Abstract #007: Prostate-Specific Antigen (PSA) Kinetics in Patients (pts) With Advanced Prostate Cancer Treated With Apalutamide (APA): Results from the TITAN and SPARTAN Studies
Kim N. Chi,1 Fred Saad,2 Simon Chowdhury,3 Julie N. Graff,4 Neeraj Agarwal,5 Stéphane Oudard,6 Gang Li,7 Angela Lopez-Gitlitz,8 Julie S. Larsen,8 Sharon McCarthy,7 Suneel Mundle,7 Matthew R. Smith,9 Eric J. Small10
1BC Cancer and Vancouver Prostate Centre, Vancouver, BC, Canada; 2Centre Hospitalier de l’Université de Mon- tréal, Université de Montréal, Montréal, Québec, Canada; 3Guy’s, King’s, and St. Thomas’ Hospitals, and Sarah Cannon Research Institute, London, UK; 4VA Portland Health Care System, Portland and Knight Cancer Institute, Oregon Health & Science University, Portland, OR; 5Hunts- man Cancer Institute, University of Utah, Salt Lake City, UT; 6Georges Pompidou Hospital, University René Des- cartes, Paris, France; 7Janssen Research & Development, Raritan, NJ; 8Janssen Research & Development, Los Ange- les, CA; 9Massachusetts General Hospital Cancer Center and Harvard Medical School, Boston, MA; 10Helen Diller Family Comprehensive Cancer Center, University of Cali- fornia San Francisco, San Francisco, CA
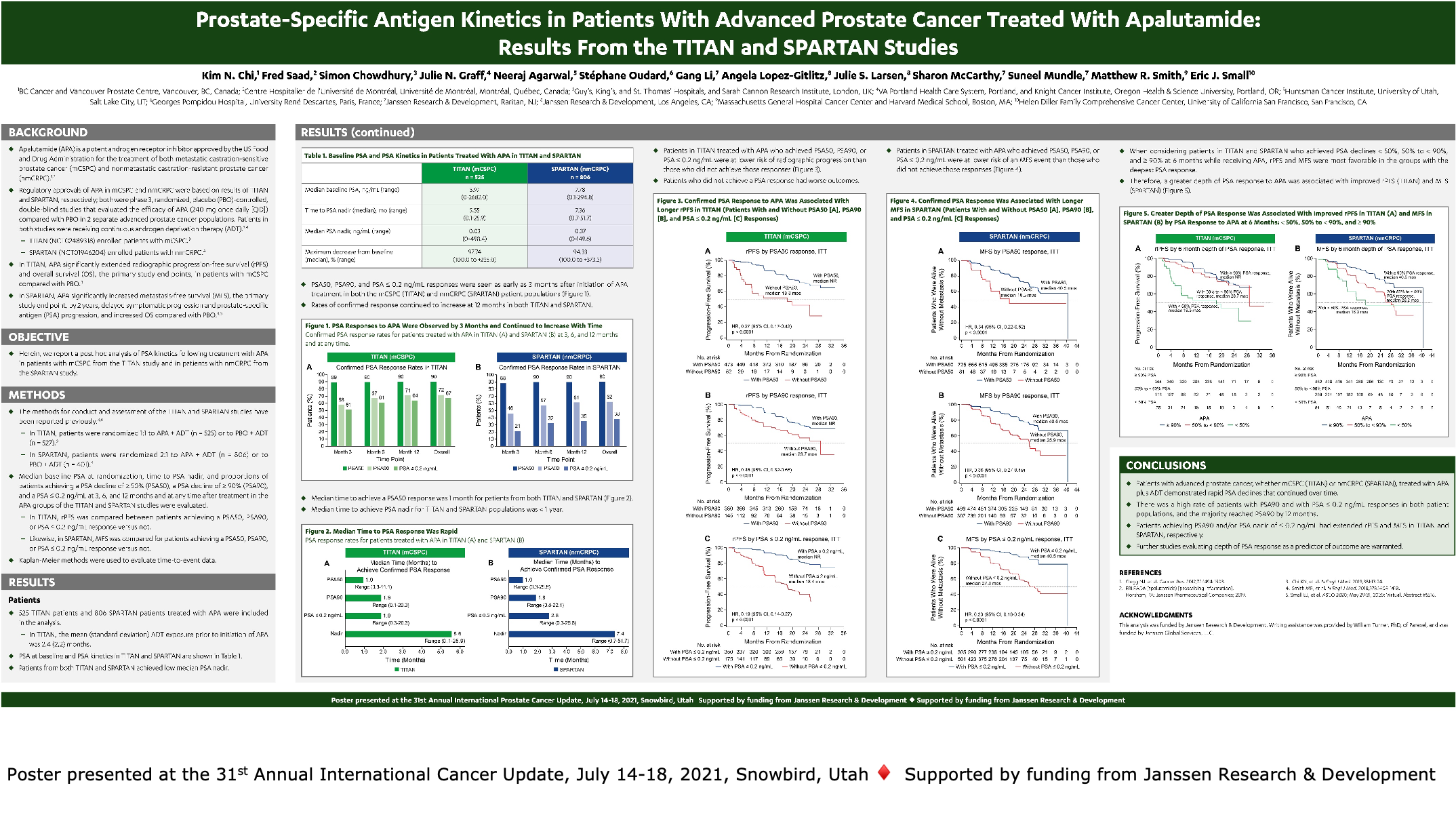
Introduction: The phase 3 TITAN and SPARTAN studies demonstrated improved outcomes with the addition of APA to ongoing androgen deprivation therapy (ADT) versus pla- cebo plus ADT; outcomes included prolonging overall sur- vival and radiographic progression-free survival (rPFS) in metastatic castration-sensitive prostate cancer (mCSPC) in TITAN, and metastasis-free survival (MFS) in nonmetastatic castration-resistant PC (nmCRPC) in SPARTAN. A post hoc analysis of PSA kinetics in pts from both studies is reported.
Methods: Baseline PSA at randomization, time to PSA nadir, and proportion of pts achieving a PSA decline of ≥ 90% (PSA90) and of pts achieving a PSA ≤ 0.2 ng/mL at 3 and 12 months and at any time after treatment in the APA arms of the TITAN and SPARTAN studies were evaluated. Within each study, rPFS/MFS were com- pared between pts achieving a PSA90 or PSA ≤ 0.2 ng/ mL response vs not.
Results: 525 TITAN pts and 806 SPARTAN pts treated with APA were included in the analysis. Median baseline PSA, time to PSA nadir, median PSA nadir, and maximum per- centage changes from baseline PSA are shown in the table. PSA90 and confirmed PSA ≤ 0.2 ng/mL were evident as early as 3 months in both TITAN and SPARTAN, and per- centage of confirmed response continued to increase at 12 months. Pts treated with APA who achieved PSA90 were at lower risk of rPFS events in TITAN and of MFS events in SPARTAN, with a hazard ratio (95% confidence interval) of 0.46 (0.321-0.653) and 0.36 (0.271-0.489) in each respec- tive study (both p < 0.0001), compared with APA pts who did not achieve PSA90. Pts with confirmed PSA ≤ 0.2 ng/mL had similar rPFS and MFS benefits.
Conclusions: Pts with advanced PC, whether mCSPC or nmCRPC, treated with APA + ADT demonstrated rapid PSA declines that continued over time. There was a high rate of pts with PSA90 and with PSA ≤ 0.2 ng/mL responses, with a majority of pts reaching PSA90 by 12 months. Pts achieving PSA90 and/or PSA nadir of ≤ 0.2 ng/mL had a prolonged rPFS and MFS in TITAN and SPARTAN, respectively.
Source of Funding: Janssen Research & Development Registration: TITAN (ClinicalTrials.gov, NCT02489318);
SPARTAN (ClinicalTrials.gov, NCT01946204
|
TITAN (mCSPC) N = 525 |
SPARTAN (nmCRPC) N = 806 |
|
|
Median baseline PSA, ng/mL |
5.97 |
7.78 |
|
Time to PSA nadir (median), mo |
5.55 |
7.36 |
|
Median PSA nadir, ng/mL |
0.03 |
0.37 |
|
Maximum decrease from baseline (median), % |
98 |
94 |
|
90% PSA rate, % 3mo |
58 |
46 |
|
Confirmed PSA ≤ 0.2 ng/mL, % 3mo |
51 |
21 |
