How to cite: Goldfischer, Evan R. “Negotiating Hospital Contracts” January 27, 2018. Accessed [date today]. https://grandroundsinurology.com/Negotiating-Hospital-Contracts/
Summary:
Evan R. Goldfischer, MD, MBA, FACS, advises urologists on how to optimally and responsibly negotiate hospital contracts under present-day Fair Market Value parameters. He describes negotiating service arrangements, clinical co-management, call coverage, and quality improvement programs.
Reveal the Answer to Audience Response Question #1
- A. True
- B. False
Answer Explanation:
Hospitals cannot pay you for the amount of work that’s brought to the hospital. They can’t pay for cases. That’s important to understand. Threatening to pull your volume out of a hospital and go somewhere else won’t work. The hospital can’t pay you for keeping your cases there. If they did pay you for that, it would be considered an inducement.
Reveal the Answer to Audience Response Question #2
- A. True
- B. False
Answer Explanation:
Fair-market value is a range. Hospitals can go to the 75th percentile very comfortably. They can go above the 75th percentile when a clear demonstrated need exists, but it’s hard to get above the 75th percentile without a lot more paperwork involved, and a lot more compliance metrics.
Negotiating Hospital Contracts – Transcript
Click on slide to expand
Service Line Agreements
So, we’re going to shift from the science a little bit and talk about negotiating hospital contracts. And they come in a number of different varieties. There are professional service arrangements, there’s clinical co-management agreements, there’s call coverage, and there are quality improvement programs.
Physician Health System Alignment
And when you start to negotiate, and you approach your hospital CEO, the things you have to take into consideration are: the level of autonomy that you want, the level of clinical integration between you and your hospital, the time to implement, what sort of infrastructure and cost it’s going to be, the scale, which is one hospital or the entire system, and of payer interest.
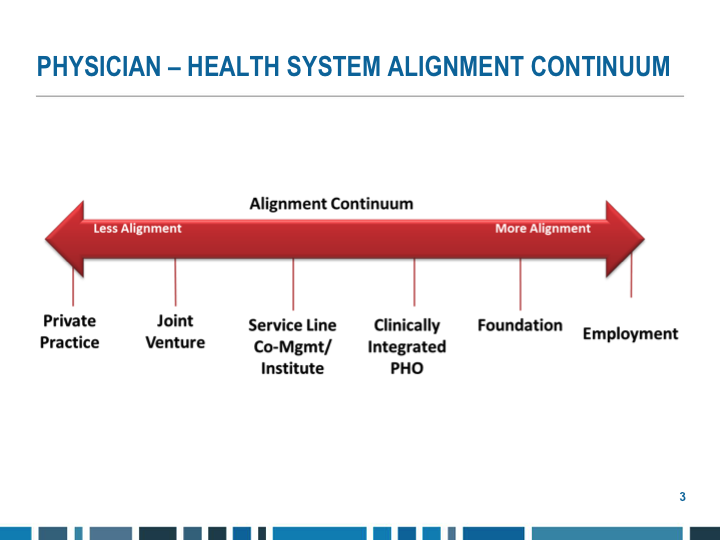
Physician – Health System Alignment Continuum
And, you know, we’re LUGPA. We’re much more on this side of the scale. But, even if you’re an employed urologist, be it directly for the hospital or in academics, you need to work with your hospital, and you need to get paid for your expertise in what you do, because you can save the hospital a lot of money by providing the appropriate services.
Why Do Hospitals Want To Partner?
Why do hospitals even want to partner with us? Well, a lot of them are buying doctors right now, but they have no idea how to effectively manage the service line, particularly if it’s a new service line like urology. They may know how to manage hospital, emergency room doctors, cardiac surgery, things that typically hospital-based, but urology is not typically hospital based, and most hospitals don’t know how to manage it.
They’re going to reimbursed on value-based care, so it’s important that we create the value for them. There is plenty of money on the table, so it’s worthwhile for them. Obviously, they need us to take call for them, and their patients require our specialization, a sub-specialization, and it improves their ability to compete for admission, so they’ve got an efficient urology service.
Why Should We Partner With Hospitals?
Why do we want to partner with them? Well, it is better care. You know, if you got a hospital to provide 24/7, 365 PA coverage for you to handle the first hits to the floor, it reduces response time for a doctor, the patients get taken care of much faster, much more expeditiously. We want to reduce their incentive to develop internal urology departments. We want to protect our independence and our referral base. We certainly want to increase position productivity. We need to work at the level of our degree in order to generate revenue for our practice. We want to help improve OR efficiency. We can help them do that, and if a hospital is part of a large system, and you partner with them, you can be the urology group for the entire system. So it helps expand your geographic reach and improves—it gets you bigger and improves your volume.
Patient Benefit
For the patients, they get improved access to care. They get consistent application of evidence-based medicine, access to well-trained physicians, improved and consistent quality and safety.
Call Coverage & QI Service Arrangements
So let’s start with some of the low-hanging fruit: call coverage. Hospital engages a group of specialists who agree to provide detailed call coverage and other quality improvement services. Specialists from more than one practice may form an LLC to be the contracting entity and physicians in the group become the on-call panel that are responsible for setting the call coverage schedule.
Call Coverage Responsibilities
It’s usually 24/7, 365. It includes ED coverage, hospital consults, unassigned patients, unassigned ED patients, you have to adhere to mandatory response times, and obviously, you have to round on those patients and take care of them.
Call Coverage Compensation
We collect and bill for our services and we get a flat fee for coverage. And the valuation of that flat fee is the extent of burden on the physician, the likelihood of having to come in and respond to the call. Are you a small hospital, a large hospital? Are you a level-1 trauma center? Are you a level-3 trauma center? You’re not a trauma center. And the likelihood you’re going to have to provide uncompensated care, what’s the free care that your hospital gives away, or what’s your Medicaid population—restricted call, meaning if they actually want you in-house, that obviously is a higher compensation than unrestricted call when you’re from home, and they’ve got fair-market value considerations as well.
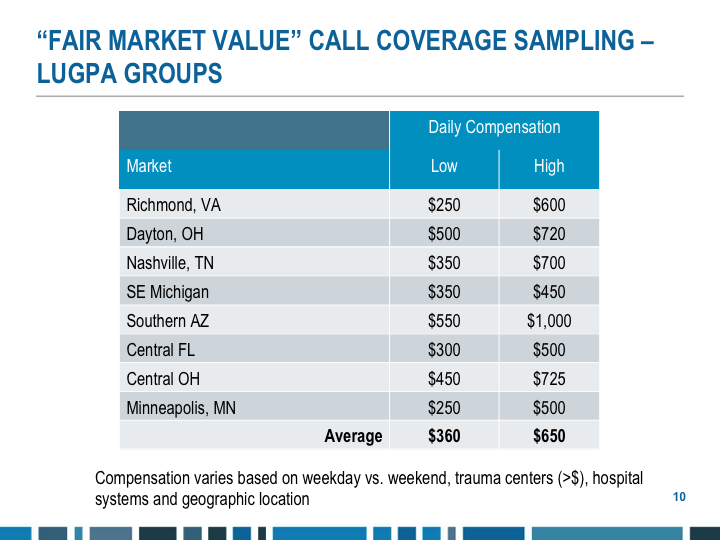
“Fair Market Value” Call Coverage Sampling – LUGPA Groups
So, here is a sampling from various parts of the country of what call is. You’re not worth as much as you think you are. That’s the bottom line. When you go into a hospital and you start to negotiate, you have to understand they’re going talk to you about fair-market value, and it does have to be at fair-market value, because there can’t appear to be an inducement that they’re trying to buy your business. Remember the olden days, 20 years old, you walked to the hospital and said, “I’m going to pull all my cases out of your hospital if you don’t pay me X amount of dollars for a chairmanship or a service line management.”
That doesn’t fly anymore. Everything has to be according to the compliance policy of the hospital, of your group, and a fair-market value. Understand this, this is key, and I learned this in one case the hard way. Fair-market value is never a number. Fair-market value is never a number. Fair-market value is always a range, and you want to know what the range is, and there a lot of different companies that do the fair-market value assessments.
There are those that are typically paid by hospitals, and there are those that are paid by doctors. So, when a hospital comes to you and gives a fair-market value number, you need to know where it came from, the company that did it, and where it lies at the spectrum. Hospitals are going to try and pay you at the 50 percentile or less. They can very easily go to the 75 percentile without going through any sort of business ethics or getting lawyers involved to see if it’s actually true fair-market value. So, you want to strive for the 75 percentile. If you can get better than that, great, but then there’s a lot more compliance issues there.
So this is a range. But in general, roughly, about $600 a day, meaning a 24-hour period for a non-trauma 250-300-bed hospital is kind of the range. If the hospital’s bigger, has trauma, you can do a little bit better. But these are the numbers, just so you kind of understand what you’re going into, because you can’t walk in and say, you know, we want $500 an hour to take call because that’s what we generate in our practice per hour. Doesn’t work.
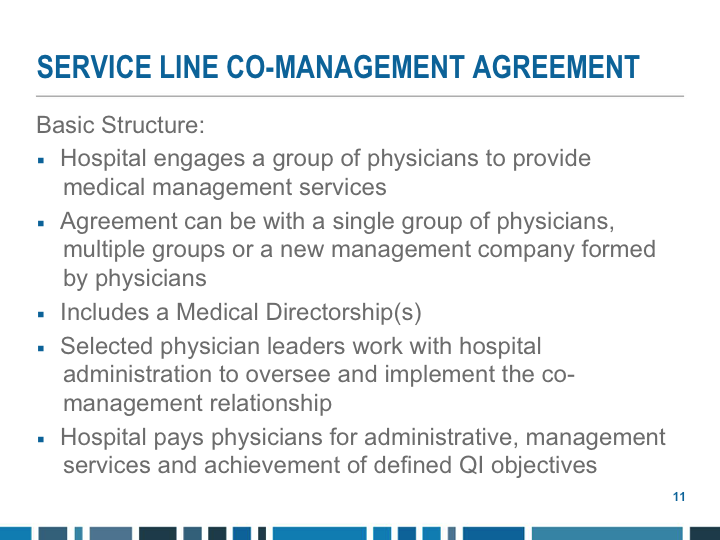
Service Line Co-management Agreement
Service line co-management. Basic structure, they provide—a group of physicians provide medical management services. The agreement can be with a single group of physicians, or multiple groups can come together to form your own company. It includes a medical directorship, and selected physician leaders work with hospital administration to oversee and implement the co-management relationship, and the hospital pays the administrative management services an achievement of defined quality objectives.
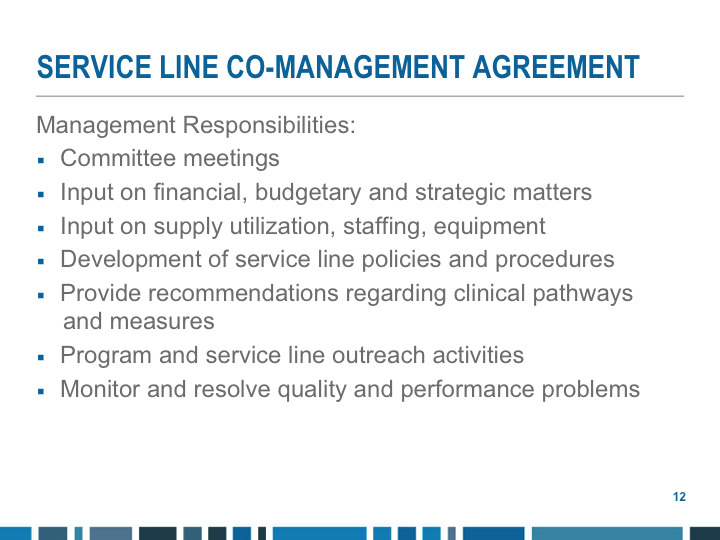
Service Line Co-management Agreement
There are committee meetings you have to attend. You have input on financial, budgetary, and strategic matters, supply utilization, staffing and management, supply utilization, you know, if you’ve got a group of 20, 25 doctors, if one group of doctors insist that we have Boston Scientific stents and another group insists that you have Cook stents, another insists that you have Bard stents, if you get everybody to agree to use the same stent, hospitals save money. Part of that savings can come back to you—service line policies and procedures, recommendations on clinical pathways and measures, program of service line outreach activities, and quality and performance metrics.
Service Line Co-management Agreement
You are compensated, again, based on fair-market value. Usually, it’s an hourly rate, depending on the size of the hospital, the size of the service line, the amount of money going through. The hourly rate is usually between $150 and $300 an hour. You’re not worth as much as an administrator as you are a clinician. There are certain caps that are going to be established, again, because they can only pay you so much money a year, and yes, the work must actually be documented or reported regularly. Our group does it monthly.
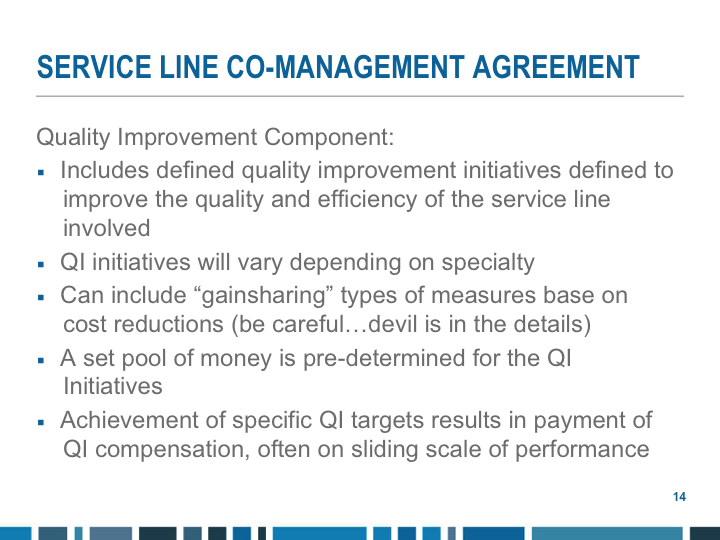
Service Line Co-management Agreement
Quality improvement, you define what the initiatives are, and then you establish gain-sharing types of arrangements based on cost reduction, and a set pool of money is predetermined for this. The longer the relationship is in place, the harder these initiatives are. Let me give you an example. When our group first started doing this, the initiatives were very simple: sign your medical records on time, your operative notes and discharge summaries, get it done within 24 hours, and the other one was show up to the operating room on time. Don’t show up a half an hour late. That was really low-hanging fruit, and for the first two years while those were in place, we got our money.
Then we started doing it. So the bar got raised—how fast did we respond to the emergency room, how fast did we respond to consults from the hospitals. So the longer the arrangements were in place the higher the bar is going to be because you’ve already achieved certain goals and they’re going to want you to achieve more goals, so understand that.
Quality Based Payment Strategies
CMS has decreased payments to hospital-acquired infections, including retain foreign objects, certain surgical-site infections. You all know this is a zero-sum game. Some people win, and some people will lose.
Understand Where Your Hospital Falls Short
So, one of the things that hospitals are really gung-ho about right now are CAUTIs—catheter-acquired urinary tract infections. They have no idea how to stop this problem, and they don’t get paid for the CAUTIs, and it’s a metric that the government really watches. So, you can establish a committee, you can establish a protocol in the use of Foley catheters, you go out educating the nurses and the ER doctors and the hospitals that there are a lot of ways to monitor urine output. You don’t necessarily need a Foley catheter when somebody is mentally competent and able to void.
One of the simple things is just stop putting the catheters in and you’ll decrease your CAUTI rate. But, that’s one thing that’s on the table that hospitals are talking about a lot.
Patient satisfaction survey, that’s a big thing right now, both in-patient and out-patient. Your length of stay and your complication rate, hospitals use Crimson data—Crimson’s based on Texas. They get a lot of data from all the hospitals. You should be meeting with your vice-president for medical affairs of your hospital on a quarterly basis. You should find out what your Crimson data is, what they have. You should understand how it is derived, and then you should set targets to try and improve your Crimson data, length of stay, complications, et cetera. And that is a way for the hospital to pay you for improving quality measures.
And some of it is, again, educational. So what do I mean by that? When you look at length of stay, you have to understand how they derive their length of stay. And if you have one Fournier’s gangrene patient that stayed in the hospital for 60 days and got multiple operations, that is going to completely mess up your length of stay data from the hospital perspective, but they’re just looking at the overall number. So again, learning how to carve out that data is important, so that you see what your true length of stay is, and you get rid of the outliers.
Another things post-operative complications. Post-op day 1, you round on a patient who’s had a robotic prostatectomy. If the doctor writes in the chart patient has an ileus, you now have a complication. No one has an ileus in Poughkeepsie, New York post-op day 1. They have decreased bowel sounds. That is not a complication, but they do not have an ileus. So part of it is learning the system, looking at the key words that Crimson is looking for and understanding how the data is derived, and you can improve your metrics dramatically—time to seek consults on the floor of the emergency room, on-time surgical starts, again, costs of the disposals in the operating room, getting people to agree to only carry one stent, one basket, et cetera.
Research programming, I know a lot of LUPGA groups are doing research. Hospitals have cancer centers now. Cancer centers make money, but cancer centers have to have a certain number of patients per year enrolled in clinical trials. Most hospitals do not know how to manage a research program to get the clinical trials. If you are doing research and you can affiliate your program with the hospital, that is something they can pay you for. It’s good for them; it’s good for you.
How Hospitals Will Evaluate Surgeons
Hospitals are going to start evaluating surgeons based on the quality of care before, during, and after surgery. There’s going to be economic credentials. They’re going to look at three surgeons who are doing robotic prostatectomies in the hospital and they’re going to want to know why one surgeon is 25 percent more expensive than somebody else. Crimson is going live with out-patient as well as in-patient data. And again, quality is the core driver.
Negotiating A Contract
So, in order to negotiate the contract, you’ve got to know your data, and you’ve got to know their data and where they’re getting it. Go after the low-hanging fruit first, understand the finances, what the hospital is looking to save, so you can monetize the metrics, and know what percentage of the savings you can get. Do not have all-or-nothing contracts. You will lose. You know where your baseline is, you know where you’re starting from. There should be an amount of money that you get when you hit your target and then an amount of money when you hit the stretch goal, and then if you become the top decile for a certain metric, then that’s more money. So, set it up on a graduating basis.
And make sure you’re not penalized for things you cannot control. Certain things the hospital has to do and have on-time start rates, for example, in the operating room, and make sure if the anesthesiologist is late, you’re not penalized because it wasn’t an on-time start.
Lessons Learned
Trust is critical, but I’ve been at my hospital now for 20 years and I’ve seen eight CEOs. Get it in writing, that contract is so important because it has to not just survive the current CEO, it has to survive probably four or five more CEOs. Your career at a hospital is much longer than the CEO or a VPMA or a chief operating or financial officer. Everything goes in writing. Don’t just count on it as, “He’s my friend, of course he would never cheat me,” in a contract later on.
There’s got to be transparency in the goals and the numbers, agreed upon communication channels, mutual commitment and—between the two, and if there’s any discrepancy how you’re going to resolve things. And there have to be defined clear measurable targets and exit strategies for both sides if things aren’t working out.
Conclusions
Hospitals that try for quality without physician engagement will fail. Physicians understand their specialty, and we should be compensated now for achieving higher quality and lower costs, and understand if we do not work with hospitals, they will define quality for us, AKA if you’re not at the table, you’re on the menu.
ABOUT THE AUTHOR
Evan R. Goldfischer, MD, MBA, FACS, is a urologist and Director of the Research Department at Premier Medical Group in Poughkeepsie, New York. He received his BA from Tufts University and his MD from Cornell University Medical College. He completed his internship in general surgery and his residency in urology at the University of Chicago. He then completed a fellowship in endourology under the direction of Arthur Smith at Long Island Jewish Medical Center. Dr. Goldfischer received his MBA from the University of Massachusetts and is a certified physician executive. He is the founder and chair of the Board of Premier Cares Foundation, which aims to support and educate individuals who are unable to address significant issues like prostate and colon cancer. He has authored more than 100 peer-reviewed abstracts and publications and has lectured on six continents. Dr. Goldfischer has served as the chair of the Advanced Prostate Cancer Expert Panel for the Public Education Council of the Urology Care Foundation, which is the official foundation of the AUA. He was elected to the LUGPA Board of Directors in 2014 and was elected secretary of LUGPA in November 2018. Dr. Goldfischer was elected president of LUGPA in 2022 and still serves in that role.