Michael S. Cookson, MD, MMHC, presented “MRI in the Enhanced Detection of Prostate Cancer: What Urologists Need to Know” during the 27th Annual Perspectives in Urology: Point Counterpoint on November 9, 2018 in Scottsdale, Arizona.
How to cite: Cookson, Michael S. “MRI in the Enhanced Detection of Prostate Cancer: What Urologists Need to Know” November 9, 2018. Accessed Jan 2026. https://grandroundsinurology.com/mri-in-the-enhanced-detection-of-prostate-cancer-what-urologists-need-to-know/
MRI in the Enhanced Detection of Prostate Cancer: What Urologists Need to Know – Summary:#
Michael S. Cookson, MD, discusses prostate MRI as an upfront assessment for targeting lesions in biopsy naive patients and the conclusion from PROMIS and PRECISION regarding this application. He also reviews the potential applications of MRI in patients with prior negative biopsy and in those on active surveillance.
Abstract:#
Biopsies ordered initially for patients presenting with an elevated PSA are often negative, and transrectal ultrasound (TRUS) biopsies often miss significant cancers. However, a 2017 American Urological Association (AUA) policy statement clearly acknowledges that MRI-guided biopsy and MRI-targeting reduces these failures. Even so, this statement did not recommend routine MRI for every biopsy naive patient due to insufficient evidence.
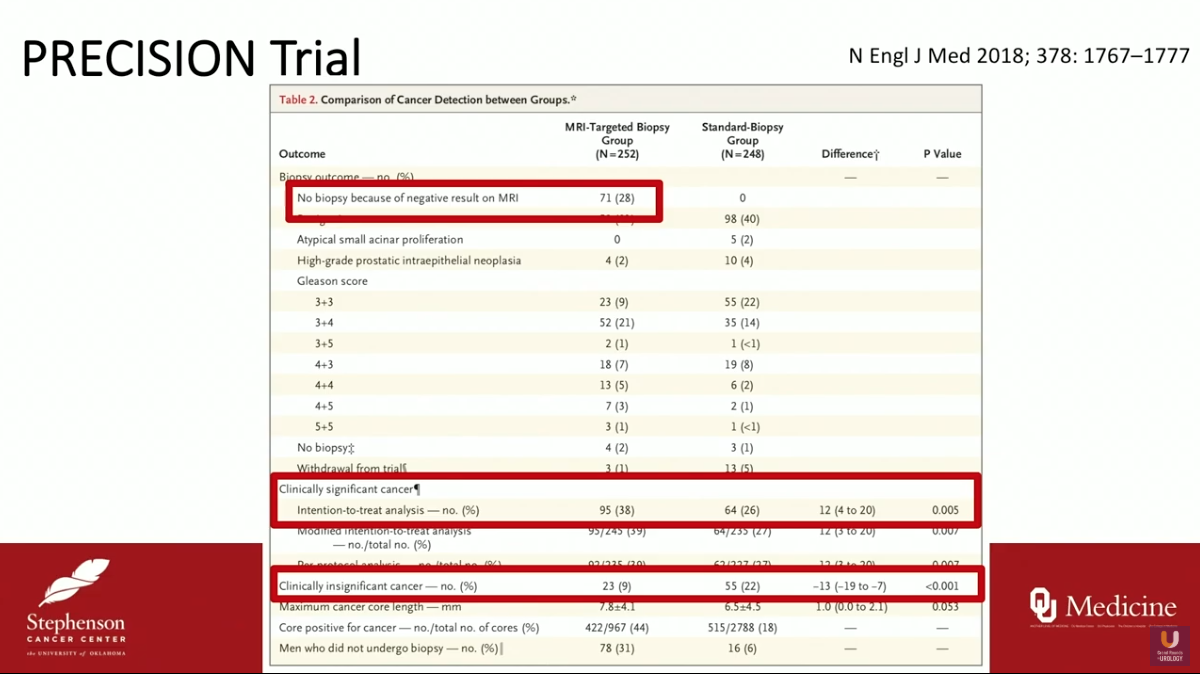
Since then, the PROMIS and PRECISION trials have reported data that is favorable to this application of MRI. In the PROMIS trial, MRI-targeting demonstrated an improved rate of significant cancer detection and a reduction in overdiagnosis of insignificant cancers compared to standard 12-core TRUS biopsy. The PRECISION trial, testing non-inferiority of MRI-targeting to TRUS biopsy, found similar results. Notably, 28% of men in this study avoided biopsy because of negative results on MRI.
Many societies have changed their guidelines in the post-PROMIS and -PRECISION era. For example, the National Comprehensive Cancer Network (NCCN) guidelines on prostate cancer early detection now include consideration of MRI for evaluation before biopsy.
Additionally, there is a rationale for utilizing MRI following prior negative biopsy. As an AUA initiative states, “While blood, urine and tissue based biomarkers may improve patient selection for repeat biopsy, they do not help to improve the diagnostic yield of the biopsy itself. Only imaging has the potential to both improve patient selection and the yield of repeat biopsy.”
MRI could also be a noninvasive monitoring technique for patients on active surveillance. Although there is not yet high-level evidence for this application, it demonstrates favorable detection rates in small cohort studies. The AUA policy statement maintains MRI for active surveillance could be beneficial, but evidence is insufficient for a full endorsement.
About Perspectives in Urology: Point Counterpoint#
Perspectives in Urology: Point Counterpoint (PCP) is an annual CME-accredited conference devoted to discussing and debating the latest topics in men’s health, general urology, and genitourinary cancers. The conference’s format includes more than didactic lectures. It also includes debates, point-counterpoint discussion panels, and unique case-based presentations. Dr. Cookson presented this lecture during the 27th PCP in 2018. Please visit this page in order to register for future PCP meetings.
ABOUT THE AUTHOR
Michael S. Cookson, MD, MMHC, is Professor and Chairman of the Department of Urology and holds the Donald D. Albers Endowed Chair in Urology at the University of Oklahoma Health Sciences Center in Oklahoma City. He has authored some 240 peer-reviewed journal publications as well as more than 30 chapters of various textbooks, and he is nationally recognized for his outstanding contributions to urologic oncology. Dr. Cookson completed his Urology residency at the University of Texas, San Antonio, and completed his Urologic Oncology fellowship at Memorial Sloan-Kettering Cancer Center in New York. From 1998 to 2013, he served as the Vice Chairman of Urologic Surgery and Director of the Urologic Oncology Fellowship Program at Vanderbilt University in Nashville, Tennessee.