Chris Gonzalez, MD, presented “Management of Lichen Sclerosus Related Urethral Strictures” at the Jackson Hole Seminars on February 7, 2018 in Jackson Hole, Wyoming.
How to cite: Gonzalez, Chris. “Management of Lichen Sclerosus Related Urethral Strictures” February 7, 2018. Accessed Jan 2026. https://grandroundsinurology.com/Management-of-Lichen-Sclerosus-Related-Urethral-Strictures/
Summary:
Chris M. Gonzalez, MD, MBA, FACS, defines the prevalence of lichen sclerosus related urethral strictures in men and other common risks. He explains best practices for managing the disease in order to reduce complications and recurrences, and to improve urinary and sexual function outcomes.
Management of Lichen Sclerosus Related Urethral Strictures – Transcript
Click on slide to expand
Lichen Sclerosus
So, lichen sclerosus, what was formerly known as BXO. We call it lichen sclerosus now because we’ve advanced into that era, and that’s technically the correct term. So, it’s a chronic, progressive, inflammatory disorder of the skin. Unclear underlying etiology. It’s been linked to everything from infections, to autoimmune disorders, trauma, genetics. We’re not really quite sure what causes it. Bereli Buruli has been implicated in this. Most commonly involves the genital region and associated with urethral stricture. So, this affects women about 10x more than it does men, and of all of the men that get lichen sclerosus of their genital skin, about 7% to 10% will get a urethral stricture. Overall prevalence is controversial. Usually see it in younger, white men, anywhere between 1 in 300, to 1 in 1,000.
Lichen Sclerosus #2
So again, just shows that we really don’t understand 100%, even the demographics of this. So, we did a case control study showing that men with LS have a higher BMI, coronary artery disease, diabetes, and tobacco use. So really, the profile of a man that we notice that came in was somebody who was obese, concealed penis, and had all of these particular issues. Erickson and colleagues came back a little bit later with different institutions and said, “Yeah, we agree with that,” and wrote pretty much the same paper. But really I think – I’m not sure if we can say it’s a systemic disease. It just means – this is just who presents with it. Really, I think the question becomes, “What is the infectious etiology of this?”
So, we’re doing microbiome studies right now at Case trying to take a look at this. We have a few ideas, but I think there’s a lot more work that needs to be put into this. And then, there’s also this concept of it starts at the meatus and works its way back through the glans of the urethra. We never really believed that, so we went back and looked at our isolated bulbar strictures at Northwestern. And we found 70 patients. We had all of the tissue blocks for them, and we found, when we looked at the tissue blocks with our pathologist, that nearly half had features consistent with LS, isolated LS, which makes absolutely no sense. So, this whole distal to proximal progression, we proved we don’t – we don’t think that is really what is going on. So, there could be a trauma phenomena, a Koebner phenomenon, but again, just again shows that we don’t know.
LS at a Young Age
So, if you take a look, it presents very, very early. This is a young child about to undergo circumcision. For those young boys that get a circumcision and have LS in the path specimen, about one in five will need another operation for meatal involvement, or it comes back on the skin. So, it’s a real disease. And this is something we all probably see in our clinics. Right?
Concealed Penis
So, a lot can be told from this particular story. You know, this individual has a concealed penis. See how high the scrotum is here. Probably had too much skin taken off at circumcision at birth, which is another problem, which led to the concealed penis but that redness, irritation, pruritus, all of those things, it really drives people crazy. So it’s a real problem.
Initial Evaluation
So, I’m going to put some guidelines in here that are appropriate, from the AUA guidelines, on stricture disease. One of the guidelines was clinicians may perform biopsy for suspected LS and must perform biopsy if carcinoma is suspected. So, you can take a look at it and say ah-ha, LS, like that greyish white appearance for that young boy, but for somebody who has disease that’s more suspect, do a biopsy. Just get a little piece of tissue to be sure. Squamous cell carcinoma has been reported in anywhere from 2% to about 9% of cases. So this is real, and the same thing in the vulva with women. It’s the exact same thing that happens. So, Baird Carlson [phonetic] was a really talented medical student at Northwestern, and you know it was my great mentorship with him, and he went into orthopedic surgery. We couldn’t get him to go into urology, but anyway, he did some good work for us. He went back and looked at all of the literature that’s out there. He found some pretty interesting things. He found that p53, a tumor suppressor gene, is over expressed in lichen sclerosus, and also in squamous cell carcinoma in that area. Ki-67, which is a proliferative marker of cell growth, is also over expressed. p16 was overexpressed and implicated with HPV. That was also found in penile squamous cell carcinoma, and angiogenesis markers of VEGF and cyclooxygenase 2 were found in vulvar lichen sclerosus and squamous cell carcinoma. So, looking for protein markers or how to determine indolent versus malignant disease. These are the kinds of things that I think are going to be what we need to push the envelope on, and obviously, urethral involvement. Cystoscopy, retrograde urethrogram to figure out how far back does this go in the urethra.
Lichen Sclerosus as Progressive Squamous Cell Carcinoma
Here’s an example. I mean, I hope we don’t see these things, but if we do, I think we all know what we need to do. This is classic lichen sclerosus as progressive squamous cell carcinoma. So, this person is in for quite a bit of surgery after we made the diagnosis. So, these are the things we have to look out for. If you have a concealed penis, get it unconcealed. If you have to go to the OR to get it unconcealed, do it, because we pulled out squamous cell carcinoma in more than one situation. So again, please do that. These guys will bounce around until somebody actually makes a diagnosis. So, what about topical steroids?
Medical Management
What about topical steroids? Well, they are the mainstay of cutaneous medical therapy. The optimal topical steroid regimen has not been defined. We give it to them twice a day for a period of a few weeks. Some people do it for three months. The bottom line is, no one steroid works better than others. So clobetasol, betamethasone, mometasone, hydrocortisone – they all work the same. A lot of studies in vulvar involvement and also in genital skin and nails. So, there is really not one optimal treatment regimen. I will say it’s pretty much temporary. It will go away while they’re on steroids. Comes right back after a while, at least I find, with cutaneous disease.
Medical Management #2
So, what about intraurethral clobetasol for biopsy-proven LS? This is actually pretty interesting. This is Drew Peterson‘s work, and I think it’s very good work. He found some men that didn’t want to undergo urethroplasty. They wanted to try and temporize this and treat this with intraurethral clobetasol, so they could have had a distal stricture, or it could have been farther up in the bulbar urethral. They coated the dilator. They coated the catheter with clobetasol, and they’d suck it in there twice a day for about three months, at least three months, some went out to six months. But, then they kind of decided how they were going to taper it off. And he found of all those patients, at about two-year follow up, that most did not progress to surgery or urinary retention. Now, there is a subset of these patients that started out that needed Drew to go back to the OR and open them up to begin with. That’s how bad the strictures were, so there is some kind of a temporizing mechanism that could be associated with the dilation, but also with the steroids. Again, two years that hold temporary effect. I think this needs a little bit more work. I’d be more impressed to see at five years and no catheterization what happens to these individuals. So, I think that we should encourage that kind of data to be looked at, because there may be something here.
Medical Management #3
Other options for medical management, topical tacrolimus, topical testosterone, oral acitretin. This stuff is pretty toxic, at least in men. Testosterone does have some effect in vulvar lichen sclerosus, but again, steroids, and there is no one steroid that works better. So, these can be offered, but they are probably not going to give you any advantages in your male patients. So, something to keep in mind.
Surgical Management
So, what about surgical management? And, that’s something that we should talk about. We all see this in our office. So, when LS is combined to the preputial skin, circumcision is associated with a 92% cure rate. So, you want to make sure there is no urethral involvement. Even if there is meatal involvement and the guy is peeing okay, let him alone, because generally when you diagnose LS or you see it in the urethral, if you’ve got enough of a caliber for the individual to pee and they’re not having any problems, I would not go in. You are not going to make it any better, or any bigger, or any wider, so just let it be. Many times, it will just stay that way, and I’ve had patients in my practice for 10 or 15 years. But you’ve got to keep an eye on it. If it does recur following circumcision, the one thing you don’t want to do is a repeat circumcision, because that goes down a certain pathway that is not good for the patient or good for the doctor.
Split Thickness Skin Graft
And here is an example. I’m sure we’ve all see this before. Kind of a bigger guy. Had a circumcision. Now, I can’t get it exposed. You’ve got the cracking, the markings, the pruritus. This person is absolutely miserable. You do not want to do another circumcision on him. We get these folks sent to us, and generally, what these folks need is something pretty extensive.
Split Thickness Skin Graft #2
So, what we will do is we will excise all infected tissue, which is a principal of lichen sclerosus surgery, to get rid of as much tissue as you possibly can, right down to the scrotum. We will pex that penile shaft right down there to the base of the scrotum, and then we will get a split thickness skin graft. I was talking to Doug Houston from Mayo. He said they use buccal mucosa around that mucosal collar right there. It actually works pretty well. I haven’t tried that before, but that’s actually interesting. That split thickness skin graft, these guys are happy. They can see their penis. You can examine them, and if and when it comes back, you can do something about it. So again, be really careful with those folks with a concealed penis and lichen sclerosus.
Extended Meatotomy
Another thing to think about is extended meatotomy. So this is something that is more of an aggressive meatoplasty. So distal strictures involved with LS extending from the meatus into the fossa navicularis. Okay. We’ve got to take buccal mucosa. We’ve got to do all of these things. The patient is like, “Oh boy,” you know, so informed consent with the patient. You may have some spraying. You may have some loss of voiding control. The appearance is going to be different, but they actually do really, really well. Al Morey showed us this, and in our experience too following, what Al was telling us, we think it works pretty well too. So, in mean follow-up at 38 months, these people were actually happy. They’re the happiest people when you wake them up in the recovery room saying, “Hey, we didn’t have to take the buccal mucosa.”
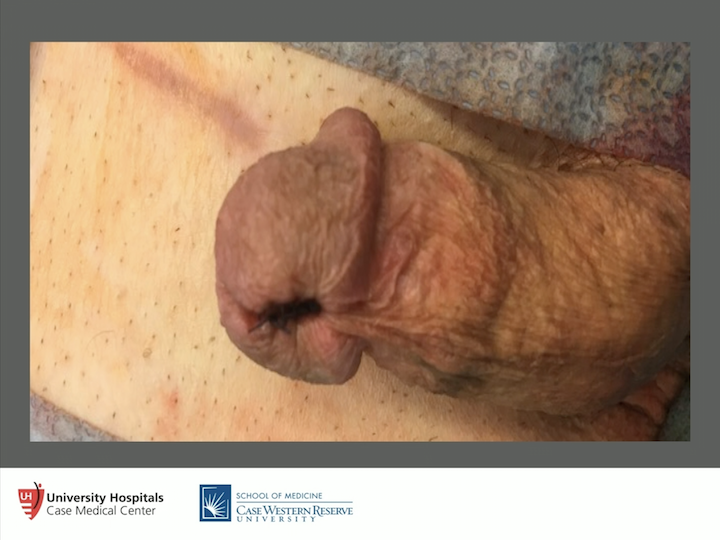
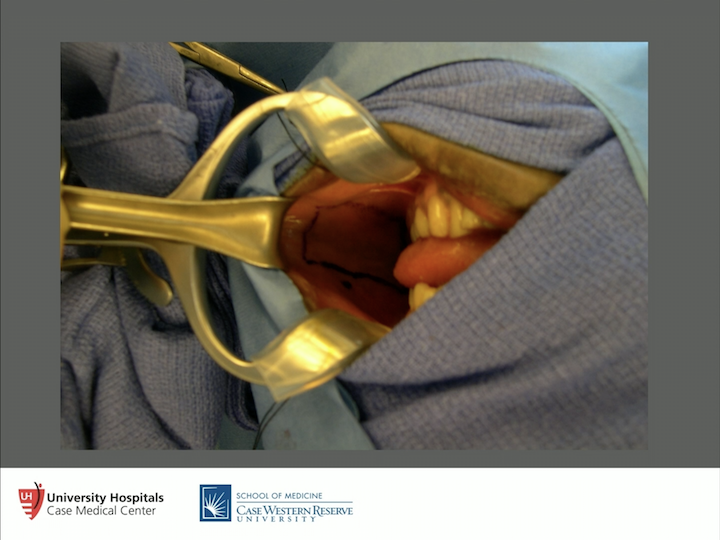
Meatotomy
We were able to get the meatotomy done, and you can tell from the appearance that, actually, people are happy with it, young and old. So the key is get rid of all of that scar tissue in the glans, but keep that meatus in the glans. If you drop it down here, you’re in a whole different world. So don’t do that. Keep the meatus in the glans. It’s just a simple meatotomy. Pull that mucosa, that healthy mucosa up to the skin, but get rid of all the bad stuff. If you find yourself having to dig deeper, then you probably need to do a fossa navicularis urethroplasty. So again this is very effective. It makes patients very happy. So extended meatoplasty.
Urethral Reconstruction
So for urethroplasty, the principles. You want to excise as much involved genital skin and urethral mucosa as possible. Sometimes, that gets hard, because everything is involved with it. So, give them steroids to make yourself feel better, but it’s probably going to wind up coming back. Frozen section analysis, only if you need to. You’ve usually made this diagnosis already at least once. We have some panurethral strictures that we have had. The tissue wasn’t looking right, wasn’t feeling right, so we did send frozen section analysis. It turned out to be squamous cell carcinoma deep in. So, this can happen very, very rarely, so it’s something to keep in mind. One operation or two operations? Nobody really has the right answer for this. My thoughts – Chris Gonzalez’s thoughts – for what that is worth. So, if it’s one stage, if it’s limited disease and the architecture is not distorted, if you’ve got an obliterated segment, if the architecture is distorted. If it’s all over the place and you’ve got to excise a lot of tissue, then go with multi-stage, and I hear some people talking about, “Hey, we don’t ever do multi-stage, or we only do –” that’s fine, but I think you’ve got to have – you have a little bit of some flexibility here, because not one size fits all.
Urethral Reconstruction #2
So, going back again to the guidelines. Evidence strength Grade B, this is probably some of the strongest evidence that we have in the stricture guidelines. So, surgeons should not use genital skin for reconstruction in proven LS. So, when we go back and look at early failures, late failures, Tony Mundy went back and looked at his results way back in the day as far as when he was doing urethroplasties with genital skin, and saw a lot of recurrences. We think it’s because we’re putting the lichen sclerosus from the genital skin right back into the urethra again, so we weren’t doing the patients a service at that point. So, again, stay away from if you’ve got lichen sclerosus, don’t use scrotal or don’t use penile skin at all. Recurrence rates even for short segment fossa navicularis strictures is anywhere from 50 to 100% so this is real. Oral mucosa is preferred, so that is what you want to use.
Cheek Oral Mucosa
There is lots of oral mucosa to get. So don’t ever take it from the lower lip. You get a lot of paresthesias, drooling, all of these types of things that can happen to patients. Take it from their cheeks. Know where Stensen’s duct is, which is outlined right there, and you can close it or leave it open. That’s always a little bit of controversy for us. If we’re taking about 4 cm or so, we’ll close it, and if we’re taking more, we’ll take the whole area out. You should get about up to 6 or 7 centimeters from each side or the cheek. You can get lingual tissue as well. We haven’t done that, but people talk about that. So, you can get quite a bit. So if you take 14, 15 cm, you are almost replacing the entire urethra, and at least 3 cm wide if you are going to do a staged approach. But many times, you only need about 1.75 or 2 cm in width if you’re going to do an onlay or an inlay.
Abdominal Skin
Something else that we had looked at was using skin right down here in the abdominal wall, the hairless skin just below the belt. Cosmetically, we thought that would be appealing. We reported on – these are the worst of the worst that we use this on, for both stage and single operations, but patting ourselves on the back on what great results we had after two years. And then, after about three or four years, we found that pretty much everybody failed. So then, we wrote another paper saying how bad, don’t do this. So anyways, it was a good idea when it lasted, but one big strip was something that we all thought was pretty good.
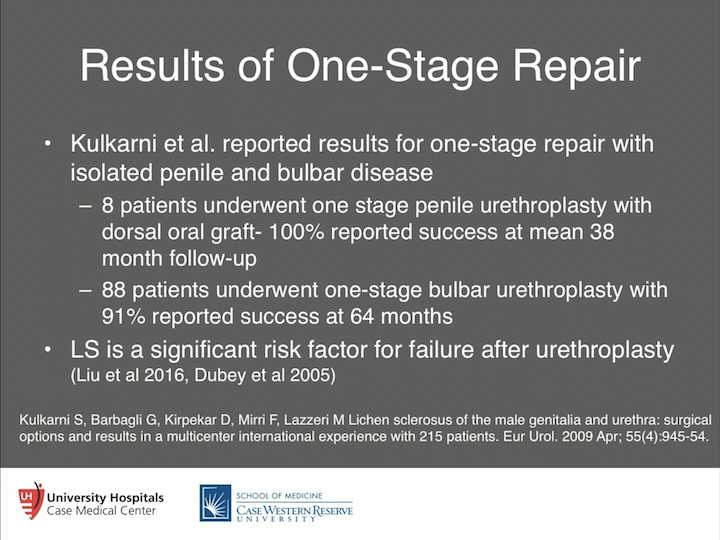
Results of One-Stage Repair
So results of one-stage repair, and these are the most expert hands, Sanjay Kulkarni, Guido Barbagli, fantastic surgeons. I’ve seen them both work. They’ve got excellent results. So, eight patients for one-stage penile urethroplasty. Dorsal oral graft 100% success at mean 38 month follow-up. I believe the results. 88% underwent a one-stage bulbar urethroplasty. Again, 91% reported success at 64 months. So, that’s very good patient selection. I’m sure they excised all of the excess disease, and they got a good operation done. But again we went back and looked at all of our failures for urethroplasty, and other groups have done the same thing. LS is a significant risk factor for failure, so you have to prep the patient up that this is one of the things that may get you. We have to keep a close eye on you. Most of the time, we’ll endoscopically cut them with a cold knife. If they do come back, they will come back at one side or the other of the anastomosis. So again, it’s a significant risk factor for failure, but patient selection is very important.
Multi-stage repair
What about a multi-stage repair? This is more involved. So, this is when you’ve got the obliterated urethral segment. The architecture is distorted. So, what we will do is we will put a sound in that urethra, and we’ll take the knife, and we’ll open them all the way up as far as they need to go. Some go all the way back to the bulbar urethra. Some go to the penile urethra.
Process of Lichen Sclerosus Surgery
Excise all of the penile skin that is involved, and that’s a big piece of urethral mucosa that’s involved. That comes out. We get everything cleared out of there, because if we don’t, it’s going to come right back and it’s going to burn us.
Process of Lichen Sclerosus Surgery #2
And then, we plate that with buccal mucosa, and that’s actually – we get as much out as we can, put the buccal mucosa in. We pie-crust it to make sure there is no seromal formation, put some quilting sutures in there, we’ll let a dressing stay on there for about five days, take the dressing and the catheter out. These patients are exceedingly happy because they can pee for the first time, they can have sex. Some say, “Hey, doc, nice work, I don’t think I need the second stage, I don’t want to risk it,” and they don’t come back. I think that’s fine. Most do say they want to get it rolled up and taken care of, and the other thing with this, with lichen sclerosus, you keep an eye on it for four to six months and make sure it doesn’t come back. And treat it if it does, and I wouldn’t treat it with steroids. I would excise it and would do more grafting on it, but that’s pretty rare if you do a good job the first time around.
Architecture Distortion Example
Different patient, but that’s what you’re looking at at around six months. So there you’ve got the buccal mucosa, you’ve got a little bit of architecture distortion there, more on the right than the left due to all the disease this person had. So what we will do then is we will close them up.
Wound Closure
So how do you close them up? You make an incision between the penile skin and buccal mucosa, and you free this whole area up so it’s very, very loose, and you take a 4-0 or a 5-0 Vicryl and you put a couple of rows of sutures in that to close them up.
Wound Closure #2
Get them closed up, get the glans closed, close the penile skin. I was using tunica vaginalis around the testicle to wrap that as an insurance layer, but I’ve stopped actually, because if you get a good closure, you don’t necessarily even need that. Plus they don’t have to have the testicle issues that they’ll complain of. “My testicle rides high now, thanks a lot, doc.” So, I try and stay away from those things if need be.
Results of Two-Stage Repair
So again, Kulkarni reports the results of two-stage penile urethroplasty, and those are very difficult cases, and again 15 patients with 73% success. That makes sense. It’s harder to fix a stricture in the penile urethra than it is in the bulbar urethra. Maybe it’s blood supply. Hard to say, but it’s just tougher to fix. And Drew Peterson also reported the same thing, about 82% success in 11 patients who underwent a two-stage procedure. So, it works when done right, but a lot of counseling needs to be done with the patient. So, it’s extremely important that that gets done.
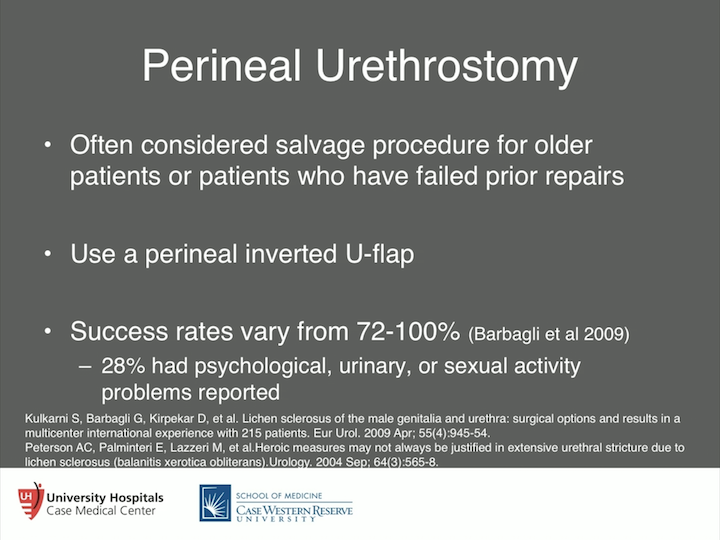
Perineal Urethrostomy
So what about perineal urethrostomy? We talk about this as a bail-out maneuver. I think it’s an under utilized operation. I think it’s something that definitely works, but you have to consider if there is lichen sclerosus in the penile urethra or in the bulbar urethra. It’s going to be involved when you do the perineal urethrostomy. Okay? So, consider it a salvage procedure for older patients or patients with failed prior repairs, but you’ve got to counsel the patient up. But, I will tell you these folks are very, very happy. We use the inverted U-flap. So we’ll make an inverted U-flap in the perineum. We’ll leave the urethra almost inside too, open up longitudinally, and bring that U-flap right down to the inferior aspect of my urethrotomy. Bring the scrotum down to the superior aspect of the urethrotomy and close the skin around it. I think it’s very effective. It’s a very well-defined approach. What is interesting is Guido was very honest about his data. Good functional results with these folks, but he reported that about a third had problems with psychological issues, urinary and sexual activity issues with their partner. So, it’s something to keep in mind, especially if you are going to operate on somebody who is still sexually active. That’s very, very important is you’ve got to explain these things to them. So, a third is a lot. So they may be able to pee well, and they may be happy with you from that perspective, but you may be altering some other things. So, it’s something to keep in mind.
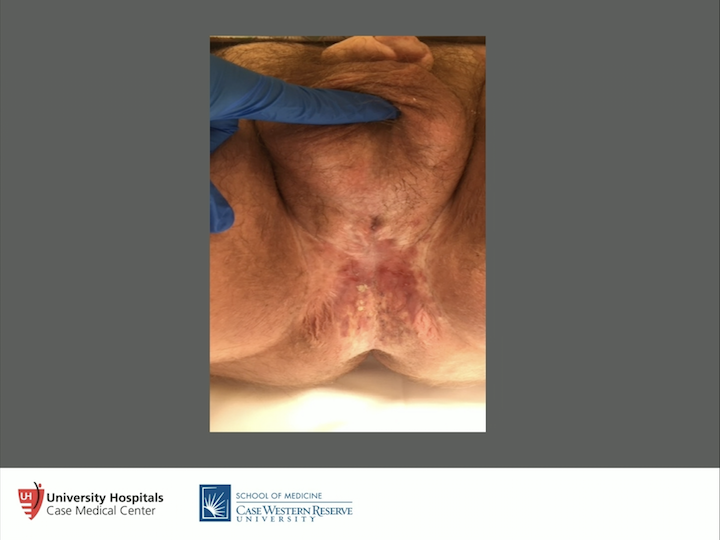
Individual Case
And just kind of this last slide is just to show just how aggressive this lichen sclerosus is. This is a gentleman that we had done probably three or four operations in a multi-staged approach. He had recurred. He kept recurring. Why he kept coming back to me, I’m not sure, but he did. So basically, what we did was we did a perineal urethrostomy on him. We were all happy with that. Peeing well, and the lichen sclerosus recurred right in the perineal urethrostomy in the perineum. I’ve never seen that before. So, we treated this individual with steroids. I don’t know what else to do, right? You know, made it look good, probably for us, and then we did another inverted U-flap on him. And he’s actually been doing well about two years out, but this is the kind of aggressive disease you have to deal with. We biopsied him up and down to make sure this is not cancer, but again, there are treatment algorithms for these patients. But don’t be afraid to refer them. And I think that the biggest thing is steroids, probably most likely a temporary effect. I don’t think there’s any long-term effects with patients and steroids.
ABOUT THE AUTHOR
Chris M. Gonzalez, MD, MBA, FACS, is the Albert J. Speh, Jr., and Claire R. Speh Professor and Chair of the Department of Urology at Loyola Medicine and Loyola University Chicago Stritch School of Medicine.
Dr. Gonzalez earned a medical degree from the University of Iowa College of Medicine and completed a urologic residency at McGaw Medical Center of Northwestern University. He earned an MBA from the Kellogg School of Management at Northwestern in 2006. He served as Chief of Urology for VA Lakeside from 2003 to 2006 and was Director of Surgery for the Northwestern Medicine Surgical Services Department from 2014 to 2015. He then moved to the University Hospitals Cleveland Medical Center in Ohio, where he served as the Lester Persky Professor and Chair of the Department of Urology and Director of the Urologic Institute from 2015 to 2018.
Dr. Gonzalez is Associate Editor for the Genitourinary Reconstruction Section of Urology and a Section Editor for Urology Times. He has published numerous peer-reviewed manuscripts, articles, editorials, and book chapters. Dr. Gonzalez is also an expert clinician who specializes in urethral stricture disease, salvage of failed hypospadias surgery, genitourinary fistula disease, erectile dysfunction, penile prosthesis placement, Peyronie’s disease, penile curvature correction, and treatment of male urinary incontinence.