How to cite: Nickel, J. Curtis. “Prostate Inflammation and Prostate Cancer: What do I need to know?” January 27, 2018. Accessed Nov 2025. https://grandroundsinurology.com/Prostate-Inflammation-and-Prostate-Cancer/
Reveal the Answer to Audience Response Question #1
- A. Greater BPH and Clinical Prostatitis symptom severity
- B. BPH and Clinical Prostatitis symptom progression
- C. Increased risk of developing BPH and Prostatitis Symptoms
- D. Increased risk of developing Prostatitis Symptoms
Reveal the Answer to Audience Response Question #2
- A. Higher incident risk and increased severity of PCa
- B. Lower incident risk but increased severity of PCa
- C. Higher incident risk but decreased severity of PCa
- D. Lower incident risk and decreased severity of PCa
Summary:
Dr. J. Curtis Nickel, MD, FRCSC, explains the relationship between acute and chronic inflammation of the prostate and prostate cancer risk, citing data from the REDUCE trial. He also discusses prostate cancer risk factors, including tumor volume, number of positive cores, and prostate atrophy.
Prostate Inflammation and Prostate Cancer: What do I need to know? – Transcript
Click on slide to expand
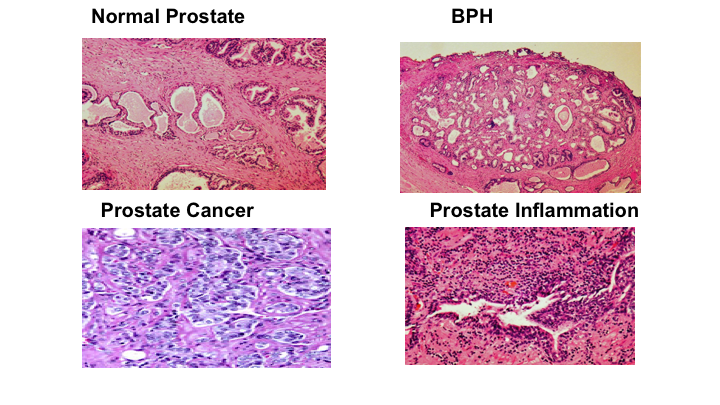
Normal Prostate – BPH
So like I said, the prostate cancer at the bottom left there is not really my area of expertise, but I do know what a normal prostate looks like. I’ve worked in BPH for over 25, 30 years, and prostate inflammation is what I’m very interested in, its relationship to prostatitis and other diseases of the prostate. That disease of the prostate, of course, is prostate cancer. Next slide please. Oh, I’ve got it here.
REDUCE Study
So I’m going to jump right in and not talk about prostatitis because I only have a small amount of time, but some year I’ll come and talk about clinical prostatitis, prostate cancer, and what not, but what I want to talk about is a study that you’re all aware of, certainly oncologists are, the REDUCE study. It really didn’t do that—make that much of a big bang in prostate cancer prevention. It did not get the FDA indication. so what use is it? Well, it turns out to be a fantastic study to predict who is going to get prostate cancer, and if they get it how severe it is.
It is actually the best longitudinal study we will ever have to evaluate prostate inflammation and implications for BPH because we collected IPSS symptom score. Chronic prostatitis because we collected information, the chronic prostatitis symptom index, and prostate cancer because everybody in this study had a mandated biopsy, one for either for cause or a mandated biopsy at two years and four years. They all had a biopsy to start with.
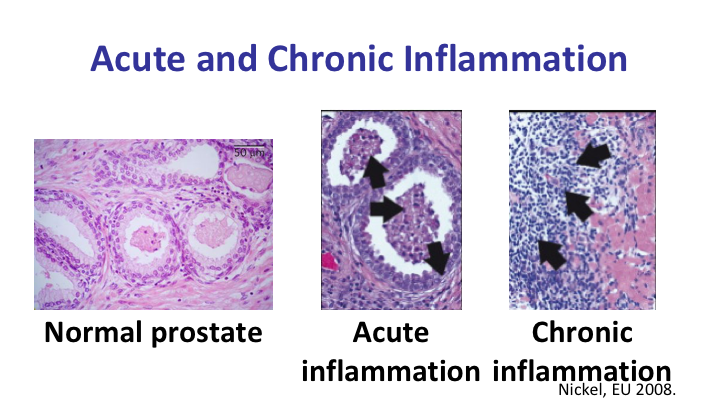
Acute and Chronic Inflammation
And we were able to induce, twist GSK’s arm to say that it is important to figure out this story of inflammation and prostate cancer. So we were able to determine whether the patients had a normal prostate, whether they had acute inflammation or chronic inflammation.
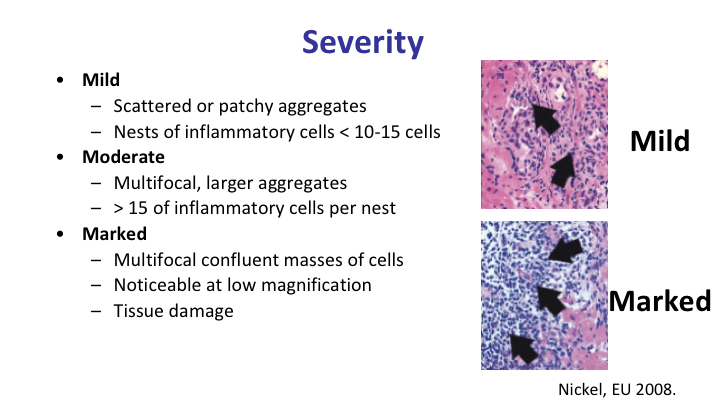
Severity
And we also determined whether they had mild, moderate or marked inflammation, and we also determined the extent of prostate inflammation across all the six to ten cores that they had during the initial biopsy. And if you remember, the patients had biopsy for cause likely PSA, but the biopsy was negative for prostate cancer.
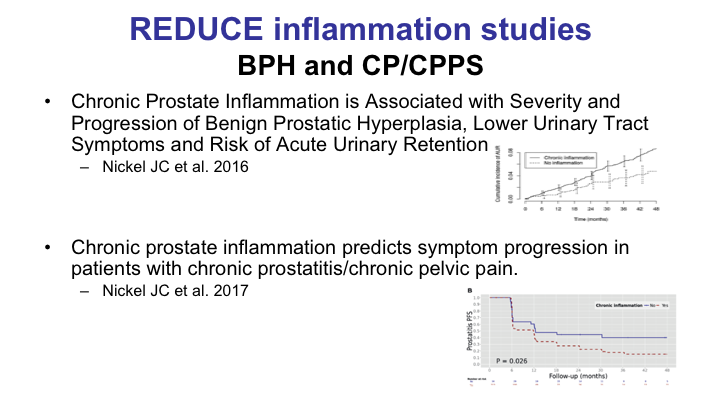
REDUCE Inflammation Studies
I’m going to jump into two conclusions that we reached in terms of the benign study without going into the details, but if you had inflammation at a first biopsy, it did not predict whether or not you had clinical prostatitis, but it did predict if you had chronic prostatitis symptoms that you would have progression of those symptoms. Similarly, with BPH it did the same thing. If you had BPH in terms of an enlarged prostate, an IPSS symptom score in the BPH range, and you had inflammation, it predicted progression of BPH.
Bottom Line
So the bottom line is inflammation of prostate is predictive of progression in patients suffering from both BPH and prostatitis.
Prostatitis, Prostate Inflammation, and Prostate Cancer
Now, clinical prostatitis, I don’t want to get into that, but patients with clinical prostatitis seeing urologists have a higher risk of being diagnosed with prostate cancer, and all of the studies suffer from the bias of over urology utilization. Once the prostatitis patient gets into the urologist’s hands, not only is he concerned that he has prostate cancer, he’s going to get PSA testing, and he’s more apt to get a biopsy. So it is unlikely a real thing.
Histological prostate cancer we know from other cancers such as cervical, esophageal, gastric, that inflammation is involved in the pathogenesis and etiology of those particular cancers. What about prostate? Well, certainly there is a lot of evidence, particularly the association in histological sections, and autopsy series, of a close association between inflammation of prostate cancer that this could be the case.
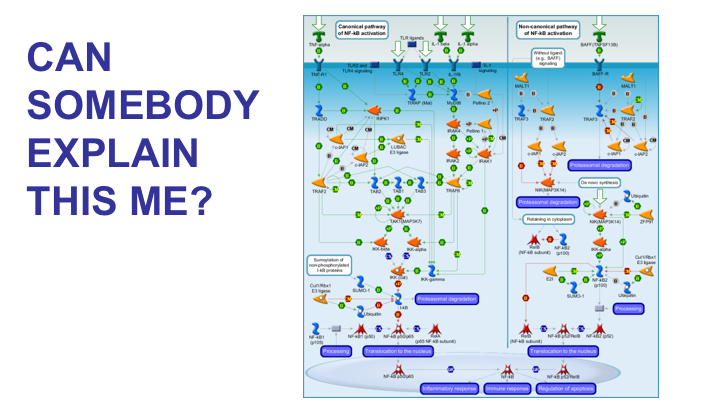
Can Somebody Explain This to Me?
I’ve been at a lot of prostate cancer meetings, and invariably somebody throws up a slide like this. I’ve always wanted to do that because I’m going to serve a simple field. So finally I’m in a prostate cancer meeting, and I explain the theory of why inflammation can cause prostate cancer. And this is great. Now, it’s kind of interesting because in reality it looks to me like this is evolution from the bottom of the ocean up to the air, but all of these things are very important and they make absolutely no sense to me. But this is the explanation of why inflammation causes prostate cancer.
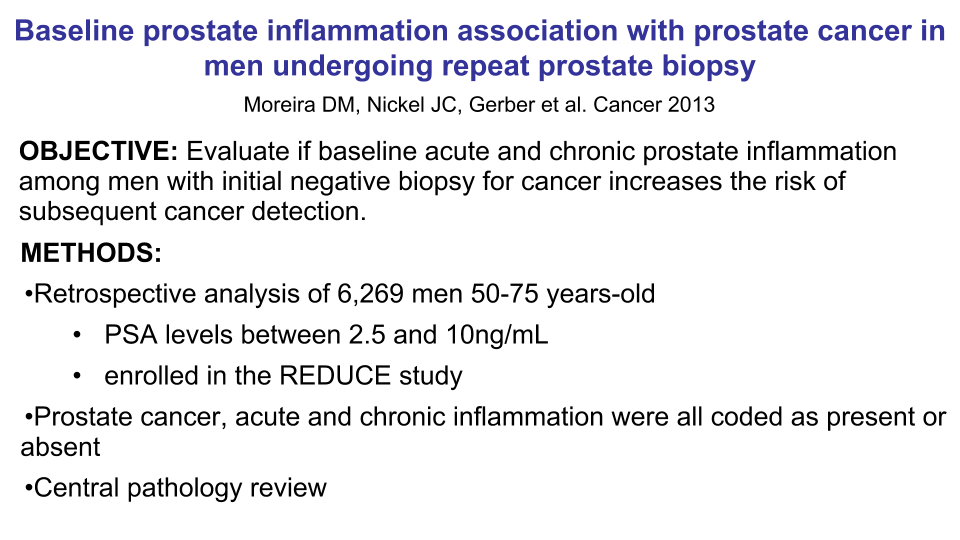
Prostate Inflammation Association with Prostate Cancer in Men Undergoing Repeat Prostate Biopsy
What we wanted to do is take the reduced biopsies and see whether or not inflammation in the initial biopsy and the extent and the severity of the inflammation plays a role of whether or not they develop prostate cancer over the four years of the study.
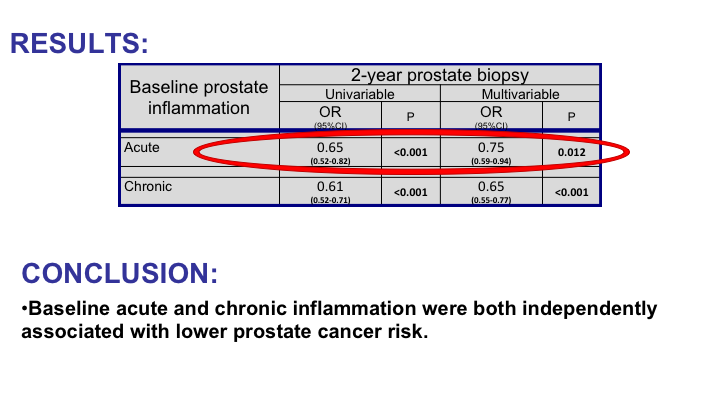
Results
So the results I’m just going to throw them right out here. For acute inflammation and this is yes/no, they had acute inflammation or no inflammation. There was a decreased risk of having prostate cancer in subsequent biopsies. With chronic inflammation it was even more significant. Conclusion of this first analysis we did is baseline acute and chronic inflammation were both independently associated with a lower prostate cancer risk.
Well, we need more information of that because we have to have concordance all the way around.
Extension of Baseline Prostate Acute and Chronic Inflammation Association with Incidence of Prostate Cancer on Repeat Biopsy
What we did is we looked at the extent of baseline acute and chronic prostate inflammation, and we tried to associate that with the incidence of prostate cancer on repeat biopsy. Now, this is a little bit complicated, but as you can see, we can see the number, the percentage of the cores with acute inflammation, chronic inflammation, and these are the PSA prostate volumes and everything.
Cores with Prostate Inflammation
But when we actually look at the actual study, what we see is there is a very significant—a significant association between the extent of inflammation and a lower risk of prostate cancer.
If we look at the chronic inflammation, I have two buttons here, we also see a significant association between the extent of chronic inflammation seen on the biopsies and whether or not the patient has prostate at 2 and 4 years. So the extent of baseline acute and chronic prostate inflammation was again independently associated with a lower prostate cancer risk. And in all of these studies we did account for prostate volume. We did account for PSA. We did account for age.
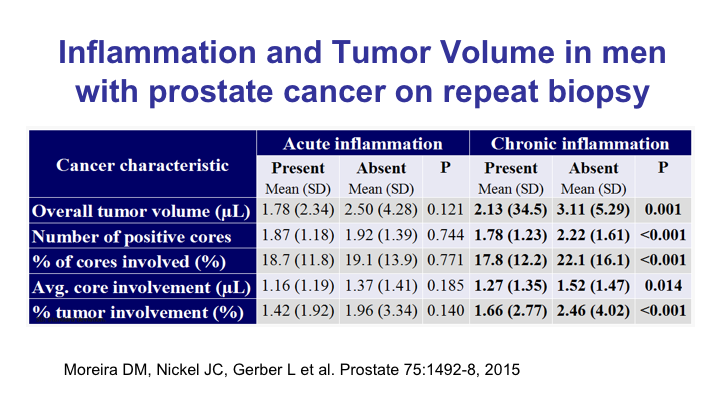
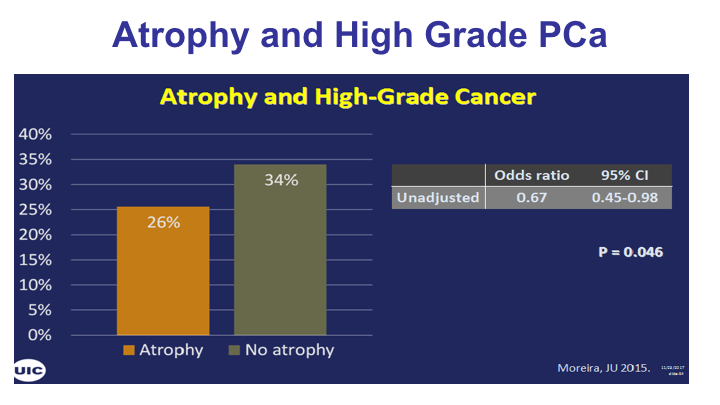
Inflammation and Tumor Volume in Men with Prostate Cancer on Repeat Biopsy
Now, what about inflammation and tumor volume? That’s something else we’re interested in, and again this is the data, but basically the overall tumor volume, the number of positive cores, the percentage of cores involved and the percentage of tumor involvement were all independently related to chronic inflammation, not acute inflammation. In other words, if you had chronic inflammation, you had less volume if you actually were diagnosed with cancer. Okay. So the ones that were diagnosed with cancer and had inflammation had a reduced volume than those that had no inflammation.
Inflammation and Prostate Volume
So those that had inflammation had a reduced volume than those that had no inflammation. So baseline chronic inflammation was associated with lower prostate cancer volume. These are the patients that actually got the prostate cancer.
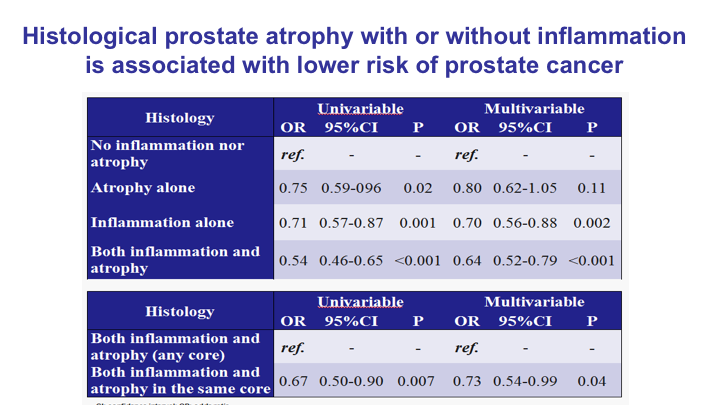
Histological Prostate Atrophy with or without Inflammation Is Associated with Lower Risk of Prostate Cancer
What about prostate atrophy? We looked at that as well with or without inflammation is again associated with a lower risk of prostate cancer. Atrophy alone, inflammation alone, both together, and we see a significant, both a univariate and multivariate analysis, decreased risk of prostate cancer.
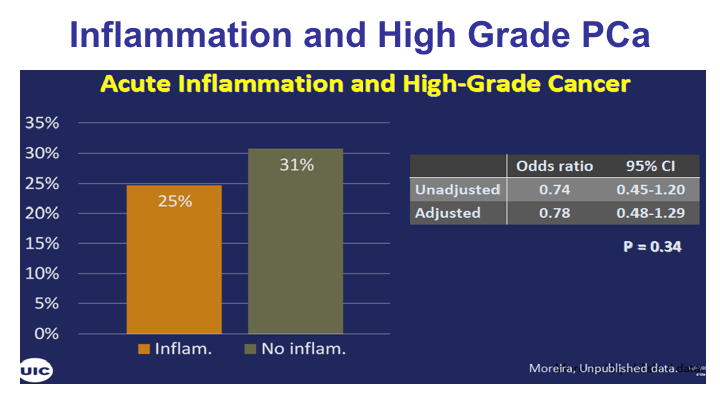
Inflammation and High Grade Prostate Cancer – Acute
What about grade? If you have acute inflammation you have a decreased chance of having high-grade 8, 9, 10 prostate cancer compared to those with no inflammation, but it wasn’t statistically significant.
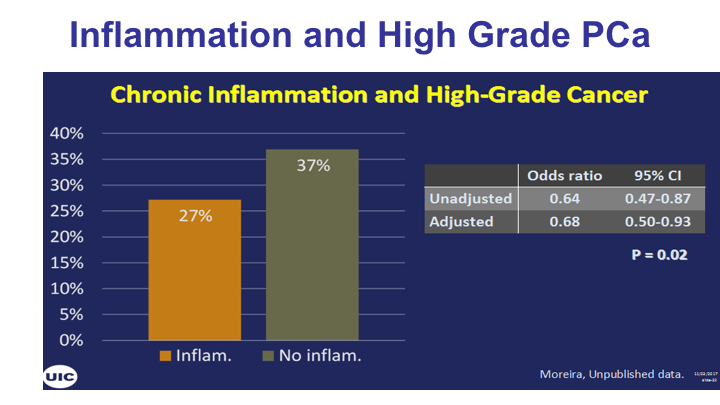
Inflammation and High Grade Prostate Cancer – Chronic
For chronic inflammation it was statistically and perhaps even clinically significant difference. Certainly, the odds ratio appear to show a significant benefit of having inflammation on a first biopsy subsequently getting cancer, and don’t forget you have a lower risk to develop cancer, and when you get cancer you have a lower volume and you have a predicted lower grade.
Bottom Line
So the bottom line of this whole analyses that I get a chance to present today on inflammation in the REDUCE study is that this is going to be the largest and longest database to look at inflammation and BPH, prostatitis, and prostate cancer outcomes ever in my lifetime. We will never get thousands of patients with biopsies, with no cancer, and then find out who gets cancer subsequently along the four-year time zone, and in this we were not able to show our hypothesis. Our hypothesis was that inflammation would predict number one, increased risk of prostate cancer, and, two, increased severity of prostate cancer. We were not able to show that in this particular study, and in fact we only showed that existing prostate inflammation predicted a lower risk in severity of prostate cancer.
Does the Literature Really Support This?
Does the literature really support this? Well, the literature is terrible. The actual studies that were done, a lot of them were associated studies. They were studies of 30 patients, the largest being a little over 150 patients. They were short-term studies, they were all uncontrolled. They weren’t controlled like the REDUCE study.
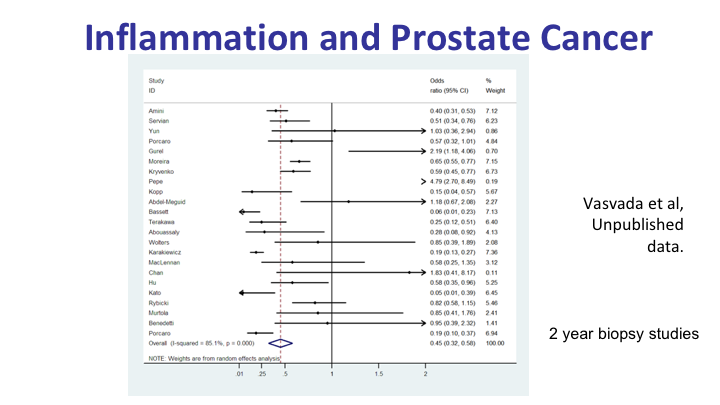
Inflammation and Prostate Cancer
But when you do a meta analysis of a two-year biopsy study, that’s the only—they had to have at least two years’ data to fit into this meta analysis what we found is that inflammation on prostate needle biopsy on the first biopsy was associated with a lower prostate cancer risk over a two-year period in this meta analysis.
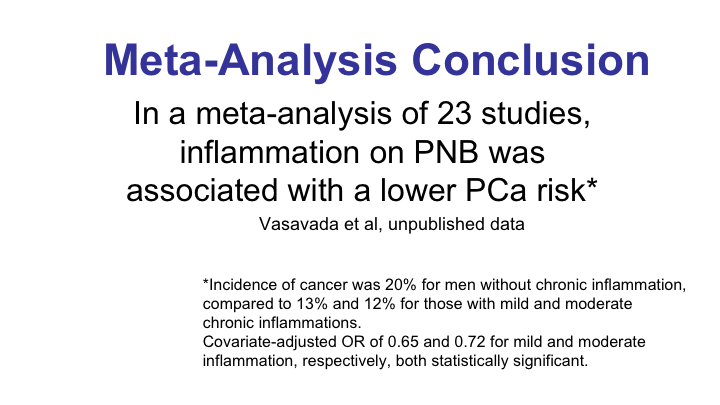
Meta-Analysis Conclusion
So without chronic inflammation the incidence of prostate cancer was 20% in the meta analysis. If there was inflammation, chronic inflammation on the initial biopsy it was 13, and 12% for those with mild and moderate inflammation. So the odds ratio was very clinically significant for this.
Clinical Implications for the Urologist
So what are the clinical implications of our analyses of inflammation in the REDUCE study? Well, for the benign conditions of which I was initially interested in, the presence of inflammation on prostate biopsy predicts BPH and prostatitis progression if they had those at the time of biopsy. If one of your patients on biopsy has inflammation on prostate biopsy, it predicts a lower prostate cancer risk, and that’s a lower incident risk, and if they develop—if they do have prostate cancer, it predicts a decreased or lesser severity. Thank you very much.
ABOUT THE AUTHOR
Dr. Nickel is the Canada Research Chair in Urologic Pain and Inflammation and a Professor of Urology at Queen’s University in Kingston, Ontario. He is also a staff urologist at Kingston General Hospital. Dr. Nickel’s research covers inflammatory, benign prostate, and pain diseases of the urinary tract. He has over 550 publications, is on the editorial board of eight urology journals, serves as editor of the AUA Update Series, has presented in 45 countries, and is funded by the US NIH and Canadian CIHR. He has been awarded a CIHR Tier I Canada Research Chair (until 2021), as well as an AUA Distinguished Contribution Award and SIU Academy Award. He is currently Immediate Past-President of the Canadian Urological Association.