Jason A. Efstathiou, MD, MPhil, presented “External Beam Radiation Therapy for High-Risk/Locally
Advanced Prostate Cancer: The Shifting Landscape” during the 24th Annual Southwest Prostate Cancer Symposium on April 12, 2019 in Scottsdale, Arizona.
How to cite: Efstathiou, Jason A. “External Beam Radiation Therapy for High-Risk/Locally
Advanced Prostate Cancer: The Shifting Landscape” April 12, 2019. Accessed Mar 2025. https://grandroundsinurology.com/external-beam-radiation-therapy-for-high-risk-locally-advanced-prostate-cancer-the-shifting-landscape/
External Beam Radiation Therapy for High-Risk/Locally Advanced Prostate Cancer: The Shifting Landscape – Summary:
Jason A. Efstathiou, MD, DPhil, emphasizes the need for continued clinical trials to refine therapy options for high-risk and locally advanced prostate cancer patients. He reviews six major considerations regarding the current state of external beam radiation therapy (EBRT) for the treatment of high-risk disease.
The Current State of Radiation Therapy for Prostate Cancer
Current recommendations for PSA screening have resulted in less screenings being performed, contributing to a trend of a decrease in the incidence of low-risk disease and an increase of high-risk and/or metastatic disease. Correspondingly, prostate cancer management has shifted considerably. There has been a rise in radical prostatectomies and indications for postoperative radiation therapy, as well as a proliferation of radiation treatment options.
In terms of radiation therapy, the National Comprehensive Cancer Network (NCCN) currently supports external beam radiation therapy (EBRT) with androgen deprivation therapy (ADT), EBRT with ADT and brachytherapy, as well as EBRT with or without ADT as adjuvant therapy following surgery in the setting of high- or very-high-risk prostate cancer.
Six Considerations for Radiation Therapy
In addition to the guidelines, radiation oncologists should be aware of certain considerations when managing these patients in the modern era. This presentation focuses on six of these considerations, starting with the fact that hormone therapy should always be accompanied by radiation therapy. Large trials have shown clear benefit to cancer-specific survival and reductions in disease-related deaths. Contraposing this is the second point, which is that radiation therapy should always be accompanied by hormone therapy, unless local control with radiation is possible. In general, hormone therapy is most effective when used with a longer duration.
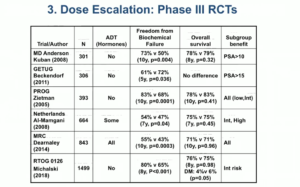
Thirdly, recommendations support offering dose escalation to assist in cancer control, but evidence shows no benefit to overall survival rates with this method. Also, toxicity is a concern that must be addressed.
Fourth, there is data to suggest radiation and prostatectomy are both equally effective treatments for high-risk patients. However, a randomized trial in the high-risk disease setting is needed to confirm these findings. Fifth, in general, there is no proven difference in outcomes between whole-pelvis irradiation and prostate-only irradiation. Sixth, studies suggest that there is a benefit to adding radiation to ADT in pathologic node-positive disease, but data regarding clinically node-positive disease in this area is inconclusive.
In conclusion, more randomized trials must be conducted to refine the treatment of high-risk prostate cancer. Ultimately, most high-risks disease warrants multimodal treatment, and therefore these refinements should occur on a multidisciplinary level.
About the Southwest Prostate Cancer Symposium
The Southwest Prostate Cancer Symposium (SPCS) is a multi-day conference that seeks to educate urologists, radiation oncologists, medical oncologists, and other healthcare professionals involved in the treatment of prostate cancer. The topics focus on current technical aspects of diagnosis and treatment of localized and advanced disease, particularly regarding imaging, technology, and training in the related devices. Dr. Efstathiou presented this lecture during the 24th SPCS in 2019. In 2020, the 25th SPCS will also offer training sessions involving imaging, scanning, and prostate cancer treatment related devices on site. Please visit this page in order to register for future SPCS meetings.
ABOUT THE AUTHOR
Jason A. Efstathiou, MD, DPhil, is Professor of Radiation Oncology at Harvard Medical School (HMS) as well as Director of the Genitourinary (GU) Division in the Department of Radiation Oncology and Clinical Co-Director of the Claire and John Bertucci Center for GU Cancers at Massachusetts General Hospital. He is a recognized leader in the fields of GU malignancies and radiation oncology. Dr. Efstathiou holds a BS from Yale University, an MD from Harvard Medical School, and a DPhil from the University of Oxford. He completed his residency training through the Harvard Radiation Oncology Program.
Dr. Efstathiou’s research has informed clinical guidelines and made novel contributions to innovations such as organ preservation therapy for bladder cancer, technology assessment of proton beam therapy for prostate cancer, indications for and adverse effects of androgen deprivation therapy for prostate cancer, improving radiation therapy for testicular cancer, and global oncology outreach efforts.
In addition to his educational work and his patient care, Dr. Efstathiou holds leadership positions within cooperative groups and professional societies