How to cite: Shore, Neal D. “A Primer on Alternative Payment Models: The Need for a Urology APM” January 27, 2018. Accessed [date today]. https://grandroundsinurology.com/a-primer-on-alternative-payment-models-the-need-for-a-urology-apm/
Summary:
Neal D. Shore, MD discusses a different angle of the urologists experience: the need for alternative payment models (APMs) and impact of the Merit-Based Incentive Payment System (MIPS). Many urologists do not have APM options, but the Large Urology Group Practice Association (LUGPA) is trying to change this. Dr. Shore believes an understanding of the systems in place and the need for a urology APM is important for urologists to know.
The Present and Future of LUGPA – Transcript
Click on slide to expand
A Primer on Alternative Payment Models: The Need for a Urology APM
So this whole concept of APM development or alternative payment models and why do we need one, and that probably, if I could get that message across, that may be one of the best things I can do in this presentation. Remember that the Affordable Care Act came after MACRA was already approved by Congress with overwhelming bipartisan support.
USPSTF
And the reason why we have MACRA is because we were for 20 some plus years kicking the can down the road with the sustained growth rate, or the SGR, which was a proverbial sort of Damocles over all of us that we were going to have marked reductions in our Medicare reimbursement. So finally when they got, you know, they did the MACRA, which got rid of the SGR but what we brought on instead with MACRA is this whole new way of getting reimbursement methodologies and metrics (ie, the MIPS merit incentivized based system) and APMs. So I’m going to talk a little bit more about that.
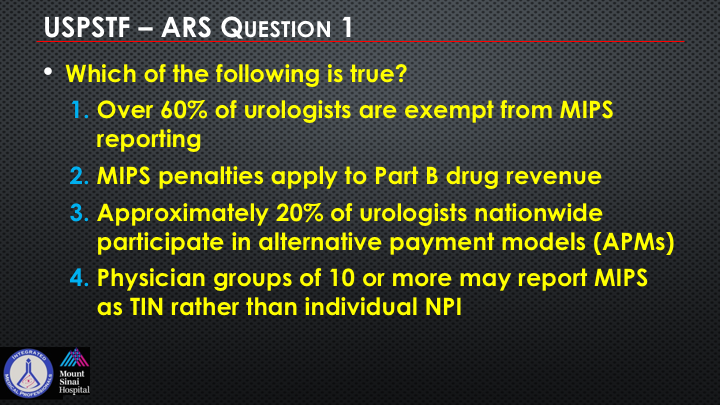
So which of the following is true? Over 60% of urologists are exempt from MIPS reporting. MIPS penalties apply to Part B drug revenue. Approximately 20% of urologists nationwide participate now in APMs. And physician groups of 10 or more may report MIPS as their tax ID number rather than an individual NPI.
Background
So background—why do urologists need an APM? The bottom line why we need an APM is it comes down to reimbursement, pure and simple, and hopefully I’ll be able to explain that to you.
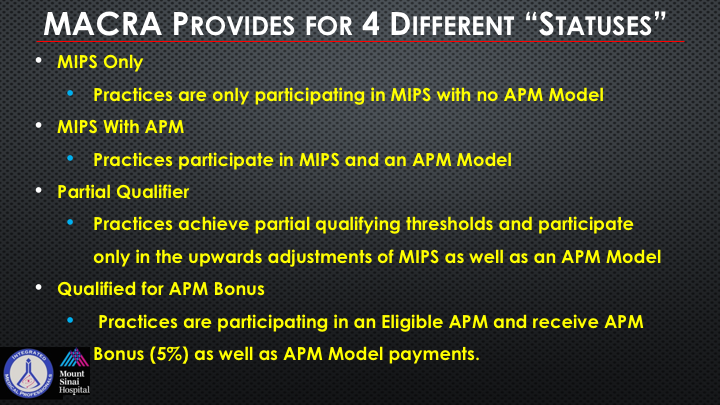
MACRA Provides for 4 Different “Statuses
So MACRA provides these four different statuses so to speak for you and your clinic or your partnership, or your employment. You could be in the MIPS only, where these are practices who are only participating in MIPS and have no APM model. MIPS with an APM are sort of a hybrid, and I’ll show you why these are all relevant as it relates to your reimbursement or lack thereof. There’s a partial qualifier, where the practice is achieving partial qualifying thresholds, and you have some upward adjustments of the MIPS as well as in your APM model, and then you’re in a qualified for an APM bonus, and these are practices that are participating in a true eligible APM, and they receive this 5% bonus as well as the APM model payments.
APM Requirements
So getting back you remember there are these four new metrics that came in with the MIPS that replaced other things such as PQRS, and meaningful use, and value-based modifiers, and so once again there is this whole word salad of acronyms that you have to have a team to help you adjust to and you’re seeing it now a lot—largely in your EHRs.
So CMS estimates that a little over 12,000 physicians, 1.1% in the entire United States, will qualify for an APM in 2017. Mind you, the MACRA legislation came out several years ago, and this is—we’re not making a lot of rapid progress here. Now, why is that important? Well, if you look down at this table, what you are seeing is that in order to get the requirements for this APM incentive, which is where all of the bonus pool of money is, and going from 2017 into 2018, ultimately to 2022, where you are going to receive this and be eligible to receive this is if you qualify for an APM, and right now only two urology practices that I’m aware of in the entire United States are part of an APM.
So CMS estimates that 88 urologists of the roughly 10,000 will qualify as an APM in 2017. So bing, bing, bing light goes on, government is telling you with this chart this is where the bonus pool of money is, and yet we’re being clearly excluded from it.
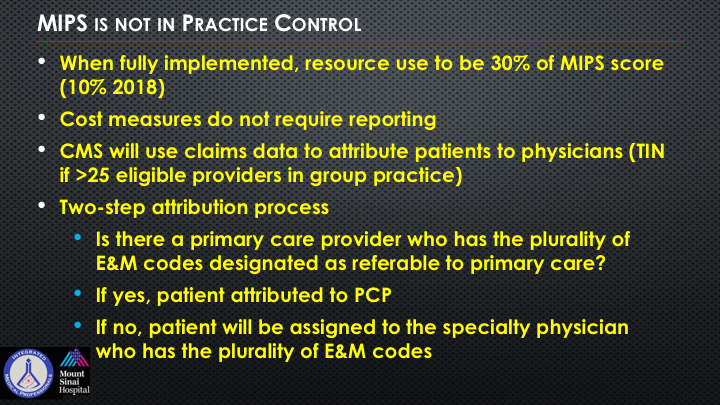
MIPS is not in Practice Control
If you don’t care about it, then none of this will be germane to you, but if you’re running a clinic, if you’re running an academic department, if you’re running a practice, if you’re any one of these things, and you have a lot of employees, these become very important. So when fully implemented, the resource use to be 30% of your MIPS score eventually right now the resource use is the cost that you’re generating. Now, this is all basically comes up as—you don’t report it. This comes through CMS claims data, and CMS will use this to attribute patients to physicians through your tax ID number if you have greater than 25, not 10, greater than 25 eligible physicians in your group. This helps you get to APM reporting. It’s a two-step attribution process.
Now, this attribution process can sometimes, when I’ve heard people talk about it, cause you a sort of deer in the headlights view on it, is who is primarily doing the majority of the patient care? So is there a primary care provider who has the plurality of the ENM codes designated as referable to the primary care? You’d be amazed how many patients you might, if you look at your own data, only come to see you as the urologist, and thus you can get attributable to their total cost of care if you have seen somebody for one, or two, or three urinary tract infections during the year or asymptomatic microhematuria, and you are part of this, and low and behold that same patient who may have other kind of drug-seeking behavior or weird comorbidities ends up hospitalized and getting all of these complications. This person then becomes attributable to you and your group if they’ve not seen anyone else.
So that’s really the final bullet at the bottom one. How do I change it?
MIPS is not in Practice Control
MIPS is not in the practice control. The physician to whom the patient is attributed is assigned all of the cost from that patient, so this now starts to speak to this concept of bidirectional risk or two-sided risk adjustment, which is a big theme of moving the risk away from the payer to the provider (ie, us). So all cost for a patient, in patient, outpatient, ancillary Part B drugs, can be attributed regardless of who provided the service, so if you are the considered the plurality of service and then they go in and have a dissecting aneurysm and you are the attributable provider, that all goes back to your bottom line, and can really affect the cost calculation on a normative curve.
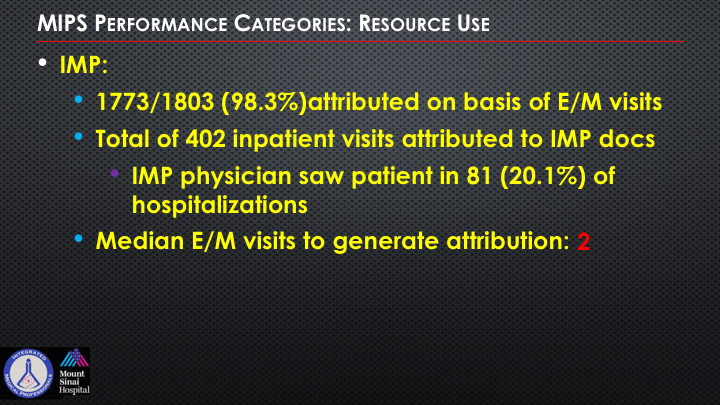
MIPS Performance Categories: Resource Use
So the MIPS performance categories, the resource use, this is the part that they’re looking through in claims data, and it can also be—it’s 98% of it is attributed to ENM visits. This is from Deepak’s own practice, and he looked at his data and IMP, integrated medical physicians, and they saw patients in only about 20% of their actual hospitalizations. So the median number of ENM visits to generate attribution to their practice.
And he actually shared with me in his own personal review, and he’s primarily doing largely administrative work, but he still sees patients, and he had this woman who came in and who he had seen for a few urinary tract infections, relatively uncomplicated, turns out she ended up getting very sick unrelated to anything with the urinary tract, and his score based upon that in his review put him and his group of over 80 physicians as one of the highest resource uses in his group despite the fact that he has one of the lowest patient volumes.
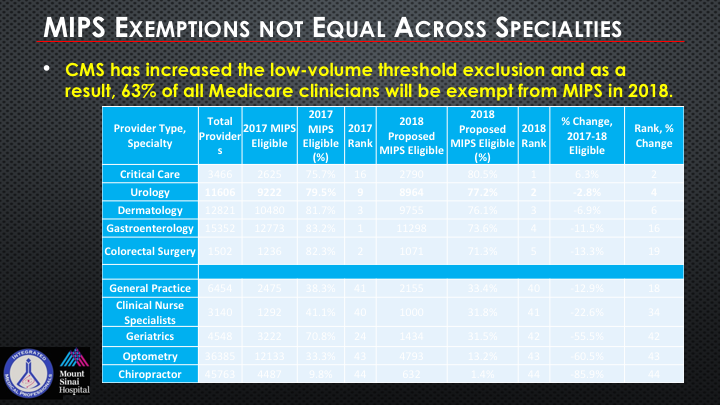
MIPS Exemptions Not Equal Across Specialties
So MIPS exemptions are not equal across the specialties. This is actually just was revised by Deepak prior to coming here so CMS has increased what’s called the low-volume threshold exclusion, and as a result, 63% of all Medicare clinicians will be exempt from MIPS in 2018, but look how high up we are as a specialty as being eligible for the MIPS in comparison to some of the other specialties. So there’s this sort of odd conundrum that we really need to follow up and be cognizant of.
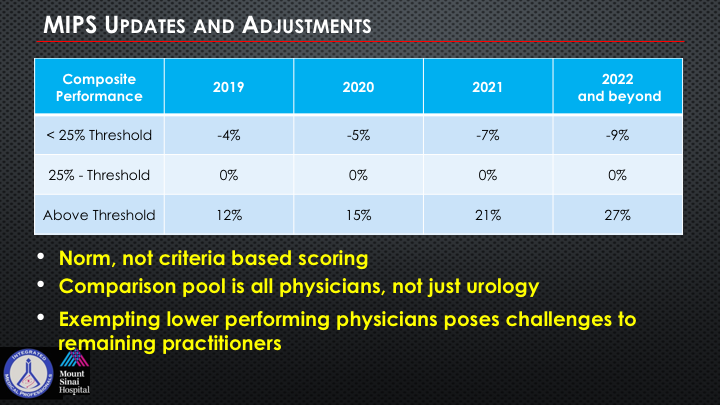
MIPS Updates and Adjustments
Now, one of the things that just came out in all of this was a change in the rule of—and taking a little bit of the teeth out of the penalty and the bonus for this year so that it’s really not going to be as Draconian as it appeared to be. But if some of the updates and the adjustments. So if you’re in this scoring threshold and you get a score for those four different metrics within the MIPS if you are less than this 25% threshold versus 25% to the above, which is vastly increased, they’ve taken a lot of the teeth out of this. And so there’s a small percentage of folks who will be above the threshold for the composite score but even the pool of money, which I think is about $500 million if I’m not mistaken has to be divided amongst all participating physicians.
So it’s normative. It’s not criteria-based scoring. It’s all physicians, not just urology. And there’s a huge exempting of many physicians who pose challenges to so many of us. So we’re being in a big pool with primary care physicians and everybody else.
MIPS Payment Adjustment to Part B Drugs
So this has to do with drugs, and if you’re into systemic therapies, and if you’re giving a lot of oncologic care, just pay attention as you can see to the far right, how if you’re in the penalty situation and you’re giving Part B drugs, and ASP percent as opposed to—and you’re in the bonus pool, so if you’re getting 4.4% because of the sequestration, it’s not really a true 6%, you could get, if you’re in the bonus pool, you could get an additional 11% on say a $100,000 treatment versus getting a negative 3.3%. So in a large practice, whether you are medical oncologists or urologists, and as more and more drug therapies become intermixed in all of our GU oncology, this becomes extremely relevant.
So by 2022, which is not that far off, low performers versus high performers, there’s a huge swing in just Part B drugs alone.
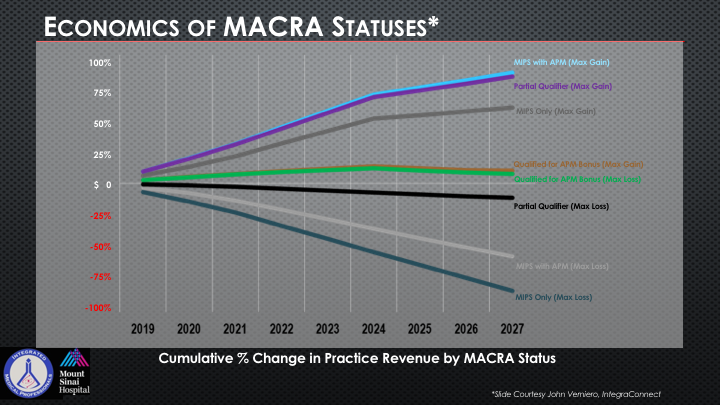
Economics of MACRA Statuses
This is important for our industry colleagues to recognize. Now, this just tells you if you look at the top kind of light Carolina blue color, but MIPS with APM that is your maximum gain. That’s where you’re going to do the best in terms of the economic status and you can see all of those different kinds of categories that I mentioned earlier.
So why am I telling you about this? I’m telling you about this because we at LUGPA put forward an APM this year.
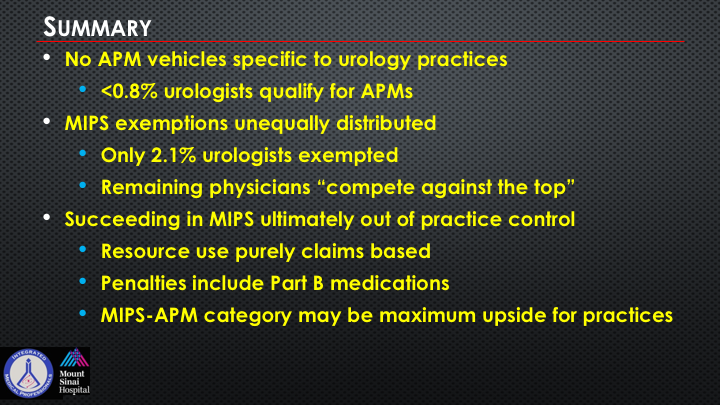
Summary
There are no APM vehicles specific to urology practices right now in the entire country. And less than 1% of urologists qualify for an APM. The MIPS exemption is unequally distributed, only 2.1% of urologists are exempted, only 2.1. The remaining physicians we compete against the top, all of the other top performers. Succeeding in MIPS is ultimately out of your practice control. Your resources are based on claims data. You’ll get penalties potentially under Part B medications if you’re not—if you’re not monitoring your metrics, and it’s the MIPS APM category that has to be obtained, and right now we can’t obtain it because it’s not within accessible reach. So we have put forward an APM at the LUGPA level.
Selection of Disease/Condition
So not every disease and condition is suited for an APM. A big part of the APM for CMMI is they want to see savings. It’s all about savings. Remember we got rid of the SGR. It’s about savings, and it’s about putting the provider at bidirectional risk meaning you can make more money if you do things really well, value—value is outcomes divided by cost, or you can get your clock cleaned if you don’t do it well. You actually can end up losing more money than you had bargained for.
So the characteristics for an APM consideration: treatment costs are meaningful for the payers, and in this specific case, this is CMMI. Numerous treatment options and/or an evolving clinical paradigm. We chose to look at the notion of newly diagnosed patients receiving active surveillance versus active intervention, and treatment variability in clinical practice, which there clearly is lots of variability with intra-practice, inter-practice, intra-, inter-region. Net cost savings if the variability narrowed, and would treatment sequencing be changed. And be able to define quality metrics and outcomes to ensure that the cost savings do not come at the expense of patient care. In other words, let’s just stop ordering tests and therapeutics, save a bunch of money. It can’t work that way. You have to demonstrate quality outcomes.
Scope of APM
So the scope. How many practices or numbers of physicians or other eligible professionals have expressed interest and willingness to participate in the model if it is approved? You have to get support from your specialty, and it has to have applicability to non-Medicare payers. How many physicians or other EPs, eligible professionals, and patients could participate in the model if it was expanded to scale?
So when we proposed ours, and we’re still in the process, it would be open and complete public exposure to the entire universe of your specialty.
Savings Estimates/Shared Savings
The portion of national episode that is reasonable to include in savings estimates, again, this is something that is very carefully reviewed, and so these are big budgetary assessments and a reasonable basis for increase in target utilization based on clinical analytics. And a lot of that clinical analytics requires population health experts, which of course requires resources and spend.
Quality Metrics
Quality metrics—how many? CMS does not provide any guidance. Zero guidance on what the metrics would be. Use existing or develop new ones? Well, there aren’t any so we are now creating these. This is a complete work in progress by multiple different specialties although right now there is, I believe, only about 5 or 6 in the entire world of medicine in the United States that have any APM approval. And this is now going several years into this process. So how do you tie quality performance targets and performance-based payment and repayment?
Pricing Methodology
Well, it’s a very big moving target, and it’s regional versus practice. There can be low-volume thresholds for receive 100% of your regional pricing, and a lot of this will vary, again, depending upon your region as we talk frequently about the heterogeneity of prostate cancer. There’s amazing heterogeneity in how we practice in different parts of the country and sometimes even within counties, and whether to allow the practices to voluntarily accept 100% of regional pricing, this is an ongoing work in progress, and it’s complicated, and so there are low-volume thresholds for applying these floors as well as upper bonuses. So you have stop-loss programming potentially. Very interesting if and when any of these things get approved for us. It brings into a whole notion for those of you who think about insurance or re-insurance methodologies to guard against stop-loss.
Episode Definition
So how do you define an episode? Well, there’s a methodology to attribute the episodes to practice. I alluded to that earlier. There’s a relationship of the APM to other APMs. The classic one right now is the oncology care model where there’s about a $165/member or per patient per month fee to basically do all of the encompassing care for the oncology care process. And a lot is being learned about that. And we actually tried to model our APM off of that with a marked reduction in that fee component.
Monitoring/Auditing
So in the monitoring and the auditing, there has to be monitoring for increased prevalence of prostate biopsy, particularly talking about our act of surveillance, act of intervention, potential APM, and there need to be monitor incentives to either start patients on active surveillance versus not, monitor incentives to keep patients on surveillance even though they should appropriately start an active treatment. And as you can imagine, surveillance, screening appropriately, and intervening or not, thinking about how you now integrate that into an economic business healthcare model has taken on its challenges. This is what we’re trying to address.
Integration and Care Coordination
So how the model would lead to greater integration of care coordination among practitioners and across settings, a completely tabula rasa blank slate moving target. To what extent would the proposed model result in changes in work force requirements compared to more traditional arrangements? Well, in order to do things well oftentimes, as we all know, it can no longer just fall on the shoulders of the clinician. There has to be a coordinated care team, and that includes advanced practice providers. That includes medical assistants. That includes all of the people who have to input in your EHR and take the time to make sure all of these things are being documented accordingly.
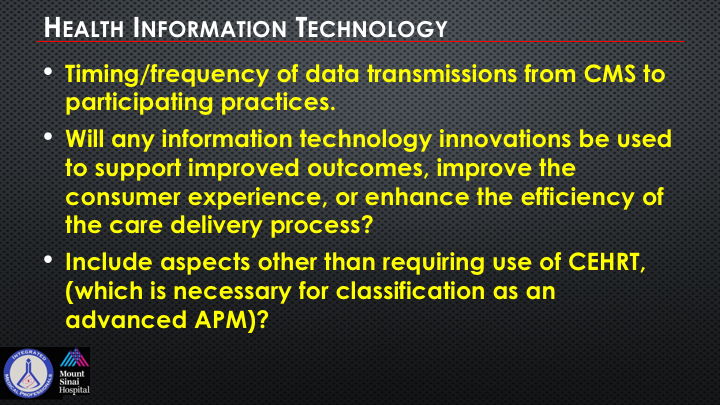
Health Information Technology
So HIT, the timing and frequency of data transitions from CMS to participating practices is a methodological requirement. Will any of these HIT innovations be used to support improved outcomes, improve the consumer experience, enhance the efficiency of the care delivery process? These are the questions that you get asked when we have prevented now to CMMI as well as to PTAC. Include aspects other than requiring the use of the CEHRT, which is necessary for classification as an advanced APM, and of course ECQM as well.
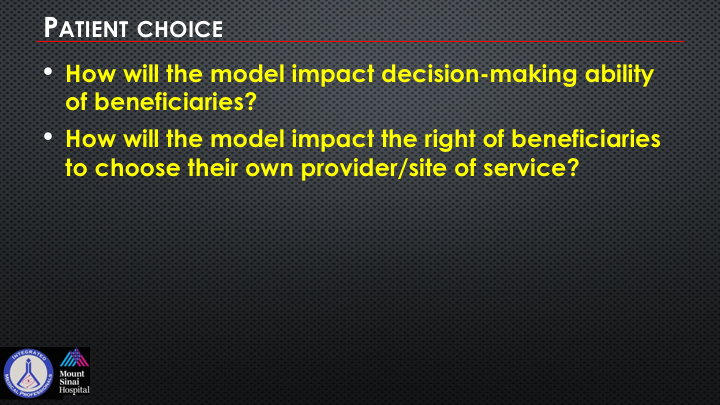
Patient Choice
So the patient choice. I’m hoping that most of you are able to follow a lot of this sort of arcane acronym soup/salad discussion of government health policy, but I think 99.9% of our patients are really clueless to all of this other than they see us come in now with laptops and/or scribes. How will the model impact decision-making ability of beneficiaries, and how will the model impact the right of beneficiaries to choose their own provider and site of services? Well, if you talk to most of your patients, they have no idea that this is going on, but this is what some of the discussion is that’s happening now at MEDPAC and at CMMI.
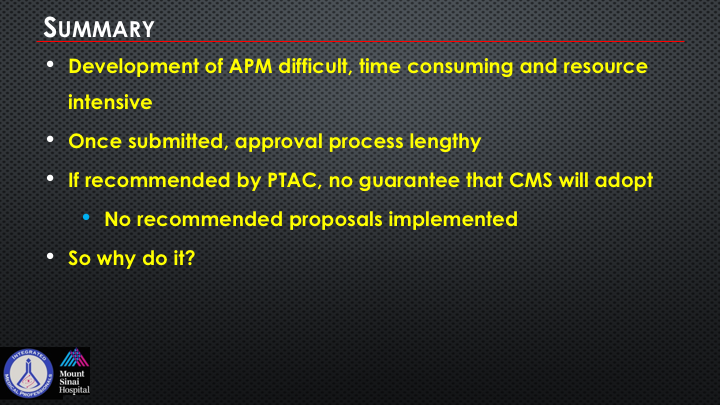
Summary
Even at our APM thing for almost two years now could never have done it without significant industry support, as well as a backbone of a project manager in the form of Integra Connect. This is an enormous process, and it continues and goes on. We actually were very fortunate to get strong support from the AUA and the AACU. So the development of an APM is difficult. It’s time consuming, and it’s very resource intensive. Once submitted, the approval process is lengthy. It’s ongoing. We don’t have a urology-specific APM in this country, and it should be clear to you why it is important for the economics that are in front of us and all other aspects of medicine. If recommended by PTAC, there’s no guarantee that CMS will adopt their recommendation, whether it was positive or negative, and there are no recommended proposals by PTAC that have been implemented to date. So why do we do it, any of us, and why at LUGPA are we doing this?
APM Development
Well, you can just add some Instant Apathy as you see here I think is a funny cartoon from Deepak. Just add whatever, whatever you want, I really don’t care, or as I said earlier, if you’re not at the table, you’re on the menu. And that’s one of the things that were really important to many of us, and frankly to the entire specialty.
ABOUT THE AUTHOR
Neal D. Shore, MD, FACS, graduated from Duke University and Duke University Medical School. He completed his general surgery/urology residency at New York Hospital-Cornell Medical Center/Memorial Sloan Kettering Cancer Center. He serves as the Medical Director for the Carolina Urologic Research Center and is the Chief Medical Officer, Strategic Growth and Pharmacy, GenesisCare, US.
Dr. Shore has conducted more than 400 clinical trials, focusing mainly on genitourinary oncology, and has authored or coauthored more than 350 peer-reviewed publications and numerous book chapters. He serves on the Society for Immunotherapy of Cancer (SITC) Guidelines Committee for Bladder Cancer, as well as the boards of the Bladder Cancer Advocacy Network, Maple Tree Alliance, and the Duke Global Health Institute. He is the Chair of both the Prostate Cancer Academy and the Bladder/Kidney Cancer Academy for the Large Urology Group Practice Association (LUGPA) Specialty Network. He also co-chairs the annual AUA International Prostate Forum. He has served/serves on the editorial boards of Reviews in Urology, Urology Times, Chemotherapy Advisor, OncLive, PLOS ONE, Urology Practice, JUOP and World Journal of Urology, and he also serves as an editor of Everyday Urology-Oncology. He is a Fellow of the American College of Surgeons.