Seth P. Lerner, MD, presented “T1 Bladder Cancer” during the 3rd Annual International Bladder Cancer Update on January 23, 2019 in Beaver Creek, Colorado.
How to cite: Lerner, Seth P. “T1 Bladder Cancer” January 23, 2019. Accessed Jun 2025. https://grandroundsinurology.com/t1-bladder-cancer/
T1 Bladder Cancer – Summary:
Seth P. Lerner, MD, provides an overview of T1 bladder cancer staging and treatment, emphasizing the importance of re-TUR. He then discusses when to offer radical cystectomy or BCG, and options for patients who have failed BCG.
Substaging and Risk-stratifying T1 Bladder Cancer
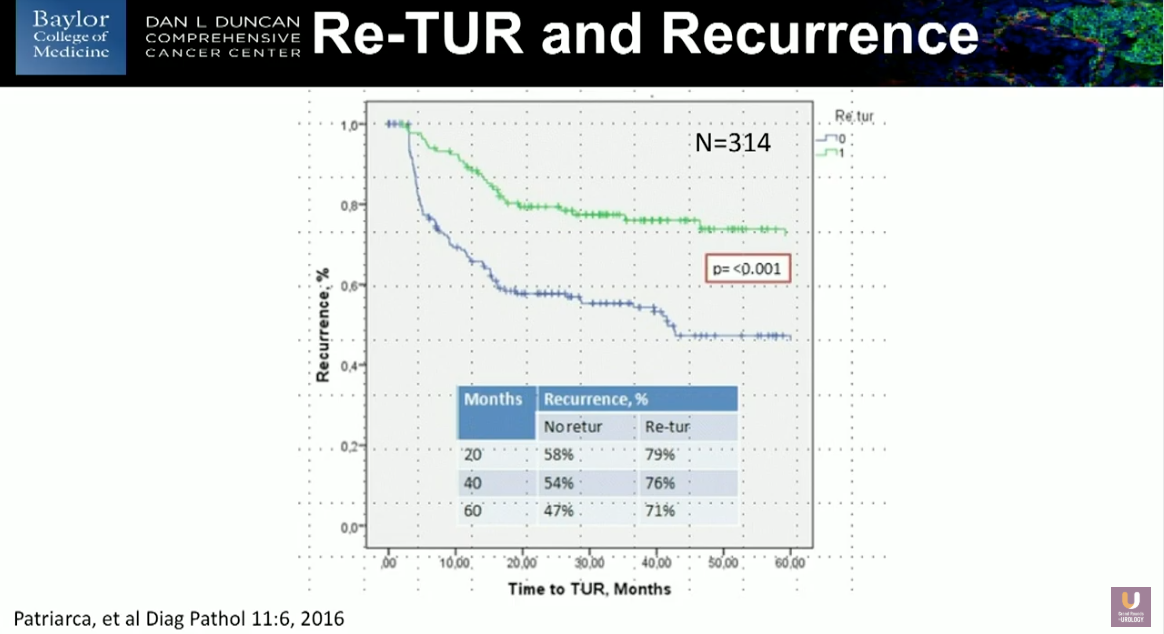
With minor exceptions, T1 bladder cancer is always high-grade and high-risk. However, the depth of the cancer in the lamina propria can provide substaging for T1 bladder cancer. Patients with multifocal and/or large volume tumors, associated carcinoma in situ (CIS), prosthetic urethra involvement, deep invasion into the lamina propria, and vairant histologies are typically considered high risk. Assessing T1 patients to substage their disease is important, and re-resection is currently standard of care for all T1 patients. However, there may be ways to avoid re-section.
Additionally, if the initial resection specimen does not include any of the detrusor muscle, then the results of the test will likely be inaccurate. Analysis shows a highly statistically significant difference in patient outcome by simply stratifying with the covariant of whether or not there was a re-resection.
However, researchers in Europe have suggested that re-transurethral resection (TUR) may not be necessary in all cases, and this may lead to future revision of guidelines.
Treatment Decision-making in T1 Bladder Cancer
When treating bladder cancer, physicians should not be over-cautious about radical cystectomy, as waiting tends to result in worse outcomes. Some characteristics of disease that may benefit from initial cystectomy include presentation of T1 disease as progression from Ta or Tis cancer, primary T1G3 cancer, lymphovascular invasion (LVI) in stage T1, or variant histology. The American Urological Association (AUA) and European Association of Urology (EAU) guidelines for initial cystectomy are fairly consistent. If patients have no very high-risk features and no T1 on re-resection, they should receive Bacillus Calmette-Guerin (BCG) followed by three years of maintenance post-induction. Drug options for patients who have failed BCG include BCG/interferon-alpha2B and valrubicin, among others under investigation.
Regarding future directions of T1 disease treatment, researchers are working on more precise methods of sub-staging using transcriptomics. Additionally, there are many current trials which aim to find better treatments for BCG-unresponsive patients.
About the International Bladder Cancer Update
The International Bladder Cancer Update (IBCU) is an annual one-day CME conference focused on bladder cancer treatment updates. IBCU takes place during its sister conference, the International Prostate Cancer Update (IPCU). The conference’s faculty consists of international experts, and the event caters to urologists, urologic oncologists, and other healthcare professionals. In addition to didactic lectures, IBCU features interactive discussions, a panel roundtable, debates, and case presentations. Dr. Lerner presented this lecture during the 3rd IBCU in 2019. Please visit this page in order to learn more about future IBCU meetings.
ABOUT THE AUTHOR
Seth P. Lerner, MD, FACS, is Professor of Urology and Vice-Chair for Faculty Affairs in the Scott Department of Urology at the Baylor College of Medicine in Houston, Texas. He holds the Beth and Dave Swalm Chair in Urologic Oncology. Dr. Lerner is the Director of Urologic Oncology and the Multidisciplinary Bladder Cancer Program, also at Baylor.
Dr. Lerner earned his medical degree from the Baylor College of Medicine, completed a surgical internship at Virginia Mason Hospital in Seattle, and returned to Baylor for his residency training. He completed a two-year fellowship at the University of Southern California in Urologic Oncology and Reconstructive Surgery and joined the full-time Baylor faculty in 1992.