PCa Commentary | Volume 124 – July 2018
Posted by Edward Weber | July 2018
ACTIVE SURVEILLANCE: EFFORTS TO IMPROVE ITS PERFORMANCE – The Multiparametric MRI
The goal of active surveillance (AS) is to delay treatment, avoiding its associated adverse effects for as long as appropriate, while ensuring that selective delayed intervention will still result in a good outcome. This management strategy has been under development for more than 20 years. It has been increasingly accepted as an appropriate option for men with low-risk disease, but further refinement is required in patient selection and monitoring strategy.
Focus groups involving physicians providing care for low-risk prostate cancer and patients were held in five centers across Canada. Their goal was “to evaluate the factors that influence physicians to recommend active surveillance and the barriers that impact adherence to this approach”¹. Not surprisingly, a major topic was optimizing criteria for patient selection and “concern about the rapidly evolving and non-standardized guidelines for patient follow-up.”
What are the current selection criteria for AS, AS outcomes, and rate of intervention?* Criteria:
Standard clinical features are currently the basis of selection criteria for identifying patients for AS: i.e., Gleason score 6, PSA < 10 ng/mL, clinical tumor stage T1c or T2a, PSA density <0.15, and increasingly, only one or two positive biopsy cores with no core having > 50% cancer. Some protocols allow eligibility for patients with favorable-risk intermediate-risk Gleason score 3+4 = 7 but with only a minimal percentage of Gleason pattern 4. PSA density (PSAD) is increasingly recognized as an important determinant for indicating significant cancer. The upper limit for AS has been set at no greater than 0.15 ng/mL/cm3. For perspective, the median PSAD for men without cancer is about 0.08. The PSA density is calculated by dividing total PSA by gland volume in cc3.
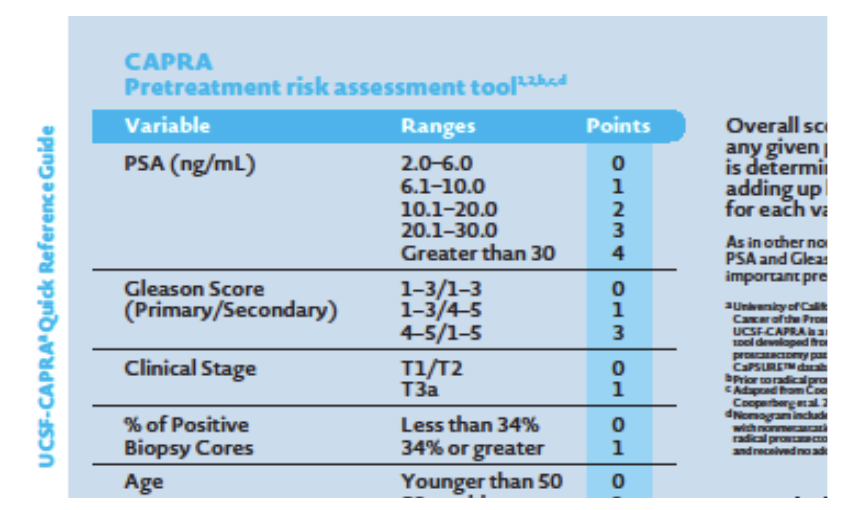
The USCF Cancer of the Prostate Risk Assessment tool (CAPRA) is a pretreatment calculator that predicts pathological findings post prostatectomy, and also predicts 3- and 5-year progression-free survival. The resulting score can usefully augment the decision to enter AS.
Some clinicians are concerned that applying the most restrictive selection criteria, i.e. those of Johns Hopkins, will unnecessarily limit eligibility for patients with favorable-risk intermediate-risk cancer. To this end, some protocols extend eligibility to men with Gleason score 3+4 = 7, but only with a minimal percentage of secondary Gleason pattern 4, e.g. 5-10%. (It is now recommended that the pathology report include percentage of pattern 4 for Gleason 7 cancers.) Laurence Klotz, MD, FRCSC, and Matthew R. Cooperberg, MD, MPH, UCSF, are researching the safety of this allowance. In this situation Dr. Klotz has suggested that the genomic test, Prolaris, could augment selection decisions. *
Outcome:
Vol.114, PCa Commentary, Aug. 2017 PCa Commentary Vol 114 presents a full discussion of the Johns Hopkins data² regarding outcome for low- and very low-risk patients on AS. In short, their data showed that the cancer-specific survival for the 1298 men in the trial was projected to be 99.9% at both 10 and 15 years. In Current Opinion in Urology, May 2017, Dr. Klotz affirmed his opinion that: “Low risk and many cases of low-intermediate risk prostate cancers are indolent, have little or no metastatic potential, and do not pose a threat to the patient in his lifetime.”³ He stressed that a key component of good management “Is the early identification of those patients who have been misattributed as having low-risk disease, who in fact harbors higher risk disease, and are likely to benefit from definitive therapy.” He asserts that proper management with early intervention based on repeat biopsy, imaging, or biomarkers yields a “0.5-3% cancer-specific mortality at 10-15 years.” Johan Stranne, MD, PhD, FEBU, at the EAU PCa Conference 2017 cited 7 high-quality studies that reported “cancer-specific (98.1-100%) and overall survival (85-100%) outcomes among men with prostate cancer on active surveillance.” *Need to Convert to Delayed Intervention: It is clear that by using the current clinical criteria for eligibility the outcome of AS in many studies is very satisfactory. In the Johns Hopkins study, intervention with curative intent occurred at a median 3 years – 37% at 5 years, 50% by 10 years, 57% by 15 years. In a Swedish study of AS4, the median time to intervention was 1.9 years. With trial data showing excellent outcomes, the current thrust in research in AS is to reduce the rate of early intervention by better identifying those men with potentially more aggressive disease at the onset before starting AS. Currently the most promising tools to accomplish this are the multiparametric MRI and the early efforts to utilize genomic analysis (not covered in this Commentary). A rational approach to follow-up during AS was outlined by Carter, Eur Urol, 20165, writing at a time before MRI was establishing a role in AS: digital rectal exam yearly, PSA “at 3 – 6 month intervals, transrectal ultrasound-directed biopsy within 12 months of diagnosis, and serial prostate biopsies at 2-5 year intervals thereafter.” He cited a “general consensus that PSA kinetics are not specific for disease progression, but should trigger further evaluation rather than intervention.” An up-grading to Gleason 3+4 or higher on biopsy is considered “significant cancer” and customarily is a trigger for initiating treatment.
The Role of MRI in the Management of Active Surveillance:
Two presentations by Dr. Klotz and Dr. Ivo G. Schoots: A major finding shared by both Klotz and Schoots based on numerous studies is that the greatest likelihood of diagnosing significant cancer at confirmatory or maintenance (i.e. during surveillance) biopsies is achieved by doing both MRI-guided targeted biopsies into the dominant lesion (Dr. Klotz recommends three cores) and a standard systematic 12-core template biopsy. A shared finding of Gleason Score 7 or greater cancer may be found together on both techniques, but, while percentages vary, there are enough instances of cancer identified by one technique and not the other to warrant the dual approach. 1.) Schoots et al. published an article on this subject with an amusing title: “Role of MRI in low-risk prostate cancer: finding the wolf in sheep’s clothing or the sheep in wolf’s clothing?”6. [The latter portion of the quote refers to using a genomic classifier to identify cancers predicted to be biologically less aggressive than implied by Gleason 3+4 on biopsy.] In their opinion, an MRI and MRI-targeted biopsy can be used at confirmation or during surveillance to detect individuals with higher grade cancer who were initially diagnosed as Gleason 3+3 (“the wolf in sheep’s clothing”). “Unfortunately, the sensitivity of TRUS-guided biopsy is known to be low, especially in the case of anterior tumors or large prostates.” A confirmatory biopsy is recommended within one year of the original (usually) TRUS biopsy and historically finds 20-30% of cancers of higher Gleason score than 3+3 and suggests the need for immediate intervention. * Confirmatory biopsies: In pooled data from 13 studies, 32% of men were up-graded based on the combination of an MRI-targeted and a standard TRUS confirmatory biopsy — 13% found on both studies, 11% on TRUS biopsy alone, and 8% solely in MRI-targeted biopsy. * Surveillance biopsies: Biopsies during AS are recommended every 1 – 4 years. In men without a prior MRI-guided biopsy, up-grading was seen in 17% of men with the combined techniques. However, even men undergoing periodic routine serial MRI-targeted and systematic TRUS-guided biopsies continue to be found to harbor higher grade cancer. In one study, in men whose MRI showed stability or regression, there was a 21% rate of progression. 2.) Klotz: “Role of MRI in the Management of Active Surveillance”7 is the title and subject of an excellent video interview with Dr. Leonard Klotz sponsored by UroToday: https://www.urotoday.com/categories-media/1748-centers-of-excellence/advanced-prostate-cancer-coe/868-embedded-media2017-11-14-19-50-55.html Dr. Klotz, Professor of Surgery at Sunnybrook Health Sciences Centre, Toronto, is clearly one of the “deans” of AS, having written and worked in this area for 20+ years. The presentation offers a “state-of-the-art” evaluation as to where the field currently stands in this rapidly evolving issue.
Managing AS Using Only mpMRI:
This issue was addressed by Thurtle et al.: “Progression and treatment rates using an active surveillance protocol incorporating image-guided baseline biopsies and multiparametric magnetic resonance imaging monitoring for men with favorable, low-risk prostate cancer.” “Of 145 men … [biopsies were] triggered either by a rise in PSA level, change in mpMRI findings, or [specified] by protocol.” Disease progression was seen in 15.9%, requiring treatment and yielding a conversion rate of 11.7%, <4%/year. “Progression was detected in six men, however, solely after a protocol re-biopsy without prior PSA or mpMRI changes. Using PSA and mpMRI changes alone to detect progression was found to have only a sensitivity and specificity of 70.0% and 81.7%, respectively.”
BOTTOM LINE:
Currently employed selection criteria for AS yield excellent results. The detection of higher Gleason grade cancers at confirmatory and monitoring biopsies is best accomplished by the combination of standard systematic 12-core and MRI-guided targeted biopsies. Managing AS solely with MR imaging is not ready for prime time.
References
- Pang K, et al. Describing perspectives of health care professionals on active surveillance for the management of prostate cancer. BMC Health Services Research. June 2018.
- Tosoian et al. Intermediate and longer-term outcomes from a prospective active-surveillance program for favorable-risk prostate cancer. JCO. Oct 2015.
- Klotz L. Active surveillance for low-risk prostate cancer. Current Opinion in Urology. May 2017.
- Godtman RA, et al. Long-term outcomes after deferred radical prostatectomy in men initially treated with active surveillance. J Urol. May 2018.
- Carter HB. Optimizing active surveillance. Eur Urol. 2016
- Schoots IG, Moore CM, Rouvière O. “Role of MRI in low-risk prostate cancer: finding the wolf in sheep’s clothing or the sheep in wolf’s clothing?” Current Opinion in Urology, 2017.
- Role of MRI in the Management of Active Surveillance. Urotoday.com. https://www.urotoday.com/categories-media/1748-centers-of-excellence/advanced-prostate-cancer-coe/868-embedded-media2017-11-14-19-50-55.html. Published November 14, 2017.
- Thurtle D, et al. Progression and treatment rates using an active surveillance protocol incorporating image guided baseline biopsies and multi-parametric MRI monitoring for men with favourable risk prostate cancer. BJU Int. Feb 2018.
Your comments and requests for information on a specific topic are welcome e-mail ecweber@nwlink.com. Please also visit https://prostatecancerfree.org/prostate-cancer-news for a selection of past issues of the PCa Commentary covering a variety of topics.
“I want to thank Dawn Scott, Staffperson, Tumor Institute Radiation Oncology Group, & Mike Scully, Librarian, Swedish Medical Center for their unfailing, timely, and resourceful support of the Commentary project. Without their help this Commentary would not be possible.”
ABOUT THE AUTHOR
Edward Weber, MD, is a retired medical oncologist living in Seattle, Washington. He was born and raised in a suburb of Reading, Pennsylvania. After graduating from Princeton University in 1956 with a BA in History, Dr. Weber attended medical school at the University of Pennsylvania. His internship training took place at the University of Vermont in Burlington.
A tour of service as a Naval Flight Surgeon positioned him on Whidbey Island, Washington, and this introduction to the Pacific Northwest ultimately proved irresistible. Following naval service, he received postgraduate training in internal medicine in Philadelphia at the Pennsylvania Hospital and then pursued a fellowship in hematology and oncology at the University of Washington.
His career in medical oncology was at the Tumor Institute of the Swedish Hospital in Seattle where his practice focused largely on the treatment of patients experiencing lung, breast, colon, and genitourinary cancer and malignant lymphoma.
Toward the end of his career, he developed a particular concentration on the treatment of prostate cancer. Since retirement in 2002, he has authored the PCa Commentary, published by the Prostate Cancer Treatment Research Foundation, an analysis of new developments in the prostate cancer field with essays discussing and evaluating treatment management options in this disease. He is a regular speaker at various prostate cancer support groups around Seattle.