Laila E. Woc-Colburn, MD, DTM&H, FACP, FIDSA, presented “Multi-Drug Resistance Bacteria Recent Trends in Uropathogens” during the 23rd Annual Innovations in Urologic Practice on September 14, 2018 in Santa Fe, New Mexico.
How to cite: Woc-Colburn, Laila E. “Multi-Drug Resistance Bacteria Recent Trends in Uropathogens” September 14, 2018. Accessed [date today]. https://grandroundsinurology.com/multi-drug-resistance-bacteria-recent-trends-in-uropathogens/
Multi-Drug Resistance Bacteria Recent Trends in Uropathogens – Summary:
Laila E. Woc-Colburn, MD, DTM&H, FACP, FIDSA, describes the identification and treatment of multi-drug resistant (MDR) Gram-negative infections and the role of Gram-negative bacteria in determining empirical antimicrobial therapy. She also discusses different strategies for treating MDR genitourinary infections.
ABSTRACT:
MDR Gram-Negative Infections
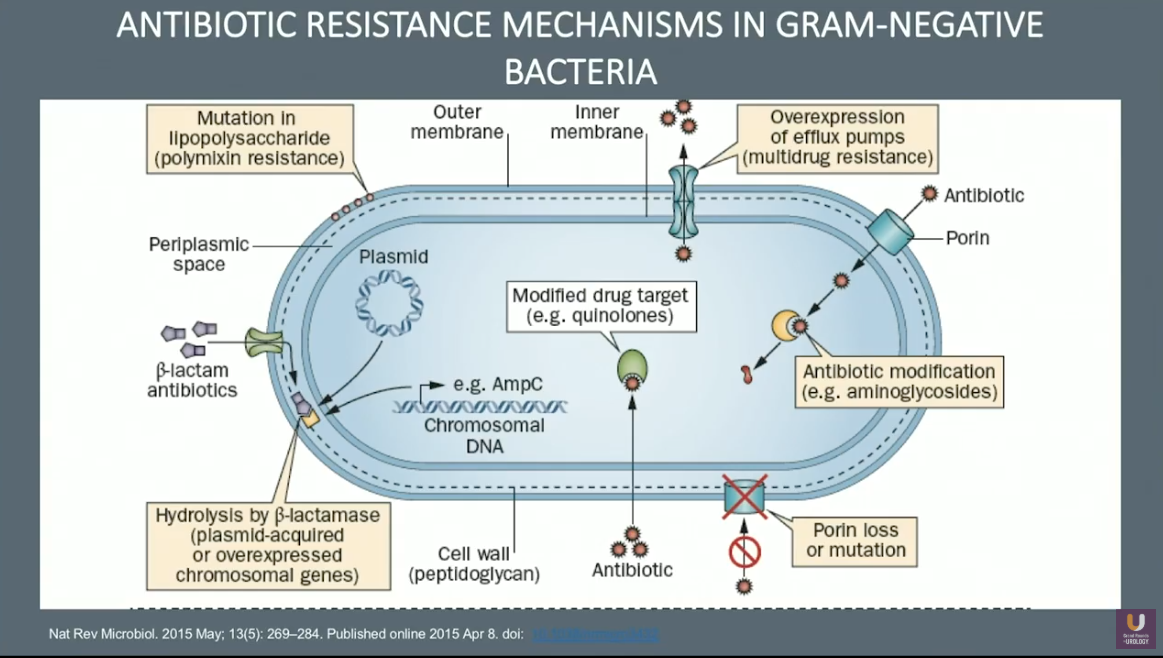
Urinary Tract Infections (UTIs) are one of the most common infectious diseases, affecting people of all age groups and geographical locations. Unfortunately, treating long-term UTIs has become more difficult with the increased prevalence of MDR gram-negative infections. These infections are resistant to one or more of the antibiotics used to treat them, particularly fluoroquinolones and carbapenems.
This often prolongs the infection for the patient and increases the likelihood of recurring infections later in life. Specific culprits include extended spectrum beta-lactamases (ESBL) enzymes, quinolone-resistant Gram-positive and Gram-negative bacteria, and multi-resistant enterococci, which is resistant to vancomycin and aminoglycoside.
Uncomplicated Versus Complicated UTIs
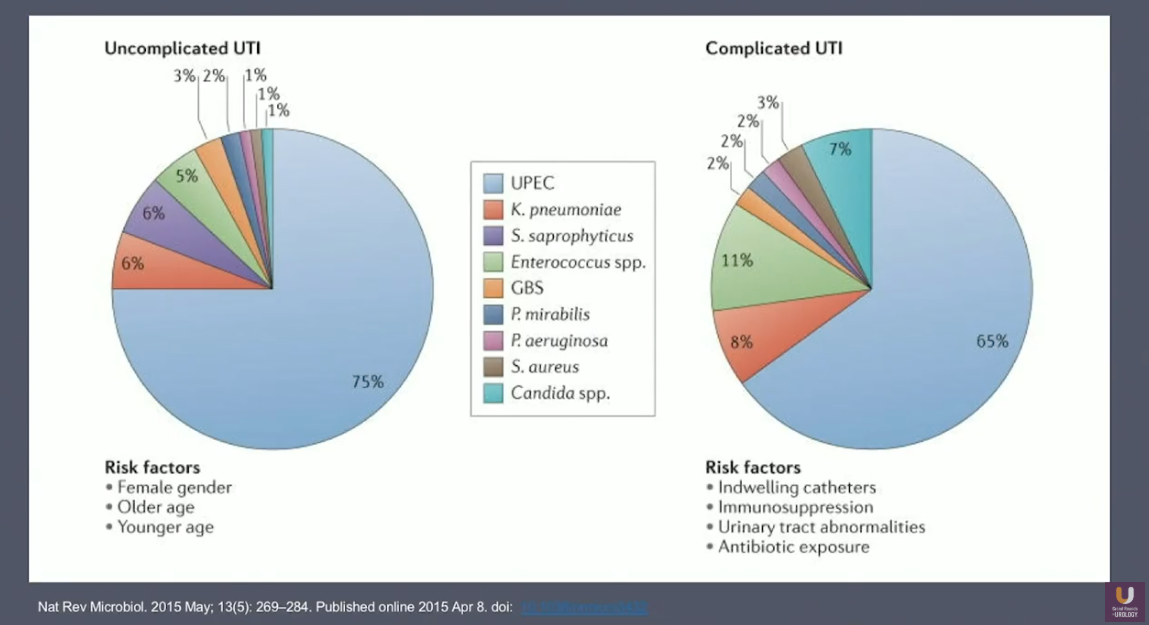
Research indicates that the largest subgroup of infections is catheter-associated urinary tract infections (CAUTI) at 35%. To further illustrate the role CAUTIs play in the resistance epidemic, Woc-Colburn describes risk factors for uncomplicated versus complicated UTIs.
Uropathogenic Escherichia coli (UPEC), is significantly present in cases for either type, with UPEC affecting 75% of uncomplicated UTI cases and 65% of complicated UTI cases. Risk factors for uncomplicated UTIs involve gender and age, as it mainly affects women of both younger and older ages. In contrast, risk factors for complicated UTIs relate directly to medical care: indwelling catheters, immunosuppression, urinary tract abnormalities, and/or antibiotic exposure.
Avoiding Antibiotic Resistance in UTI Treatment
Long-term care requires more than an initial urine culture and treatment for every individual infection. In order to avoid more frequent and increasingly resistant UTIs in the future, prioritizing urinalysis and perineal hygiene is essential.
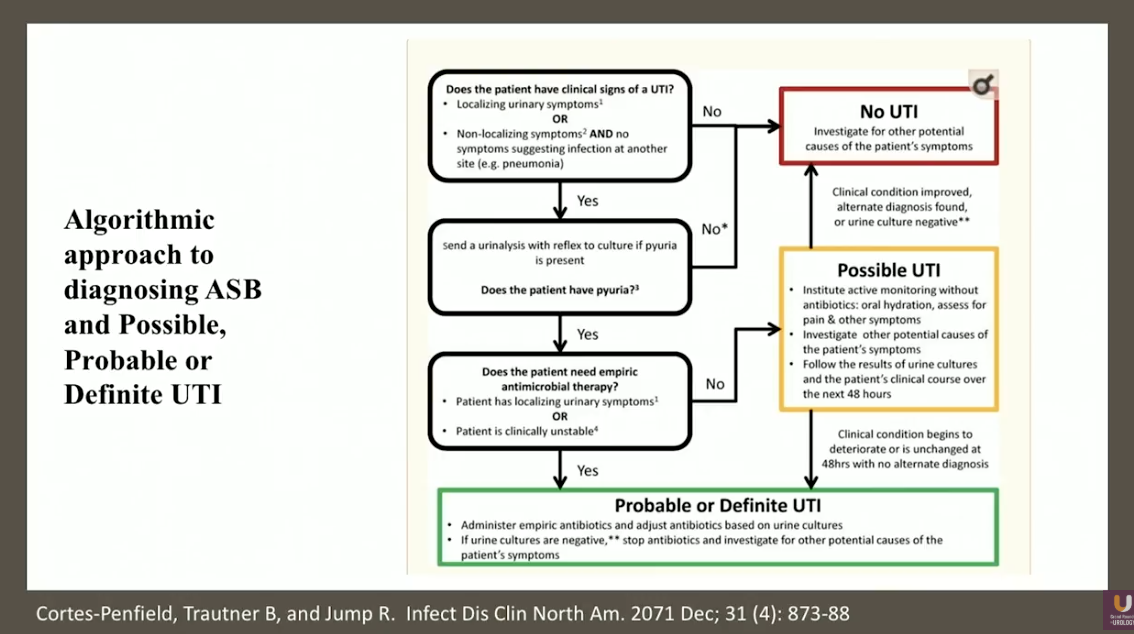
Infectious disease physicians should educate doctors and primary caregivers about treating urologic issues with methods other than the antibiotics used to treat UTIs in order to prevent resistance from developing. Physicians should avoid antibiotics for possible UTIs and instead use oral hydration, investigating other causes of pain and symptoms, and following results of urine culture for 48 hours. For a probable or definite UTI, physicians should administer empiric antibiotics and adjust based on urine cultures. If the cultures are negative, doctors should stop antibiotics and investigate other causes.
When treating MDR gram-negative uropathogens, the first step is to evaluate the degree of resistance, then test minimum inhibitory concentrations for specific antibiotics. Subsequently, test for newer antibiotics that have not been in use frequently enough to cause resistance. Presently, only two antimicrobial treatment options for MDR gram-negative are FDA-approved: ceftazidime-avibactam and ceftolozane-tazobactam. New carbapenems are under investigation, and one new aminoglycoside, plazomicin, is already available on the market. Finally, look at options for combination antibiotics and/or surgery.
Future Directions for Reducing MDR Gram-Negative Infections
The overall future approach for reducing MDR Gram-negative infections should be to implementing fewer days of treatment for UTIs. Additionally, it is necessary to minimize antibiotics by targeting specific pathogens through urinalysis. Physicians should consider combination therapy, pre- and probiotics, for which there are ongoing trials, as well as fecal transplants (FMT). Notably, The Michigan Urological Surgery Improvement Collaborative (MUSIC) is currently aiming to reduce infection and fluoroquinolone resistance related complications in men post-prostate biopsy.
About Innovations in Urologic Practice
Innovations in Urologic Practice (IUP) is an annual CME-accredited conference devoted to updating urologists on the rapidly changing healthcare environment. Topics focus on innovative diagnostic and treatment strategies, controversies, new and currently developing technologies, and challenges in today’s urologic practice. Dr. Woc-Colburn presented this lecture during the 23rd IUP in 2018. Please visit this page in order to learn more about future IUP meetings.
ABOUT THE AUTHOR
Dr. Woc-Colburn is an Associate Professor in the National School of Tropical Medicine as well as in the Infectious Diseases Department at Baylor College of Medicine, Houston, TX. She also serves as Director of Medical Education in the National School of Tropical Medicine and Medical Director of the Baylor Medicine Infectious Disease Group and the Tropical Medicine Clinic at Baylor. She received her MD from Universidad Francisco Marroquin, Guatemala City, Guatemala. She was recruited by the Infectious Diseases Department at Baylor College of Medicine in 2010 to start the HIV/AIDS transition service at Ben Taub Hospital/Harris Health System, Houston, TX. She went on to start the first tropical medicine clinic at Ben Taub Hospital/Harris Health System. Since 2012, she has helped oversee infectious disease cases at Baylor St. Luke’s Medical Center, Houston, TX. Her professional interests include tropical medicine, HIV/AIDS patient care, medical education, endovascular infections, fungal infections, and non-tuberculosis mycobacterium. Dr. Woc-Colburn received the Norton Rose A. Fulbright Faculty Excellence Award in 2016, and the Rising Star Clinician Award in 2015, reflecting her commitment to both medical education and clinical excellence. Dr. Woc-Colburn is a fellow of the American College of Physicians and the Infectious Disease Society of America, as well as a member of the American Society of Tropical Medicine and Hygiene, the International Antiviral Society, and the Asociación Guatemalteca Enfermedades Infecciosas.