Neil E. Fleshner, MD, MPH, FRCS, presented “Current Findings on High Intensity Focused Ultrasound (HIFU)” at the International Prostate Cancer Update on January 27, 2018, in Beaver Creek, Colorado.
How to cite: Fleshner, Neil E. “Current Findings on High Intensity Focused Ultrasound (HIFU)” January 27, 2018. Accessed Nov 2025. https://grandroundsinurology.com/Current-Findings-on-High-Intensity-Focused-Ultrasound-HIFU/
Summary:
Neil E. Fleshner, MD, MPH, FRCS, explains the basic science of High Intensity Focused Ultrasound (HIFU) for prostate cancer and currently available systems such as the Sonoblate and the Ablatherm. He emphasizes the importance of using this method safely, describing proper patient selection and post HIFU care.
Reveal the Answer to Audience Response Question #1
- A. Between -30° and -40°
- B. Between 50° and 69°
- C. Between 70° and 89°
- D. Between 90° and 99°
- E. Over 100°
Reveal the Answer to Audience Response Question #2
- A. Pubic arch interference
- B. Large prostate volume
- C. Preexisting brachytherapy seeds
- D. Extensive dystrophic calcification
- E. Severe anal stenosis
Answer Explanation:
The answer is Option A. This is not a transperineal delivery, it’s a transrectal delivery. So, the only one that is not a major impediment here would be pubic arch interference. We’re going transrectally, and therefore, that’s not a problem.
(Twitter Question) Reveal the Answer to Audience Response Question #3
- A. It cures everybody
- B. 3% to 7%
- C. 10% to 20%
- D. 35% to 45%
- E. 50% to 75%
Answer Explanation:
The answer is Option D. The precise answer is about 40% and. If you’re going to do whole gland ablation, you need to warn the patient that there is a 40% chance he will have to go back a second time.
Current Findings on High Intensity Focused Ultrasound (HIFU) – Transcript
Click on slide to expand
Current Findings on High Intensity Focused Ultrasound
Just on the way of some disclosures, I have been, along with Dr. Clawson, a variety of other colleagues, we have been running a high intensity focused ultrasound unit for about six or seven years now and I’ll share with you a little of our evolution, but also where we are and for those of you who are not that familiar, I will give you a little bit of a primer on how this all works.
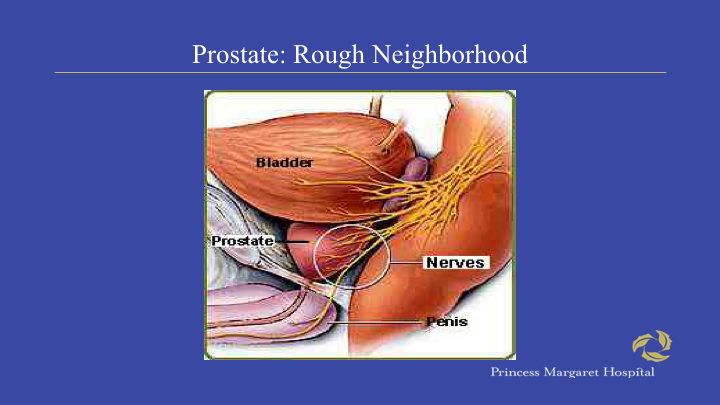
Prostate: Rough Neighborhood
As I usually tell my patients when they have prostate cancer is that the prostate lives in a rough neighborhood, right? You’ve got the neurovascular bundles for sexual function on the side. You’ve got the bladder on top, and you have the rectum behind, and we all know that treating early stage prostate cancer can be associated with morbidity in terms of those three domains of quality of life.
Traditional Radical Therapies Are Not Perfect
And we also know that traditional radical therapies are not perfect. You can see on the left, after radical prostatectomy, at least a third of patients will have a biochemical recurrence and after radiotherapy which uses a different definition, it’s also in the same ballpark, so we all know that surgery and radiotherapy are not perfect and they also have morbidity.
The Perfect Prostate Cancer Treatment
And clearly, what we want to get is the best treatment that will maintain quality of life, particularly sexual function. I think urinary morbidity from surgery in particular is quite low, but we want to balance disease control and quality of life.
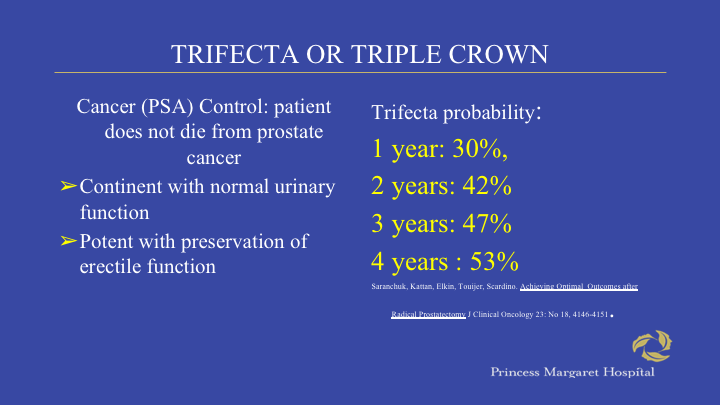
Trifecta or Triple Crown
And ideally, we use the term a triple crown in our clinic. I know Peter Scardino referred to this as the Trifecta, patient cured, potent and continent and the sad fact is, the minority of patients we treat are actually like this. You can see here the data. It’s upwards of 53%, but it’s a highly selected cohort. Many of our men are coming with suddenly impaired or moderately impaired erectile dysfunction and the outlooks for them, particularly with surgery, are not particularly great, at least in my experience.
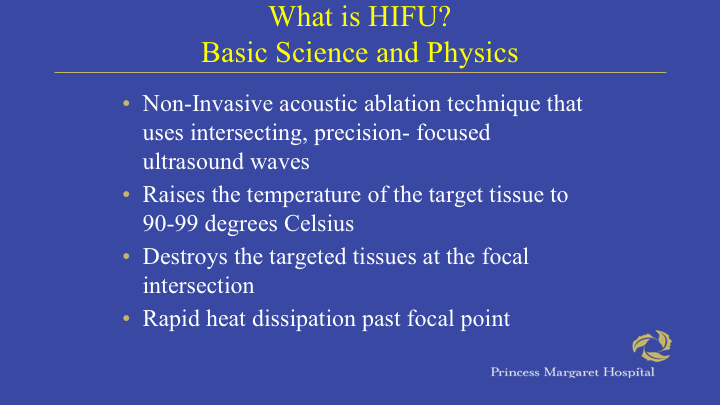
What is HIFU? Basic Science and Physics
So, basic science of high intensity focused ultrasound, this is an acoustic ablation technique. Again, heats the tissue between 90 and 99 degrees centigrade and it destroys the targeted tissue at the focal point.
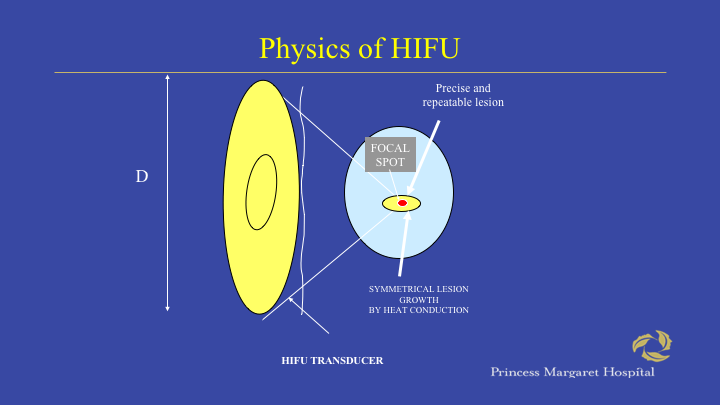
Physics of HIFU
And the best way I could describe this is by some freak of nature when you pass low intensity, sorry, high intensity ultrasound waves through an acoustic lens at the apex. Imagine like a magnifying glass you get intense heat, yet you don’t get heat on the way up towards that apex and that allows you to destroy tissue downstream or deeper than you need to. In this case, it could be done in the rectum.
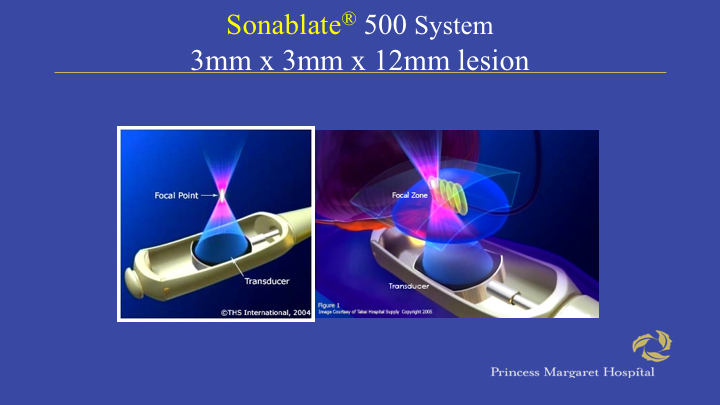
Sonablate 500 System
And this is sort of how it’s done with the Sonoblate machine. I’ll show you there’s a second machine as well, but basically you get these little pixels in three dimensions where you get intense heat at the apex of that particular ultrasound, a focused ultrasound wave.
Time-Temperature Plot
And this is a temperature plot showing what’s happening where you can see that in the actual focal zone you have 98 degrees kill, yet the rectal wall remains fairly cool. Now, it’s very important for you to recognize that this is not a set it and forget it type of machine. You can do a lot of damage with this machine and it requires a lot of teaching.
Two Systems Approved
So, there’s two approved systems. There’s the EDAP machine which is on the left and then there’s the US HIFU machine and the Sonoblate on the right. And in many ways, there are sort of two ways of packaging the same technology.
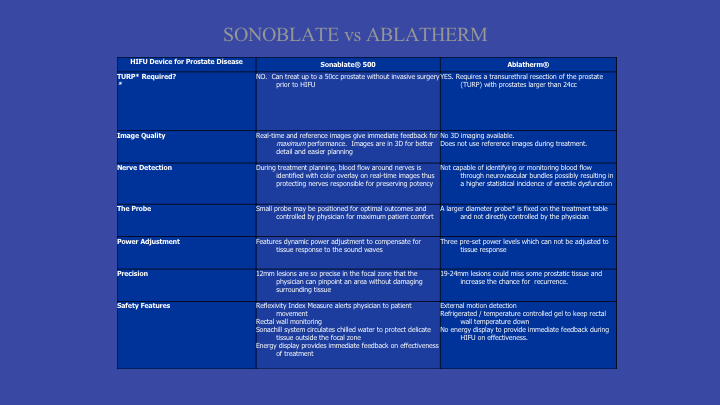
Sonoblate vs Ablatherm
There are subtle differences. The companies would like you to believe that one is particularly better than another, but I’m not sure there’s any solid data suggesting that.
Patient Selection
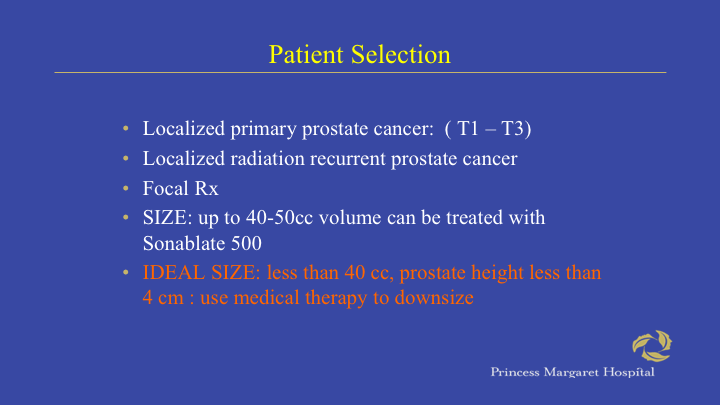
So, of a patient selection. I mean, I think this has evolved, at least in our experience over the years. In theory, you can treat patients with localized disease, patients with locally recurrent disease status post radiotherapy or patients for focal therapy and I will touch on all of these.
Patient Selection
Again, you’d like to have minimal calcifications in the prostate. If you ever see calcifications when you do ultrasound, you get a shadow behind it. If you get a shadow behind it, then the HIFU waves won’t get behind it either. It’s sonographic, it’s the same concept as ultrasound.
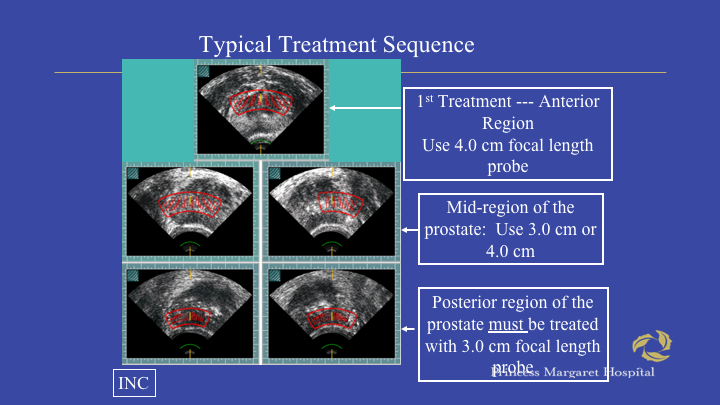
Typical Treatment Sequence
For those of you who have never done this, basically the way it works is you have a transverse image of the prostate, although you do get it as well as a sagittal, and what you do is you start anteriorly in the gland, you map the gland and then you fire the heat treatment. There’s a 4 cm focal length probe and usually you can do the anterior zone or the third floor that way. You often have a second floor which could be done with a three or the four cm probe and then you do the closest one to the rectum and you always must use a 3 cm focal length probe there. The reason you start at the top is very simple. You get a lot of tissue change, edema, and it’s difficult to see above it once you’ve treated it. So, you’ve got to start high and work your way down.
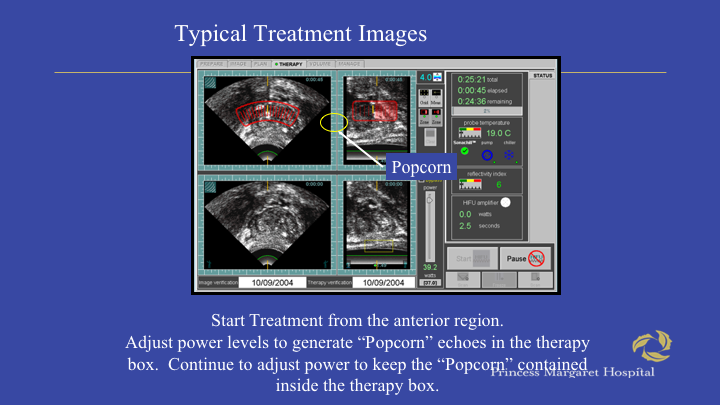
Typical Chemotherapy Images
If you’re really lucky, and in most cases this is true, you could actually see evidence of tissue destruction. It’s called popcorning, so what happens, it’s almost like a kernel popping when you’re at the movie theater and you can see this big white blog. The top is the current image. This is the reference image, so you see you don’t see any white in this particular area, but you see a white blob here and that’s effective popcorning.
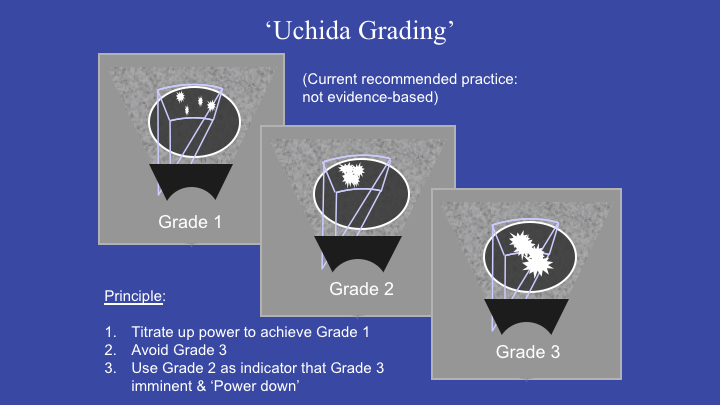
Uchida Grading
And what you would like to see is popcorning within the treatment field and if you see popcorning outside the treatment field, that’s particularly dangerous. You can imagine being on the first floor in the rectal service and if you’re getting this, then you can severely damage the rectum.
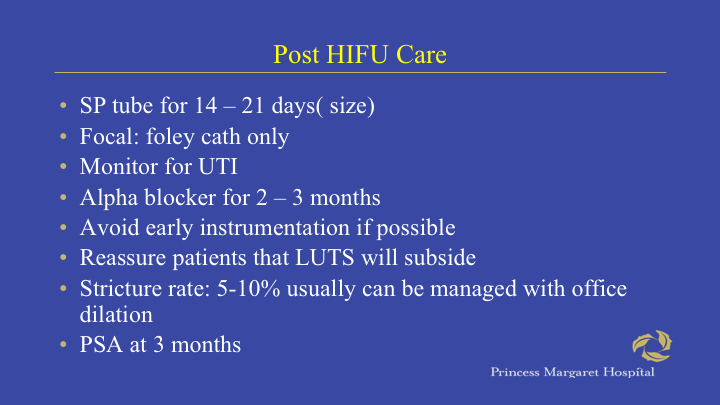
Post HIFU Care
After HIFU, basically patients either have a fully or suprapubic tube depending on if you do whole gland or focal therapy and basically this is how we manage patients fairly stable.
Visually Directed HIFU
There’s a new sort of, if you will, trend towards doing visually directive HIFU.
Visually Directed HIFU: Uchida I/II
And basically, the concept here is to treat and increase the energy, because you can adjust the energy, particularly on the Sonogblate device and you treat until you get popcorning and this has been one of the newer changes to the treatment algorism and it’s been shown in this particular publication at the Nadir PSA values are better with that approach.
HIFU Clinical Results and Data
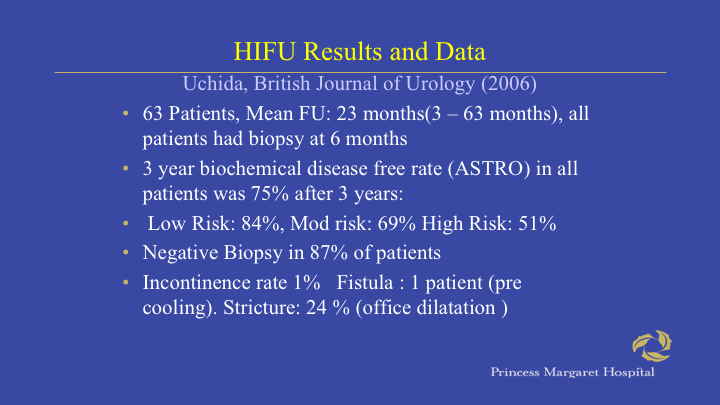
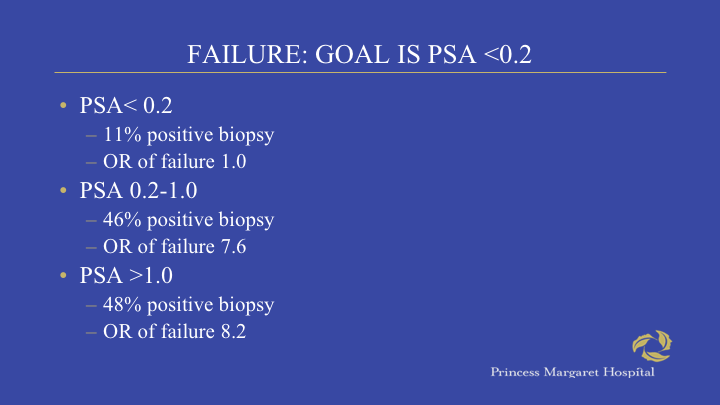
So, how are the clinical results? These are results with whole gland ablation. Just to give you an idea, particularly in Europe and Asia, there are many patients, there are tens of thousands of patients that have been treated with this modality. The key findings, based on the negative biopsy rates and the best series, about 90% probably realistically it’s more around 70 and depending on which biochemical disease free rate equation you use, most are using astro type criteria. It seems to do fairly well in low risk patients and worse as you ratchet it up. There’s not enough well controlled data to tell us how this fares compared to radiation or surgery for sure.
HIFU Results and Data
Here’s a paper from 2006. You can see here that with low risk 84% of patients had negative biopsies, with high risk it was 51% and incontinence rates, however, are rare and I’ll talk about that in a second.
Treatment of localized prostate cancer by HIFU; results of the first French prospective study on patients and previously treated: Minimum of five years of follow up Ablatherm
And I think the key here is that you have to understand that 36% of patients required two sessions and that’s got to be part of the, if you’re going to do particularly whole gland, that’s got to be part of the discussion, but you can see here that basically 75% of patients were considered so-called successful and again, HIFU with a treatment rate of 37%, 39% can typically treat at least half to 75% of the patients without major side effects.
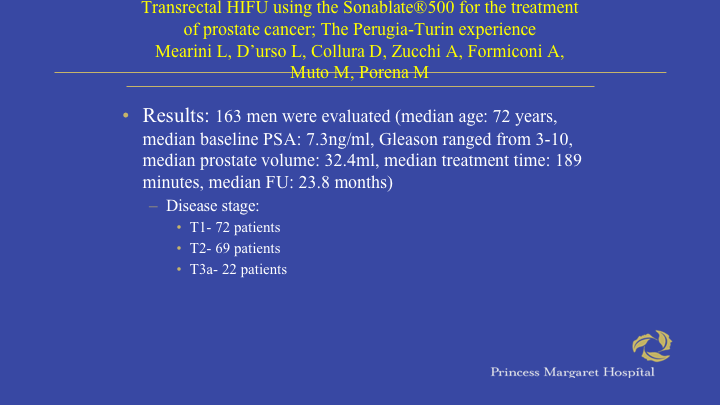
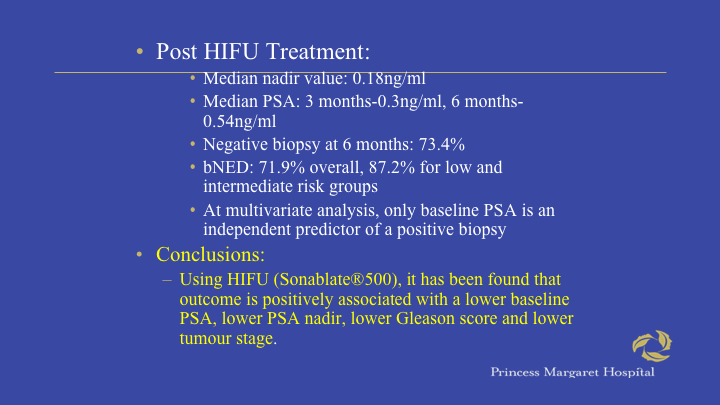
Transrectal HIFU using the Sonoblate 500 for the treatment of prostate cancer. The Perugia-Turin experience.
So, the idea is almost to use this, not that it’s as good as surgery or radiotherapy, I think that’s a silly way of thinking about it. The fact is you can control a sizeable proportion of individuals with less toxicity and these are the Italian data that have come out, 163 patients.
Post HIFU Treatment
You can see their median PSA value was 0.18, negative biopsy rate 73% and they had particularly good results.
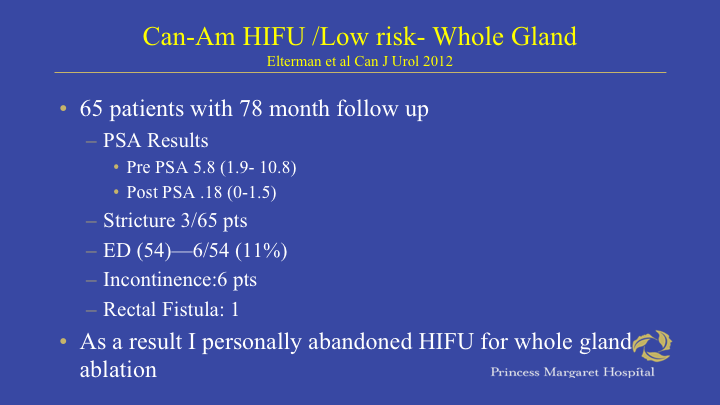
Can-Am HIFU/Low Risk-Whole Gland
This was our low risk whole gland experience that we published some years ago, 65 patients 78 month follow up and you can see that our post PSA treatment, treatment PSA was 0.18. We have about a 3/65 or a 5% stricture rate and ED was quite good at 11%, but we did have one rectal fistula. This is as we were learning and suffice to say we haven’t had one of these in quite a long time. I must admit that personally, as a prostate cancer surgeon, when I saw some of the strictures and that one fistula in particular, I personally abandoned this treatment for whole gland. I no longer do whole gland ablation at all. I only use it now for focal therapy and for the rare radiation failure.
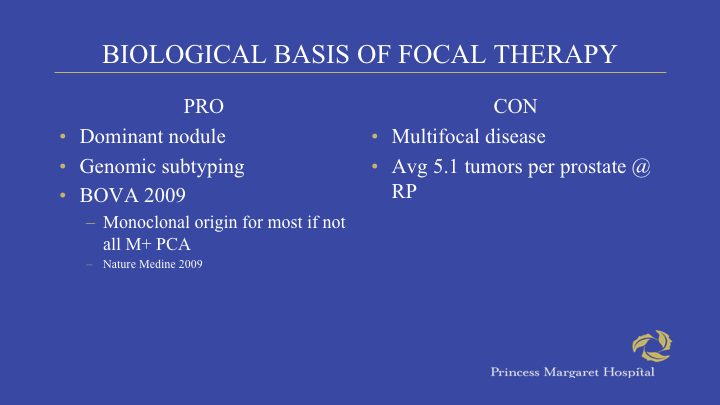
Biological Basis of Focal Therapy
So, let’s talk about focal therapy. We’re all familiar with some of the biologic bases of this and this has been discussed. The pros are concept of a dominant nodule, the fact genotypically that most metastases arise from that area and, of course, the con is that prostate cancer is a multifocal disease.
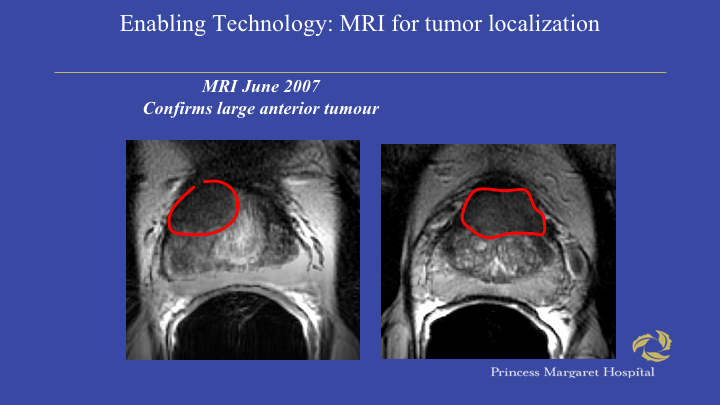
Enabling Technology: MRI for Tumor Localization.
But I think with the evolution of MRI in particular, the last discussion we do have better ways to localize tumors than we did certainly in the pre MRI era.
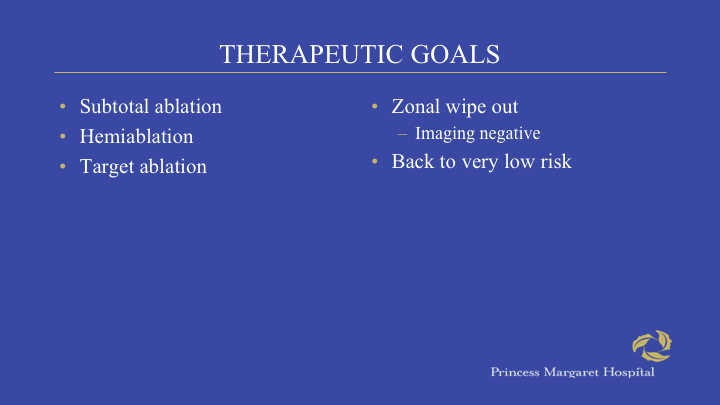
Therapeutic Goals
And, I’ll just go through this. So, what are the therapeuticals? How do we practice focal therapy with HIFU? It’s all over the place to be frank with you. We can do a subtotal ablation, a hemi ablation, we could do a target with an AMO around it in three dimensions and some patients who have, we actually choose to treat only the seven with pre-existing six. The concept is getting them back to low risk. So, there’s a variety of different strategies that you can use around focal therapy, depending on the patient’s desires.
Focal High Intensity Focused Ultrasound Targeted Hemiablation for Unilateral Prostate Cancer: A Prospective Evaluation of Oncologic and Functional Outcomes
And this is probably the most recent one where we could see the results of focal HIFU for unilateral prostate cancer. This was published just in 2016.
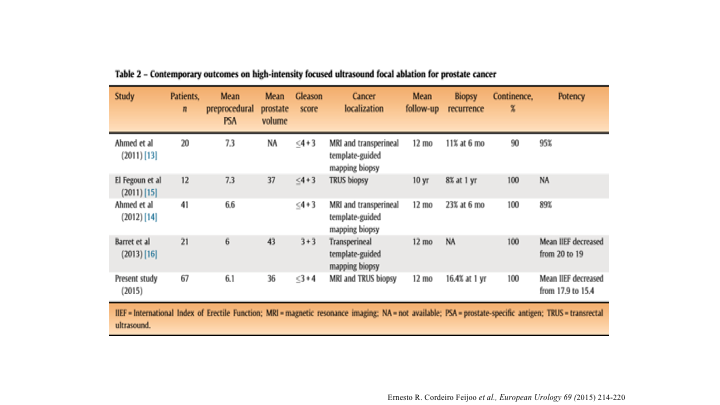
Table 2: Contemporary Outcomes on High Intensity Focused Ultrasound Focal Ablation for Prostate Cancer
And it also shows the literature. Now, I think a couple of things to take home from this, potency results are fantastic. Very few patients are going to have erectile dysfunction, unlike unilateral nerve sparing surgery, that one nerve still gets beaten up a little bit. If you destroy one nerve with HIFU and the other nerve is fine, the patients are fine. The second is the urinary side effects are very minimal. You don’t see the strictures and the contractures when you do focal therapy, probably because there’s blood supply coming in from the other side, but you can see here, when we look at the results of this, you can see biopsy recurrence in the Almed series about 11% at six months, and that’s I think people are starting to see somewhere between ten and 20% of patients have a positive biopsy, but the way to look at it is the compliment. About 80% of patients will have a negative biopsy at at least a year, and there’s also newer evidence that if your MR is clear, you don’t need a biopsy at six months.
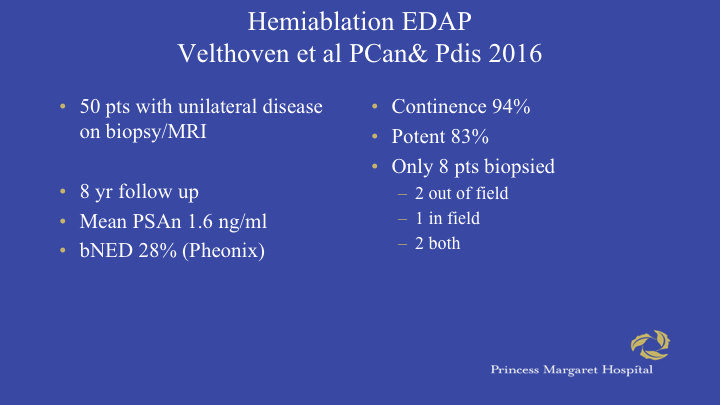
Hemiablation EDA Velthoven et al PCan & Pdis 2016
This is another series. This is using the EDAP machine. You can see there are 50 patients with the unilateral disease, eight year follow up. The bNED rate is 28% using the Phoenix criteria, which is again, it’s actually 72%. That’s a typo. Continence 94% and 83% potent. The problem with this series is very few patients were biopsied and you can see only eight patients of the 50 ended up having a biopsy.
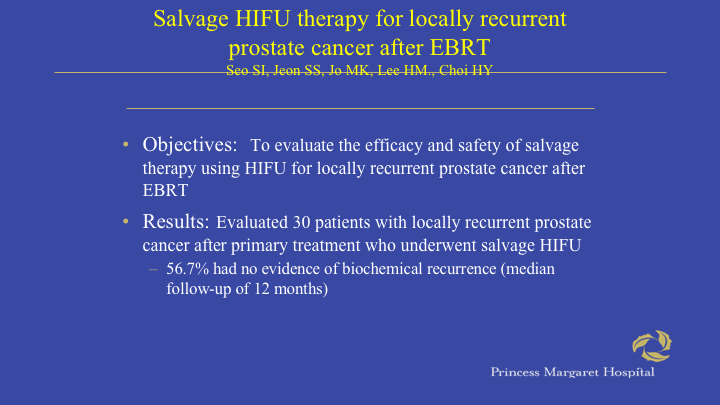
Salvage HIFU Treatment for Locally Recurrent Prostate Cancer After EBRT.
Now, what about salvage? That’s I think the last major indication. Of course, these are troubling patients. Any time you have to apply a second treatment of patients with radiotherapy, the complication rates get ratcheted up. Certainly, seeds are a contraindication. The same reason is because you can’t deliver HIFU up on top of the seeds because they create an acoustic shadow.
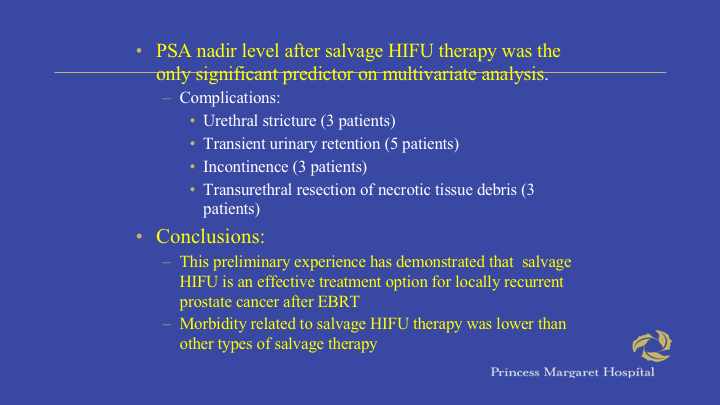
PSA Nadir level after salvage HIFU therapy was the only significant predictor on multivariate analysis
So, basically, if you look at some of the experience in the salvage setting, things you’ve got to worry about, stricture rate, transient retention incontinence and also ischemic sloughing and need for TUR to clean up the prostatic urethra can arise.
New FDA Post Radiation Failures P.I. Herb Lepore
This was the Lepore data and I haven’t heard much follow up on it. These were 200 patients, part of their FDA registration for Gleason 6 and 7, a disease. We were part of this trial. Patients had a six month and one year biopsy and you can see quite respectively, I think here, 63% of patients had a negative biopsy.
Conclusions
So, I’m going to conclude and say that this technology is not perfect. You can do harm with it. You have to be trained on it and we continue to learn and refine our techniques. Look, not all patients are cured, whether we do surgery, HIFU or radiotherapy. Do I think it’s as good as surgery? For sure not, but you can get away with keeping a sizeable proportion of patients well with this technique. Now, whether that’s, and it has to be the right patient who understands that, particularly because of the, in the focal space where morbidity and quality of life is minimally impaired. That’s an outpatient procedure and we need more data clearly and I think the best in occasions as I mentioned is focal therapy and radiation failure. Patients who have large volume disease, Gleason 8 cancers, bilateral disease, don’t offer them this therapy. I just don’t think it’s right.
MR LF-73 year old lawyer
I’ll just share with you one case about some other interesting stuff you can do with HIFU because I have two minutes left. This is a lawyer in my practice. He’s 73. I saw him in November 2015 initially diagnosed in 2004, Gleason 6 2/8 cores, PSA 2.74, had a radical prostatectomy by one of my partners at the time.
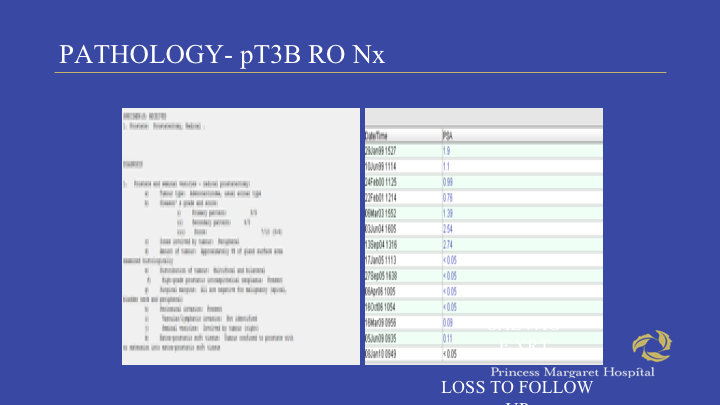
Pathology – pT3B RO Nx
This shows his PSA trajectory but you can see here he initially went undetectable in January 2005, but his PSA started to rise in 2009 and he had salvage radiotherapy and it didn’t work.
Back To Princess Margaret
His PSA started to rise again in a very short sort of response to it. When PSA hit 0.4 not by myself, but he was started on intermittent androgen suppression. Wouldn’t do it typically that long, but he’s a very nervous guy, but he had a horrible time on hormone therapy. He couldn’t walk. Severe leg cramps at night. Couldn’t sleep, depression- and this as a big problem.
Decided to Wait For PSA to Hit 2.4
So I sent them off for a PET scan at the time to Mayo for a choline PET scan and there was basically uptake in his residual seminal vesicle, so for whatever reason they didn’t target during that salvage rate of therapy or just was radio refractory and that was the only spot that was picked up on choline PET.
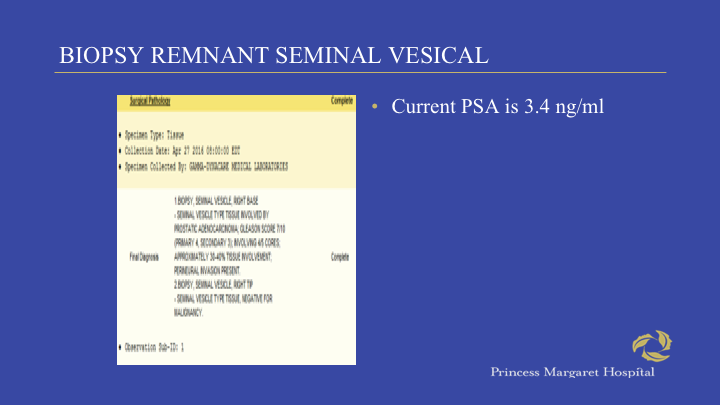
Biopsy Remnant Seminal Vesicle
So, I went and biopsied the seminal vesicle remnant and sure enough, the one that showed some residual Gleason 7 prostate cancer, his PSA is now 3.4. He’s off hormones.
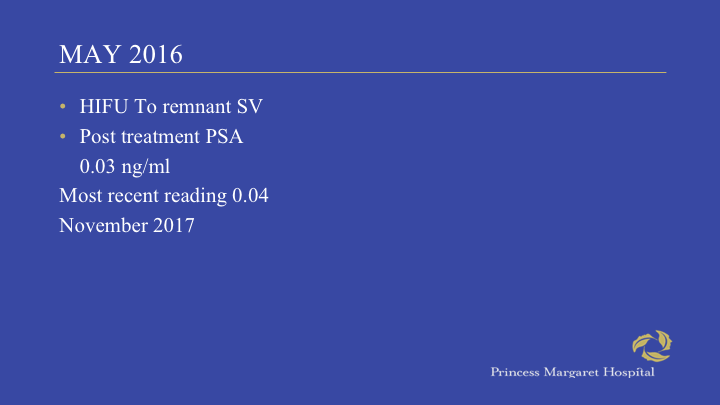
May 2016
So, I actually HIFUed his remnant seminal vesicle. These are the kind of things he could do. And believe it or not, he’s been fine for about three years with a PSA of 0.04, so there’s some other interesting things you can do with this technology. Certainly, surgery for a remnant seminal vesicle. He was offered a radical prostatectomy, a seminal vesiculectomy by robotics at Mayo which I thought after radiation was going to be pretty much a fool’s errand and probably fought with a lot of downside. So, I’ll just conclude that this is an interesting technology. We have to learn more. Please be careful when you use it. If you’re not careful, you’re going to get fistulas and from what I understand, I don’t practice in a litigious environment, apparently a fistula is an automatic lawsuit no matter what you tell patients, so, but again, you can use this technology safely, smartly, and with good effect. Thank you for your time.
ABOUT THE AUTHOR
Dr. Fleshner is a surgeon and clinician scientist and an established leader in the field of cancer prevention. He is a Professor and the Chair of the Division of Urology at the University of Toronto. Additionally, he is Head of the Division of Urology at the University Health Network and Princess Margaret Hospital in Toronto, Canada, and holds the Love Chair in Prostate Cancer Prevention at Princess Margaret Hospital. He is also affiliated with the Mount Sinai Health System in New York City.
Dr. Fleshner earned his MPH degree from the School of Public Health at Columbia University and completed his oncology training at Memorial Sloan Kettering Cancer Center. He has achieved international renown as a talented cancer researcher who has made significant contributions in the field of urologic oncology. His research priorities include translational, clinical, and health services research, focused primarily on understanding of prostate cancer pathogenesis, progression, and prevention. In addition to his clinical, academic, and research commitments, he heads the University Health Network GU BioBank, a central data and specimen repository designed to support the use of biological fluids in disease discovery, prognostication, and management. He has authored over 450 scientific papers and is a sought after speaker, both locally and internationally.