Abstract #005: Molecular Determinants of Outcome for Metastatic Castration-Sensitive Prostate Cancer (mCSPC) With Addition of Apalutamide (APA) or Placebo (PBO) to Androgen Deprivation Therapy (ADT) in TITAN
Felix Y. Feng,1 Shibu Thomas,2 Clemente Aguilar-Bona- vides,2 Michael Gormley,2 Neeraj Agarwal,3 Gerhardt Attard,4 Alexander W. Wyatt,5 Elai Davicioni,6 Deborah S. Ricci,2 Angela Lopez-Gitlitz,7 Julie S. Larsen,7 Simon Chowdhury,8 Kim N. Chi9
1Helen Diller Family Comprehensive Cancer Center, University of California San Francisco, San Francisco, CA; 2Janssen Research & Development, Spring House, PA; 3Huntsman Cancer Institute, University of Utah, Salt Lake City, UT; 4University College London Cancer Institute, London, UK; 5The University of British Columbia, Van- couver Prostate Centre, Vancouver, BC, Canada; 6Decipher Biosciences, Inc, San Diego, CA; 7Janssen Research & Development, Los Angeles, CA; 8Guy’s, King’s, and St Thomas’ Hospitals, and Sarah Cannon Research Insti- tute, London, UK; 9BC Cancer and Vancouver Prostate Centre, Vancouver, BC, Canada
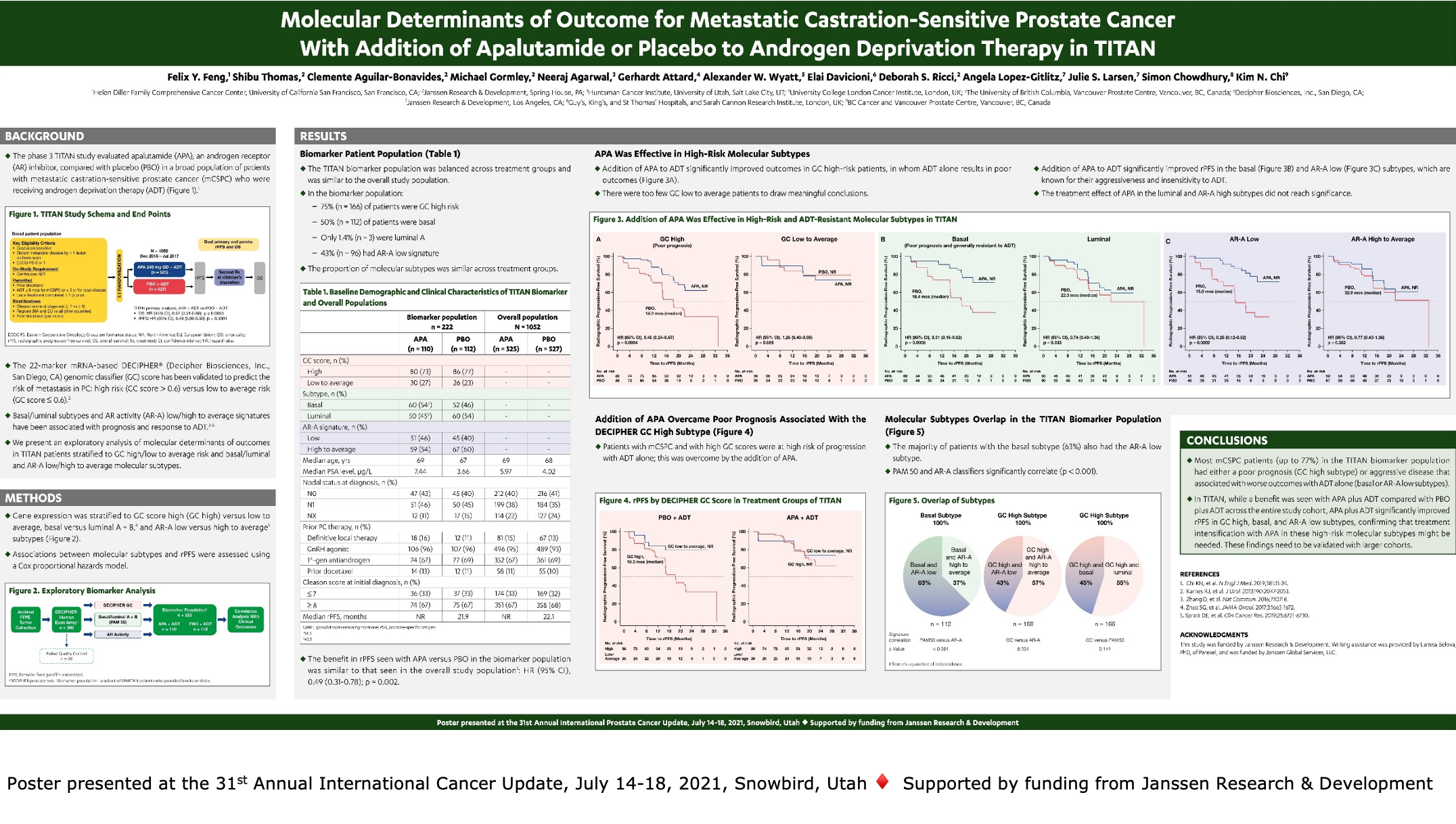
Introduction: In TITAN, addition of APA to ongoing ADT improved radiographic progression-free survival (rPFS) and overall survival (OS) versus PBO plus ADT in patients (pts) with mCSPC. In this post hoc analysis, we performed transcriptome-wide profiling of tumor samples and assessed association of molecular subtypes with rPFS.
Methods: The DECIPHER platform (Decipher Biosci- ences, Inc.) was used to assess gene expression in archi- val primary prostate tumors from TITAN. Samples were classified into high versus low to average risk of metasta- ses (DECIPHER genomic classifier [GC] > 0.6 and ≤ 0.6, respectively), basal and luminal A/B (PAM50 classifier), and androgen receptor activity (AR-A) signature high and low. Associations between subtypes with rPFS were assessed with Cox proportional hazards model.
Results: The biomarker population included 222 pts (APA, 110; PBO, 112). Benefit in rPFS from APA in the biomarker population (HR, 0.49 [95% CI, 0.31-0.78]; p = 0.002) resembled that in the overall study population (0.49 [0.40-0.61]; p < 0.0001). The majority of TITAN pts had GC high scores (n = 166, 75%). GC high risk subtype in the PBO group had poorer prognosis for rPFS than GC low to average risk subtype (median rPFS 18.2 months for GC high vs not reached [NR] for GC low to average, 0.28 [0.11-0.69]; p = 0.006), but there was no difference in prognosis between high and low to average GC risk sub- types in the APA group (GC high NR vs GC low to average NR; 0.81 [0.35-1.89]; p = 0.625). Pts were further strati- fied based on basal/luminal and AR-A signatures. Basal (n = 112, 50%) and AR-A low (n = 96, 43%) subtypes, known to be nonresponsive to ADT, both showed significant ben- efit from APA vs PBO (0.30 [0.16-0.57]; p < 0.001 and 0.25 [0.12-0.52]; p < 0.001, respectively). The majority of AR-A low subtype (74%, 71/96) overlapped with basal subtype. Further conclusions for risk of rPFS in GC low, luminal, and AR-A high subtypes and OS across all sub- types will be assessed as more events occur.
Conclusions: In TITAN, addition of APA to ADT improved rPFS for all subtypes of pts with mCSPC. APA overcame the poor prognosis of GC high risk subtype and prolonged rPFS in ADT-resistant AR-A low and basal molecular subtypes, suggesting APA is beneficial especially for the highest risk molecular subtypes.
Source of Funding: Janssen Research & Development
Registration: ClinicalTrials.gov, NCT02489318
