James S. Wysock, MD, MSc, presented “Multicenter Clinical Trial of Real-Time Prostate Cancer Diagnosis Using Optical Spectroscopy Guided Prostate Biopsy” for the Grand Rounds in Urology audience in September, 2019.
How to cite: Wysock, James S. “Multicenter Clinical Trial of Real-Time Prostate Cancer Diagnosis Using Optical Spectroscopy Guided Prostate Biopsy” September, 2019. Accessed Nov 2025. https://grandroundsinurology.com/multicenter-clinical-trial-of-real-time-prostate-cancer-diagnosis-using-optical-spectroscopy-guided-prostate-biopsy/
Multicenter Clinical Trial of Real-Time Prostate Cancer Diagnosis Using Optical Spectroscopy Guided Prostate Biopsy – Summary:
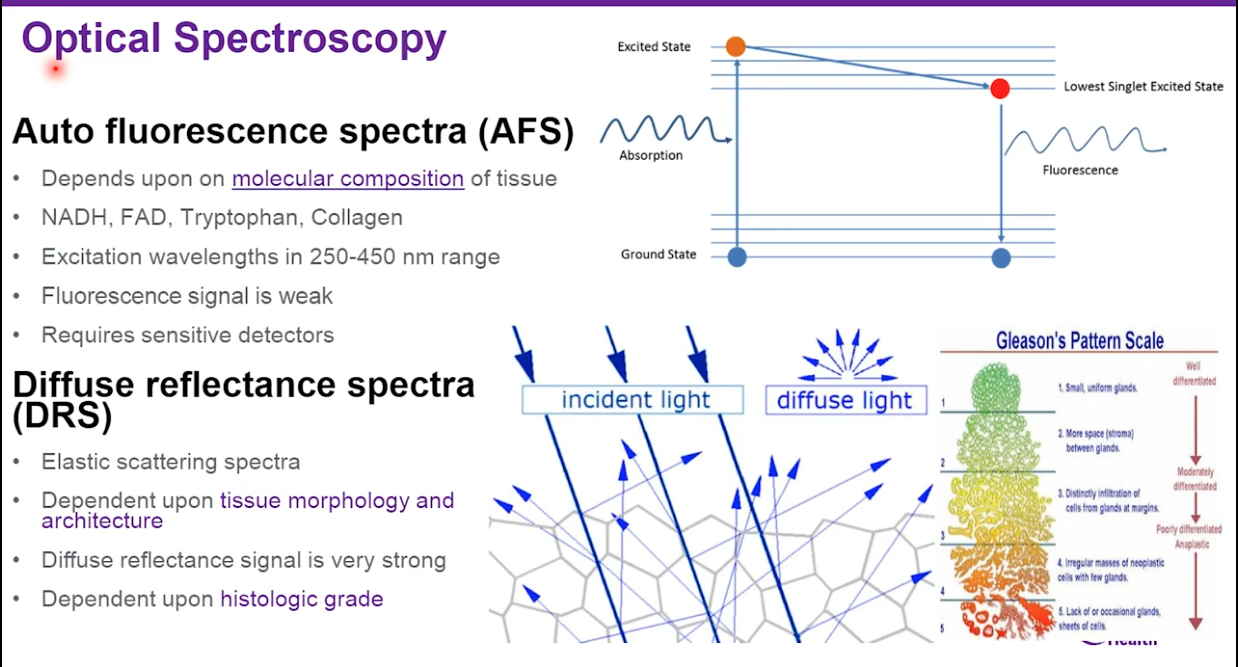
James S. Wysock, MD, MSc, discusses the Phase I trial of the ClariCore(TM) Optical Biopsy system. He outlines the limited efficacy of transrectal ultrasound (TRUS) prostate biopsies, the use of optical spectroscopy to detect Gleason patterns, and details the function and trial performance of the system.
Abstract:
TRUS-guided prostate biopsy remains the principal method for prostate tissue evaluation. As an outpatient procedure done under local anesthesia, it is accessible and scalable approach to the sizeable patient population that requires prostate cancer evaluation. However, this method remains hindered by issues such as false-negative rates and incorrect disease grading. Despite the addition of repeat TRUS biopsies performed in a patient, cancer detection does not necessarily improve.
While the introduction of multiparametric MRI into the diagnostic pathway has shown to improve the detection of clinically significant disease and decrease the detection of insignificant disease, there are still unresolved factors influencing the accuracy of targeted prostate biopsy sampling. Currently, concerns including needle deflection and variability of results based on operator experience continue to pose challenges. A lack of consensus exists regarding biopsy approach, such as whether a transrectal or transperineal approach and an end-fire probe or side-fire probe is optimal, and the ideal number of cores taken.
The ClariCore(TM) Optical Biopsy system employs a biopsy needle integrated with fiber optics to transmit, receive, and capture spectral information. This presentation reviews findings from a muti-institutional Phase I trial analyzing the utilization of this device. Overall, optical biopsy demonstrated encouraging initial results and an acceptable safety profile, meriting further investigation.
ABOUT THE AUTHOR
James S. Wysock, MD, MSc, is a Clinical Assistant Professor of Urology at New York University Grossman School of Medicine in New York, New York. Dr. Wysock also serves as the Division Chief of Urology at Bellevue Hospital Center in New York City. His research focuses on advanced imaging techniques and treatment tools to optimize cancer diagnostics and therapy. Dr. Wysock’s clinical research efforts focus on image-guided prostate cancer diagnosis and treatment, including MRI-US fusion biopsy and partial gland prostate ablation techniques, and his specialization in urologic oncology includes cancers of the kidneys, bladder, ureters, testes, and prostate.