Richard G. Stock, MD, presented “Long-Term Outcomes of Permanent Brachytherapy” during the 23rd Annual Southwest Prostate Cancer Update on April 15, 2018 in Scottsdale, Arizona
How to cite: Stock, Richard G. “Long-Term Outcomes of Permanent Brachytherapy” April 15, 2018. Accessed [date today]. https://grandroundsinurology.com/long-term-outcomes-of-permanent-brachytherapy/
Long-Term Outcomes of Permanent Brachytherapy – Summary:
Richard G. Stock, MD, compares long-term overall survival and morbidity outcomes of brachytherapy alone versus a brachytherapy/ external beam combination in intermediate and high risk prostate cancer. He also discusses factors that could affect those outcomes, such as the patient’s intermediate-risk features, duration of androgen deprivation therapy (ADT), and technique of seed implantation.
PSA Doubling Time as a Predictor of Metastasis Development and Overall Survival
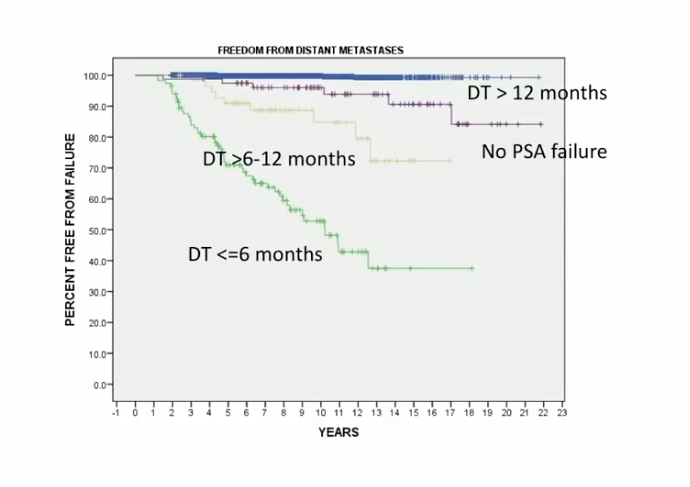
Between 1990 and 2015, Dr. Stone and a research group observed PSA doubling time following low dose rate (LDR) brachytherapy in patients with localized prostate cancer. The study separated patients into those who had a less than 6 month doubling time, a 6-12 month doubling time, a doubling time more than 12 months, or no PSA failure at all. Results showed that an insignificant amount of patients developed clinical metastatic disease without a rise in PSA. Also, no patients with a 12 months or longer PSA doubling time developed metastases within 20 years following initial treatment. The 6-12 month and less than 6 month groups and had increased risk of developing metastatic disease within 15 years.
Additionally, this study suggested an association between short PSA doubling times and decreased overall survival.
This data supports a concept of PSA doubling time as an indicator of brachytherapy outcomes. Because of this concept, Dr. Stone stresses that physicians should utilize novel therapies for metastatic and castration sensitive disease in patients who have short PSA doubling times, but have not yet manifested metastatic disease.
Long-Term Outcomes in Intermediate Risk Patients
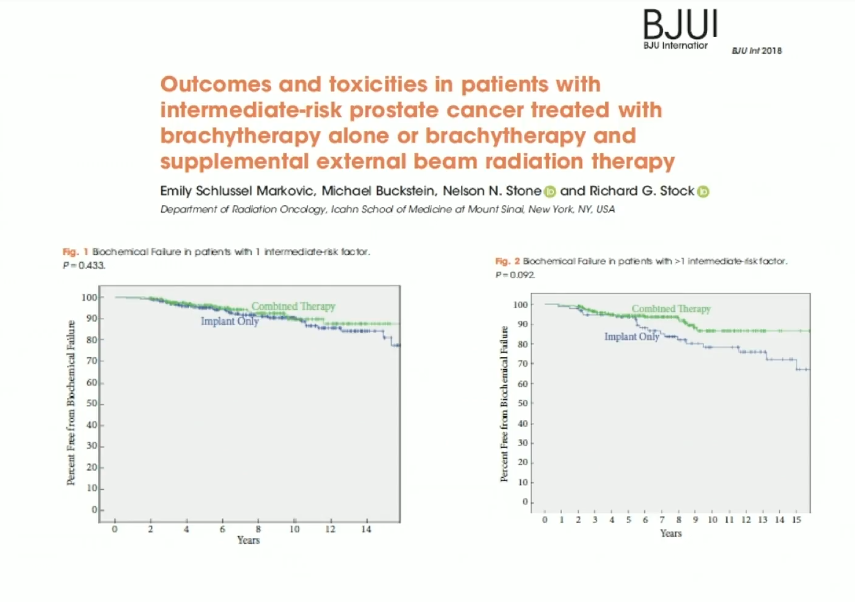
The NRG Oncology/RTOG 0232 phase III trial compared an external beam and brachytherapy combination with brachytherapy alone in intermediate risk-patients. Results suggested that in patients with one intermediate-risk feature, there was not a significant difference between the combination and monotherapy.
The RTOG 0232 trial focused primarily on patients with only one feature. Therefore, Dr. Stock saw the need to investigate brachytherapy alone versus combination therapy in patients with more than one intermediate risk feature. He and a research group conducted a later study addressing this need. The study also observed toxicity and PSA doubling time, to further understand patient outcomes.
The results of this study showed similar results to the RTOG 0232 study. However, patients with more than one risk feature showed improvement with combined therapy. The figure to the left compares biochemical failure in patients with one intermediate risk factor and multiple intermediate risk factors.
While this improvement was not statistically significant, Dr. Stock advises physicians to consider combination therapy when treating patients with more than one intermediate risk feature.
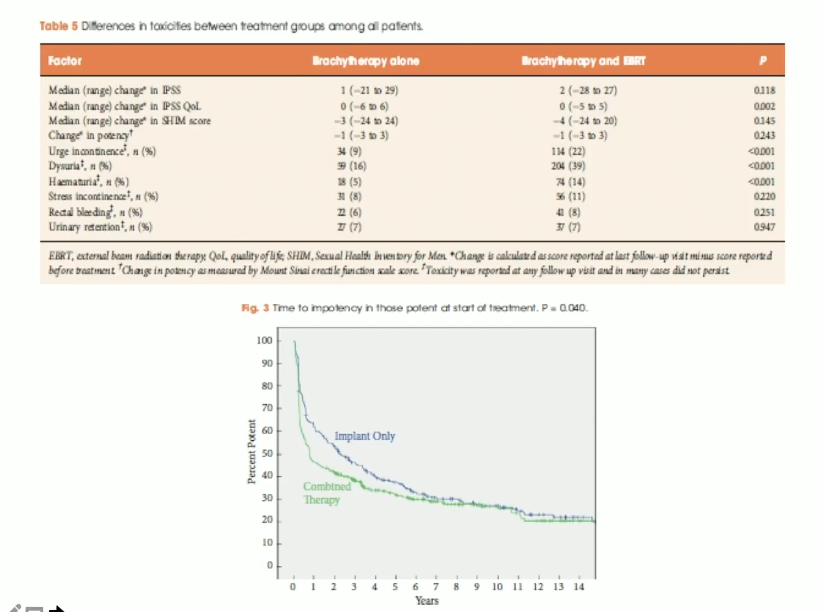
Although biochemical failure data from this study was not dramatically different from the RTOG 0232 data, the toxicity data was quite revealing. Notably, there was a higher incidence of patient-reported urge incontinence, dysuria, and hematuria in the combined treatment arm than in the brachytherapy alone arm. Also, this study suggested adding external beam to brachytherapy significantly decreased potency preservation compared to an implant alone. With this data in mind, Dr. Stock’s advises physicians to treat intermediate risk patients with brachytherapy alone when possible.
Overall Survival Following Brachytherapy: Impact of Hormone Therapy Combination
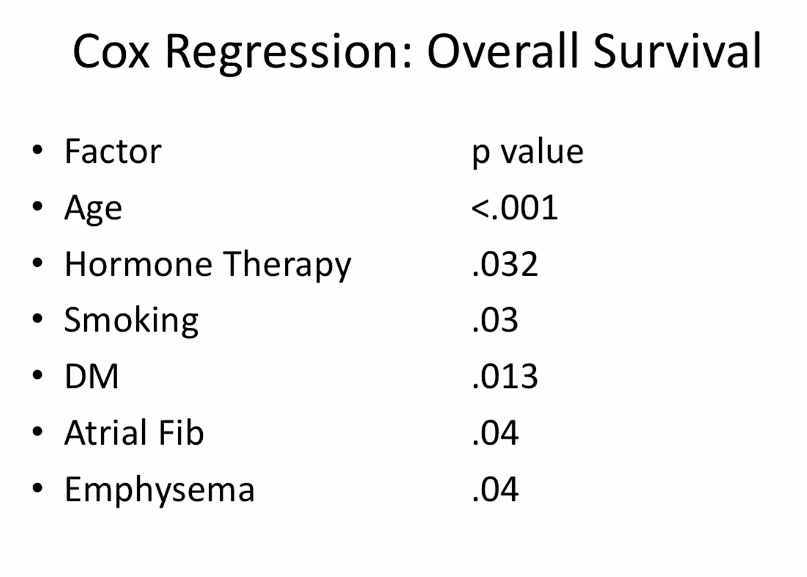
Another study by Dr. Stock, Nelson N. Stone, MD, and others observed specific and all-cause survival in prostate cancer at 15 years following brachytherapy. It separated patients with less or more than 6 months of ADT. Results showed that patients with longer-term ADT had significantly lower all-cause survival. The Cox regression analysis from this study also shows that hormone therapy is a major factor in reducing the likelihood of long-term overall survival.
Treating Higher Risk Patients
A JAMA study released in March 2018 collected patients with Gleason scores from 9-10. It broke patients into those receiving external beam alone compared to external beam plus ADT, those receiving radical prostatectomy, as well as those receiving external beam and brachytherapy with or without ADT. Results showed the adjusted 5-year prostate cancer specific mortality rates were 13% for external beam, 12% for radical prostatectomy, and a much lower rate of 3% for combined therapy. The distant metastases rate was also significantly lower in the combined modality treatment arm.
Dr. Stone notes that the brachytherapy plus external beam arm had a shorter duration of ADT than the external beam alone arm. Despite this, the combination therapy arm still did statistically better.
Randomized Trials
Biochemical progression free survival data from the toxicity reports in the ASCENDE-RT trial suggest a significant improvement for patients who revieved external beam and an implant. In high risk patients, there is about a 20-30% improvement of biochemical control with the addition of a seed implant.
However, according to the morbidity analysis of ASCENDE-RT, there were statistically significantly higher genitourinary toxicities in the brachytherapy and external beam arm. Multiple editorials have attested that, based on this data, external beam alone should be the standard of care in this setting. Dr. Stock argues against this, claiming that proper brachytherapy technique can mitigate this observed morbidity. He explains that physicians using pre-plan needles to place seeds beyond the prostatic apex leads to strictures and morbidity. A technique involving longitudinal imaging may reduce this toxicity in the future.
ABOUT THE AUTHOR
Richard G. Stock, MD, is a Professor of Radiation Oncology and Director of Genitourinary Radiation Oncology at the Icahn School of Medicine at Mount Sinai in New York City. He has dedicated his career to delivering the highest quality care to patients using the most advanced technology available, including intensity modulated radiation therapy (IMRT), Novalis Shaped Beam Radiosurgery, real-time ultrasound guided prostate seed implants, and MammoSite, all of which allow him to meticulously target tumors while achieving maximal sparing of normal tissues.
Dr. Stock has served on the board of American College of Radiology Testing and the American Brachytherapy Society, where he is member at large, and as guest editor of a special Brachytherapy issue of Techniques in Urology. He has lectured and presented at dozens of meetings and symposiums across the country and internationally, including in New York, San Francisco, Chicago, Philadelphia, Boston, Spain, Holland, France, and Japan.
Dr. Stock completed his internship at Beth Israel Medical Center and his specialty training at Memorial Sloan-Kettering Cancer Center. He is listed in America's Top Doctors.