E. David Crawford, MD, presented “Is MRI Fusion Biopsy the New Gold Standard of Diagnosis? Con Argument” during the 28th Annual Perspectives in Urology: Point Counterpoint on November 15, 2019 in Scottsdale, Arizona.
How to cite: Crawford, E. David. “Is MRI Fusion Biopsy the New Gold Standard of Diagnosis? Con Argument” November 15, 2019. Accessed Mar 2026. https://grandroundsinurology.com/is-mri-fusion-biopsy-the-new-gold-standard-of-diagnosis-con-argument/
Is MRI Fusion Biopsy the New Gold Standard of Diagnosis? Con Argument – Summary:
E. David Crawford, MD, argues that MRI fusion-guided biopsy should not be the gold standard of prostate cancer diagnosis. He cites MRI’s limitations in detecting clinically significant cancers and predicting extracapsular extension and tumor volume, as well as the existence of new technologies such as micro-ultrasound, in this point-counterpoint debate.
The “pro” rebuttal to this presentation is “Is MRI Fusion Biopsy the New Gold Standard of Diagnosis? Pro Argument” by A. Karim Kader, MD, PhD.
Abstract:
Though MRI is a valuable imaging tool for screening and targeting, this modality has significant limitations. In a retrospective analysis of the correlation between MRI results and whole-mount prostatectomy pathology, MRI did not perform well in predicting the number and volume of tumors and missed 25% of cancers with Gleason scores higher than 4+3. Furthermore, MRI missed 17% percent of clinically significant solitary lesions and has a false positive rate of 19%. MRI performs poorly in predicting extracapsular extension, even when conducted at excellent imaging centers with world-class technology and radiologists. Also, MRI typically underestimates tumor volume.
Because of these limitations, even after the well-known outcomes from the PROMIS and PRECISION trials, which were favorable to MRI, guidelines still acknowledge that false negatives can occur when using MRI to guide biopsy decisions, and therefore standard transrectal ultrasound biopsy should still be considered. MRI alone is also not adequate for planning and conducting focal therapy.
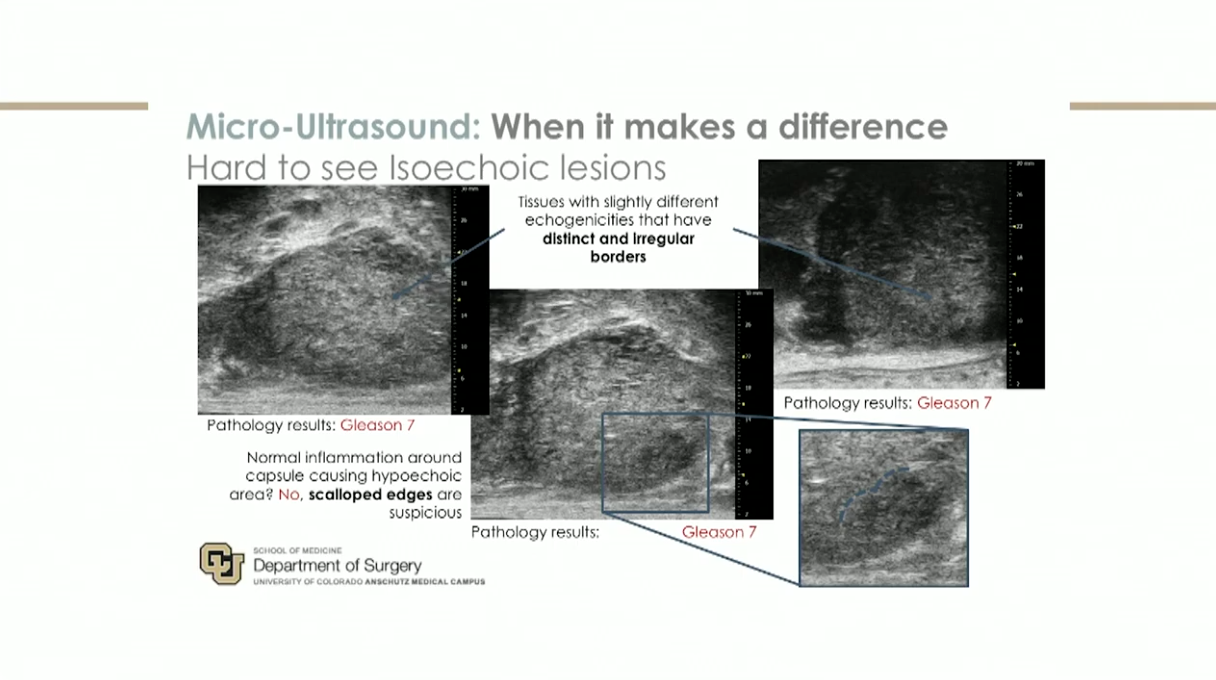
A technology that could perform better in this stage of the diagnostic pathway is a novel 29 MHz micro-ultrasound system, which allows for real-time visualization and targeting while conducting a biopsy. Compared to MRI/ultrasound fusion biopsy, micro-ultrasound has significant advantages, such as cost, inter-reader variability, and workflow complexity.
While MRI is a useful tool, due to its disadvantages relating to visualization and detection and the existence of better technologies, it should not be the gold standard in prostate cancer diagnosis.
About Perspectives in Urology: Point Counterpoint
Perspectives in Urology: Point Counterpoint (PCP) is an annual, multi-day, CME-accredited conference devoted to discussing and debating the latest topics in men’s health and general urology, as well as management of bladder, renal, and both localized and advanced prostate cancer. More than didactic lectures, the conference’s format includes debates, point-counterpoint discussion panels, and unique case-based presentations. Dr. Crawford presented this lecture during the 28th PCP in 2019. Please visit this page in order to register for future PCP meetings.
ABOUT THE AUTHOR
Researcher-physician E. David Crawford, MD, Jack A. Vickers Director of Prostate Research and Professor of Urology at the University of California, San Diego, has devoted his career in medicine to educating the public about men's health issues and finding effective techniques and procedures to address prostate cancer, the most common malignancy affecting men in the United States.