Leonard S. Marks, presented “Focal Therapy of Prostate Cancer” during the 24th Annual Southwest Prostate Cancer Symposium on April 13, 2019 in Scottsdale, Arizona.
How to cite: Marks, Leonard S. “Does the PROMIS Trial Impact Prostate Cancer Screening?” April 13, 2019. Accessed May 2025. https://grandroundsinurology.com/focal-therapy-of-prostate-cancer/
Focal Therapy of Prostate Cancer – Summary:
Leonard S. Marks, MD, discusses the response propelling consideration of focal therapy as a treatment option for localized prostate cancer. He reviews evidence on the three currently-FDA approved focal therapy modalities: cryotherapy, high-intensity focused ultrasound (HIFU), and laser ablation.
Abstract:
Focal therapy refers to the removal of cancer tissue within the prostate, sparing the normal tissue and thus reducing the morbidity associated with whole-organ treatment. This method is a direct outgrowth of targeted prostate biopsy, made possible by MRI visualization of localized prostate cancer. Focal therapy is also known as partial gland ablation (PGA). The concept of PGA originated in 2002, and is analogous to lumpectomy for breast cancer. Therefore, it is sometimes known as “male lumpectomy.” Since then, focal therapy has gained great appeal from patients.
Several concepts have propelled consideration of PGA as a treatment option for localized prostate cancer: improved tumor localization ability with MRI; the success of focal therapy in other organs; the limited benefit of radical prostatectomy shown in large, controlled studies; a growing belief in the ‘Index Theory’ of prostate cancer; and patient preferences for a safer treatment than previously available.
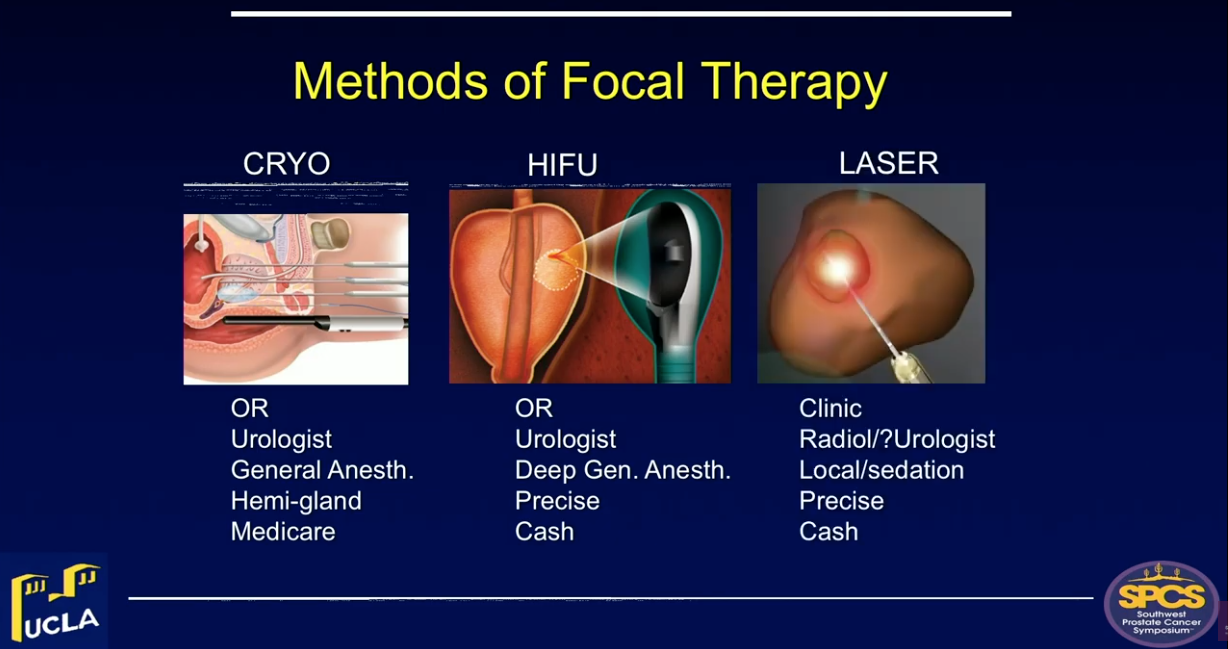
In the United States, there are 3 technologies for prostate PGA that are currently FDA-approved: cryotherapy, high-intensity focused ultrasound (HIFU), and laser ablation.
Cryotherapy is the original focal therapy, and is well-suited to hemi-gland ablation. Ongoing clinical trials generally stipulate that included patients have intermediate-risk disease, tumor confined to one side of the organ, and a prostate volume less than approximately 50-60cc. It is important to maintain active surveillance of patients who receive cryotherapy. Early results of this modality are promising. Additionally, Medicare has covered prostate cryotherapy since 1999.
Another technology option is HIFU, which was approved by the FDA ‘for ablation of prostate tissue’ in October 2015. The utilization of this method appears to be increasing, especially for focal therapy. Treatment with this modality is somewhat complex and time-consuming, requiring considerable operator expertise for optimal results. However, data on focal HIFU from England and Europe, where the procedure has been approved for 15-20 years, indicate it as safe and effective. In the United States, a facility code was issued by Medicare within the past year, leading to a reduction in out-of-pocket costs for patients seeking HFU.
Laser ablation using MRI guidance is currently performed ‘in-bore’ by interventional radiologists, and lacks third party coverage. Follow-up data on this modality is limited.
Issues that need to be addressed in the future regarding prostate focal therapy include the determination of optimal treatment margins; evaluation in clinical trials to prove efficacy and safety; and the establishment of guidelines to address the possibility of over-utilization.
About the Southwest Prostate Cancer Symposium
The Southwest Prostate Cancer Symposium (SPCS) is a multi-day conference that seeks to educate urologists, radiation oncologists, medical oncologists, and other healthcare professionals involved in the treatment of prostate cancer. The topics focus on current technical aspects of diagnosis and treatment of localized and advanced disease, particularly regarding imaging, technology, and training in the related devices. Dr. Marks presented this lecture during the 24th SPCS in 2019. In 2020, the 25th SPCS will also offer training sessions involving imaging, scanning, and prostate cancer treatment-related devices on site. Please visit this page in order to register for future SPCS meetings.
Selected Key References
Guillaumier S, Peters M, Arya M, et al. A multicenter study of 5-year outcomes following focal therapy in treating clinically significant non-metastatic prostate cancer. Eur. Urol., 2019, Article in press online (PMID: 29960750).
625 men in British centers, most with intermediate/high-risk CaP, treated with focal HIFU: 98% metastasis-free survival at median f/u 56 months. 2% Incontinence.
Zhou S, Simopoulos D, Jayadevan R, et al. Use of MRI-Guided Biopsy for Selection and Follow-up of Men Undergoing Hemi-gland Cryoablation of Prostate Cancer. Urology, 2019, Article in press online (PMID: 30659903).
Clinical trial of 29 men with intermediate risk CaP, treated with hemi-gland cryoablation; mandated 6month biopsies (guided by repeat MRI) showed no cancer in 23 (80%).
Fisher B, Anderson S, Bryant J, et al. 20 year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. New Engl.J.Med. 347: 1233, 2002.
Concluding publication of landmark United States trial showing that lumpectomy yields long-term survival about same as radical mastectomy for breast cancer.
Onik G, Narayan P, Vaughan D, et al. Focal “nerve-sparing” cryosurgery for treatment of primary prostate cancer: a new approach to preserving potency. Urology 60: 109, 2002.
First publication suggesting partial gland ablation, purpose being to reduce morbidity of prostate cancer treatment.
Luijtelaar A, Greenwood BM, Ahmed HU, et al. Focal laser ablation as clinical treatment of prostate cancer. World J. Urol. 2019, Article in press online (PMID: 30671638).
A multinational consensus report, concluding that this new U.S. approved modality appears promising and should be tested in clinical trials.
ABOUT THE AUTHOR
Leonard S. Marks, MD, is Professor and inaugural holder of the deKernion Chair in Urology at the David Geffen School of Medicine at the University of California, Los Angeles. He graduated from the University of Texas Medical Branch, where he received his MD with AOA honors and his MA in Physiology in 1969. He served an internship and surgical residency at UCLA/Harbor General Hospital. For the following two years, he served on active duty as Lieutenant Commander in the US Public Health Service. He was named a Post-Doctoral Research Scholar at UCLA School of Medicine in 1973-4. He completed his Urology Residency at UCLA and was a Lecturer in Urology there in 1978, following which he entered private practice in Los Angeles. He re-joined the UCLA faculty full-time in 2009.
While in practice, Dr. Marks founded a non-profit research organization, the Urological Sciences Research Foundation, a 501c3 corporation, to further his academic interests. He became an original AFUD scholar in 1992 for work relating serum PSA levels to prostate histology. He received a Prostate Cancer Foundation (PCF) research award in 2000 for cross-cultural studies of prostate cancer. As an early advocate of multimedia in medical education, he served as Website Editor of Urology for The Gold Journal from 1998-2010. For his work in the scientific evaluation of alternative medicines, he was appointed to committees of the American Urological Association, the National Institutes of Health, and the National Academy of Sciences.
Over the past decade, he has been Principle Investigator of three separate R01 Awards from the National Cancer Institute devoted to targeted prostate biopsy and focal therapy of prostate cancer. He has authored more than 150 scientific publications.