Paul D. Maroni, MD, presented “Salvage Lymph Node Dissection for Prostate Cancer” during the 29th Annual International Prostate Cancer Update on January 24, 2019 in Beaver Creek, Colorado.
How to cite: Maroni, Paul D. “Salvage Lymph Node Dissection for Prostate Cancer” January 24, 2019. Accessed Jun 2025. https://grandroundsinurology.com/salvage-lymph-node-dissection-for-prostate-cancer/
Salvage Lymph Node Dissection for Prostate Cancer
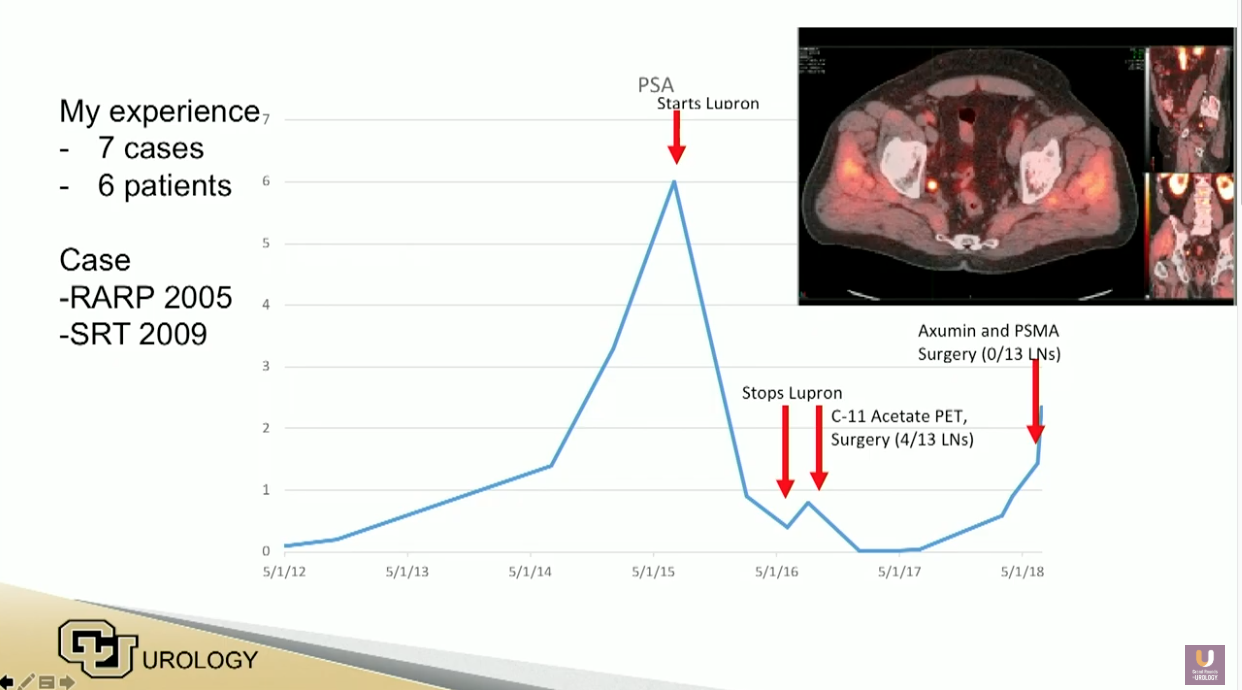
Paul D. Maroni, MD, argues that salvage pelvic lymph node dissection is feasible, safe, and may be efficacious in the treatment of oligometastatic prostate cancer. He reviews data suggesting that this method can optimize locoregional control, limit the risk of distant progression, avoid the necessity for immediate androgen deprivation therapy (ADT), and improve cancer-specific survival.
Abstract:
As imaging technologies have improved, salvage lymph node dissection (SLND) has emerged as a treatment alternative for oligometastatic prostate cancer. Next generation positron emission tomography (PET) scans can identify patients with limited pelvic or retroperitoneal disease who may be candidates for salvage surgery. Open and robotic approaches have efficacy and tolerable morbidity in these situations.
Imaging generally does not determine the full extent of lymph node disease. Given this, the surgical approach should include an extended template of the area involved. Prior pelvic surgery and/or radiotherapy can create unique challenges in these procedures.
Multiple retrospective reviews assessing SLND in nodal recurrent prostate cancer show a PSA response rate of about 40% at 2-years and 20% at 5-years. This may help some patients avoid or delay the need for systemic therapies. There are no randomized trials proving superiority of this approach compared to non-surgical management. Risk factors for early PSA failure (less than 1 year) include higher Gleason score at radical prostatectomy (RP), early PSA rise after RP, retroperitoneal involvement, 3 or more positive spots, or higher PSA at the time of salvage.
Radioguided surgery has very interesting potential in the area of recurrent prostate cancer lesions. Additionally, stereotactic body radiation therapy (SBRT) has been used successfully for treatment of oligometastatic disease.
Salvage pelvic lymph node dissection is feasible, safe, and may be efficacious in prostate cancer management. Further study is needed to determine appropriate clinical situations for the application of this therapy.
About the International Prostate Cancer Update
The International Prostate Cancer Update (IPCU) is an annual, multi-day CME conference focused on prostate cancer treatment updates. The conference’s faculty consists of international experts, and the event caters to urologists, medical oncologists, radiation oncologists, and other healthcare professionals. Topics encompass prostate cancer management, from diagnosis to treating advanced and metastatic disease. Dr. Maroni presented this lecture during the 29th IPCU in 2019. Please visit this page in order to learn more about future IPCU meetings.
ABOUT THE AUTHOR
Paul D. Maroni, MD, is the Program Leader of the Urologic Oncology Program at the University of Colorado in Aurora. He graduated from the University of Virginia in 1996 and from the University of Illinois College of Medicine in 2000. In 2006, Dr. Maroni completed his residency at the University of Colorado at Denver and Health Sciences Center prior to receiving fellowship training in Urologic Oncology at Indiana University. He returned to the University of Colorado as a faculty member in 2007. Dr. Maroni provides care to patients at the Tony Grampsas Urologic Cancer Care Clinic - Anschutz Medical Campus, where he specializes in robotic surgery for prostate or kidney cancer. As of 2020, he had performed over 1000 robotic prostate removals. He also performs minimally invasive HoLEP procedures for patients with enlarged prostates.
Dr. Maroni has published widely on the topics of prostate and testicular cancer. His specific clinical and academic interests include minimally invasive therapies for prostate cancer, robotic surgery, and surgery for metastatic testicular cancer. He is an investigator for numerous clinical trials about a wide range of subjects, from diagnostic tools to complementary medicines to immunotherapy for localized prostate cancer. Dr. Maroni’s other research interests center in quality of life outcomes for patients with prostate cancer and testicular cancer. His ultimate goal is that patients who survive cancer return to a better-than-normal state and use their cancer diagnoses to engage in healthy, life-enhancing behaviors.