Seth P. Lerner, MD presented “Lymph Node Dissection During Radical Cystectomy – Current State of the Art” during the 23rd Annual Innovations in Urologic Practice on September 14, 2018 in Santa Fe, New Mexico.
How to cite: Lerner, Seth P. “Lymph Node Dissection During Radical Cystectomy – Current State of the Art” September 14, 2018. Accessed [date today]. https://grandroundsinurology.com/lymph-node-dissection-during-radical-cystectomy-current-state-of-the-art/
Lymph Node Dissection During Radical Cystectomy – Current State of the Art – Summary:
Seth P. Lerner, MD, describes the anatomy and stage specific association of lymph node metastasis. He reviews the evidence supporting the anatomic extent of bilateral pelvic lymph node dissection (PLND), specifically the status of current phase III clinical trials investigating extended versus standard PLND.
Abstract:
In 2018, The American Joint Commission on Cancer (AJCC) updated the TNM staging of urinary bladder cancer. Notably, while involvement of common iliac lymph nodes (LN) was a prognostic stage group IV characteristic, it is now a stage group III characteristic. This particularly impacts effect sizes for randomized clinical trials.
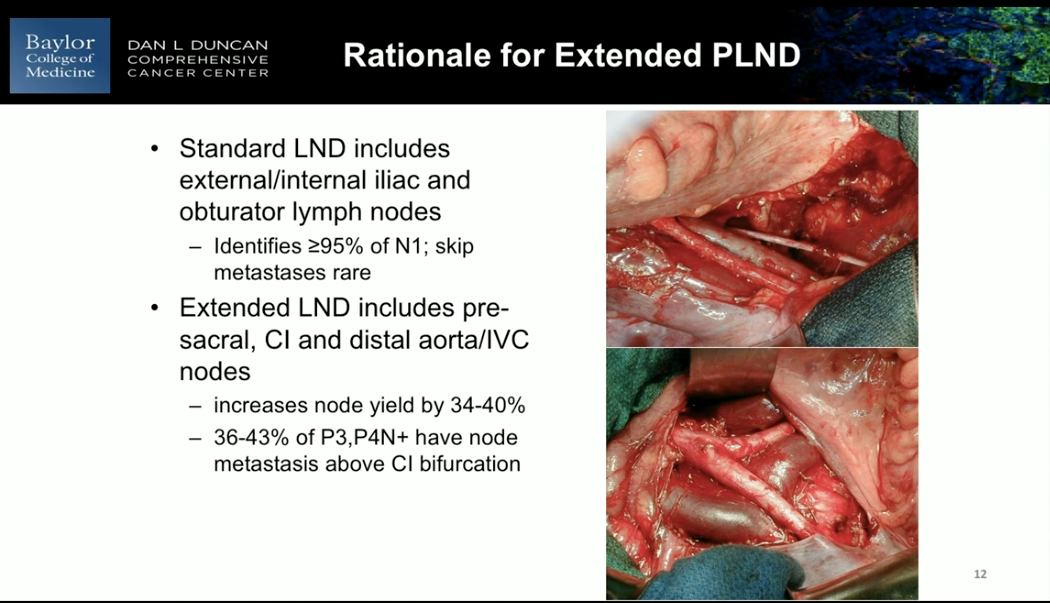
A stage specific lymph node metastasis mapping with bladder cancer undergoing radical cystectomy and PLND showed that of the patients with LN metastatic disease, the majority have multiple metastases, and about 30%-40% have metastases outside the true pelvis. Also, a study by Roth et al. mapped all lymph nodes in bladder cancer patients with a radiotracer. Results showed that PNLD including the extended template resected 92% of all lymphatic landing sites. Conversely, standard PLND resected 81%. Furthermore, data supports that the number of LNs removed correlates with outcomes in both node-negative and node-positive disease. A study testing sensitivity for LN metastasis suggested that extending the proximal limits of PLND, as well as quality of pathological analysis, increases the number of nodes identified and metastases sensitivity.
Clear evidence supports that a thorough PLND at the time of radical cystectomy has a significant impact on the incidence of local pelvic recurrence. Additionally, omitting a PLND leads to a cost in mortality outcomes. Because of these reasons, 2016 American Urological Association (AUA) guidelines and general urologic community supports standard bilateral pelvic lymphadenectomy as standard of care for
surgically curable non-metastatic disease. However, the benefits of extended PLND remains unclear. The completion of two major trials, the LEA AUO AB 25/02 and SWOG S-1011, will provide further data and conclusions regarding the utility of expended PLND.
About Innovations in Urologic Practice
Innovations in Urologic Practice (IUP) is an annual CME-accredited conference devoted to updating urologists on the rapidly changing healthcare environment. Topics focus on innovative diagnostic and treatment strategies, controversies, new and currently developing technologies, and challenges in today’s urologic practice. Dr. Lerner presented this lecture during the 23rd IUP in 2018. Please visit this page in order to learn more about future IUP meetings.
ABOUT THE AUTHOR
Seth P. Lerner, MD, FACS, is Professor of Urology and Vice-Chair for Faculty Affairs in the Scott Department of Urology at the Baylor College of Medicine in Houston, Texas. He holds the Beth and Dave Swalm Chair in Urologic Oncology. Dr. Lerner is the Director of Urologic Oncology and the Multidisciplinary Bladder Cancer Program, also at Baylor.
Dr. Lerner earned his medical degree from the Baylor College of Medicine, completed a surgical internship at Virginia Mason Hospital in Seattle, and returned to Baylor for his residency training. He completed a two-year fellowship at the University of Southern California in Urologic Oncology and Reconstructive Surgery and joined the full-time Baylor faculty in 1992.