John W. Davis, MD, FACS, presented “The Pros and Cons of Genomic Markers for Biopsy Guidance” during the 23rd Annual Innovations in Urologic Practice on September 14, 2018 in Santa Fe, New Mexico.
How to cite: Davis, John W. “The Pros and Cons of Genomic Markers for Biopsy Guidance” September 14, 2018. Accessed May 2025. https://grandroundsinurology.com/the-pros-and-cons-of-genomic-markers-for-biopsy-guidance/
The Pros and Cons of Genomic Markers for Biopsy Guidance – Summary:
John W. Davis, MD, discusses the benefits and limitations of utilizing genomic markers in order to guide prostate biopsy. While genomic markers may not be reliable risk stratification tools alone, they may play a role in risk-refining certain populations and providing information beyond clinical parameters.
Abstract:
This is a partner presentation coupled with Dr. Guilherme Godoy’s “The Pros and Cons of Imaging for Biopsy Guidance.”
There is a constructed debate between MRI image guided biopsy and genomic biomarkers in the urologic community. However, the optimal approach to assessing tumors likely involves a complementary pathway using both at the appropriate time.
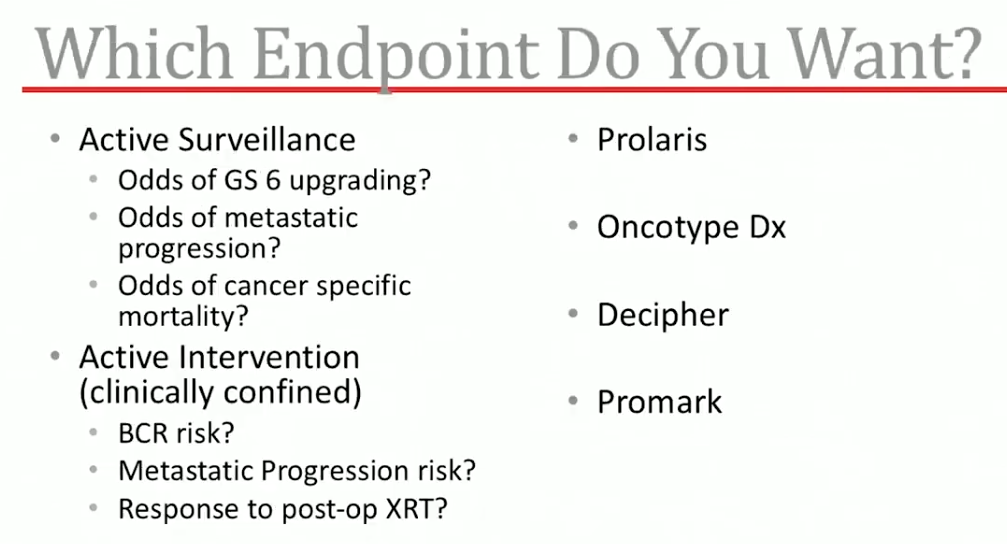
Urologists have requested genomic markers for decades due to the limitations of Gleason scores at reflecting the true metastatic and/or disease specific mortality potential of a tumor. Although, evidence shows biopsy Gleason score and radical prostatectomy Gleason score have significant discordance.
Currently, genomic markers are prognostic and not predictive. However, they often have more prognostic power than clinical parameters. Both will have increased cost potential, but perhaps cost savings with proper downstream decisions in active surveillance monitoring versus treatment. The pro side of genomic markers includes robust clinical validation, information beyond clinical parameters, as well as consistency across labs compared with MRI quality.
About Innovations in Urologic Practice
Innovations in Urologic Practice (IUP) is an annual CME-accredited conference devoted to updating urologists on the rapidly changing healthcare environment. Topics focus on innovative diagnostic and treatment strategies, controversies, new and currently developing technologies, and challenges in today’s urologic practice. Dr. Davis presented this lecture during the 23rd IUP in 2018. Please visit this page in order to learn more about future IUP meetings.
ABOUT THE AUTHOR
John W. Davis, MD, is a Professor of Urology and Director of the Urosurgical Prostate Program at the University of Texas MD Anderson Cancer Center in Houston. He received his BS in Biology at Davidson College in North Carolina in 1990. He then went on to earn his medical degree at the University of Virginia in 1994 and completed his residency training at Eastern Virginia Graduate School of Medicine in Norfolk. Dr. Davis had fellowship training in prostate cancer research in the Department of Microbiology and Molecular Cell Biology at Eastern Virginia Medical School, and received an American Foundation of Urologic Disease Scholar award for proteomic applications in prostate cancer biomarkers. He completed a Clinical Fellowship in Urologic Oncology at the MD Anderson Cancer Center, and a Fellowship in Laparoscopic Urology at Charité Hospital in Berlin, Germany, under the mentorship of Ingolf Tuerk.
Dr. Davis’ clinical interests include patients with urologic cancers, laparoscopic/robotic surgery, and general urology. His academic interests include quality of life after prostate cancer treatment, outcomes for robotic radical prostatectomy, high-risk prostate cancer trials, active surveillance for prostate cancer, and development of robotic surgical techniques for invasive bladder cancer. He has participated as an investigator in several Southwest Oncology Group and industry-sponsored clinical trials.