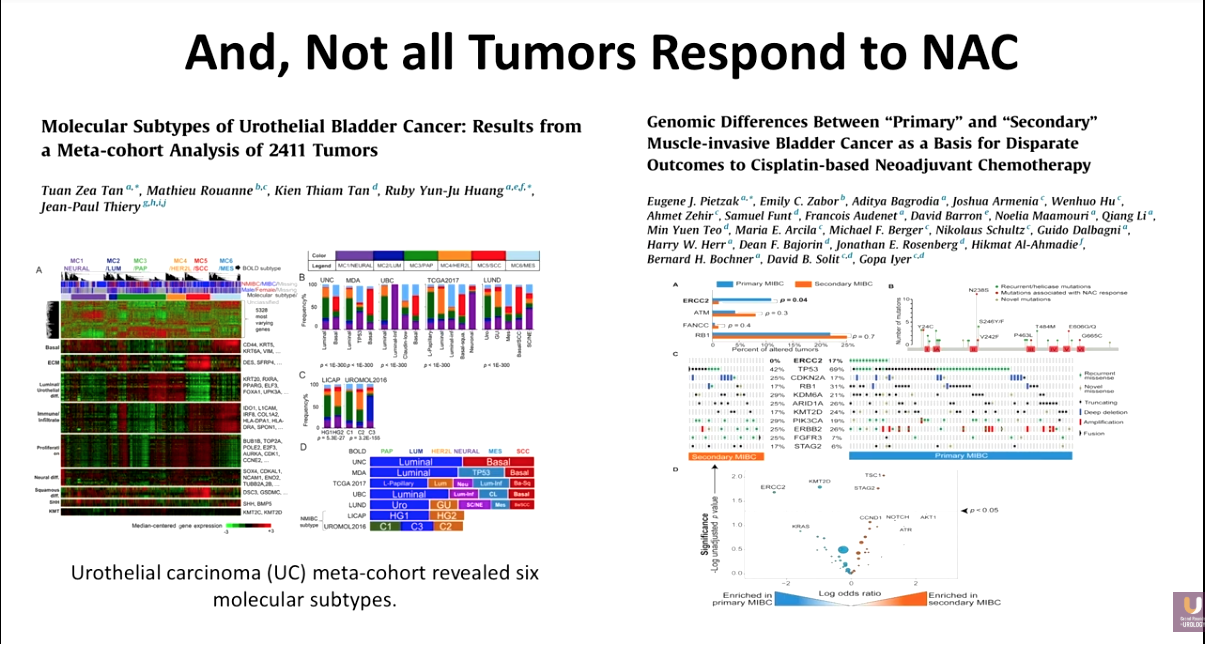
Another drawback of NAC is that not all tumors will respond, as certain molecular subtypes resist platinum altogether, and patients with “secondary,” as opposed to “primary,” MIBC have lower response rates. Furthermore, up to a third of patients undergoing NAC will have Grade 3 and 4 toxicity.
For these reasons, a selective approach to identify patients who will do well with radical cystectomy alone and those who will benefit from NAC is essential. A group from MD Anderson Cancer Center has reported on refining this patient selection process based on clinical risk-factors.
About Perspectives in Urology: Point Counterpoint
Perspectives in Urology: Point Counterpoint (PCP) is an annual CME-accredited conference devoted to discussing and debating the latest topics in men’s health, general urology, and genitourinary cancers. The conference’s format includes more than didactic lectures. It also includes debates, point-counterpoint discussion panels, and unique case-based presentations. Dr. Cookson presented this lecture during the 27th PCP in 2018. Please visit this page in order to register for future PCP meetings.
ABOUT THE AUTHOR
Michael S. Cookson, MD, MMHC, is Professor and Chairman of the Department of Urology and holds the Donald D. Albers Endowed Chair in Urology at the University of Oklahoma Health Sciences Center in Oklahoma City. He has authored some 240 peer-reviewed journal publications as well as more than 30 chapters of various textbooks, and he is nationally recognized for his outstanding contributions to urologic oncology. Dr. Cookson completed his Urology residency at the University of Texas, San Antonio, and completed his Urologic Oncology fellowship at Memorial Sloan-Kettering Cancer Center in New York. From 1998 to 2013, he served as the Vice Chairman of Urologic Surgery and Director of the Urologic Oncology Fellowship Program at Vanderbilt University in Nashville, Tennessee.