M. Scott Lucia, MD, presented “Temporal Shifts in Grade and Stage of Prostate Cancer: A Whole Mount Analysis” during the 24th Annual Southwest Prostate Cancer Symposium on April 11, 2019 in Scottsdale, Arizona.
How to cite: Lucia, M. Scott “Temporal Shifts in Grade and Stage of Prostate Cancer: A Whole Mount Analysis” April 11, 2019. Accessed Jun 2025. https://grandroundsinurology.com/temporal-shifts-in-grade-and-stage-of-prostate-cancer-a-whole-mount-analysis/
Temporal Shifts in Grade and Stage of Prostate Cancer: A Whole Mount Analysis – Summary:
M. Scott Lucia, MD, discusses the impact of changes in the clinical management of prostate cancer on pathological features of tumors in prostatectomy specimens processed over the last 16 years at his institution. He discusses the role of shifting screening and active surveillance practices in these observed changes in tumor features.
Abstract:
The clinical presentation and management of prostate cancer (PCa) has shifted dramatically over the last two decades. Changing attitudes towards PCa screening and the use of active surveillance for patients with low volume, low-grade PCa, as well as the choice of surgery for more advanced PCa, may have affected grade and stage migration. Changes in pathological grading of tumors have also led to higher tumor grades on biopsy and radical prostatectomy (RP).
These changes have resulted in marked shifts in the pathological features of the tumors in prostatectomy specimens collected in a database at the University of Colorado Anschutz Medical Campus.
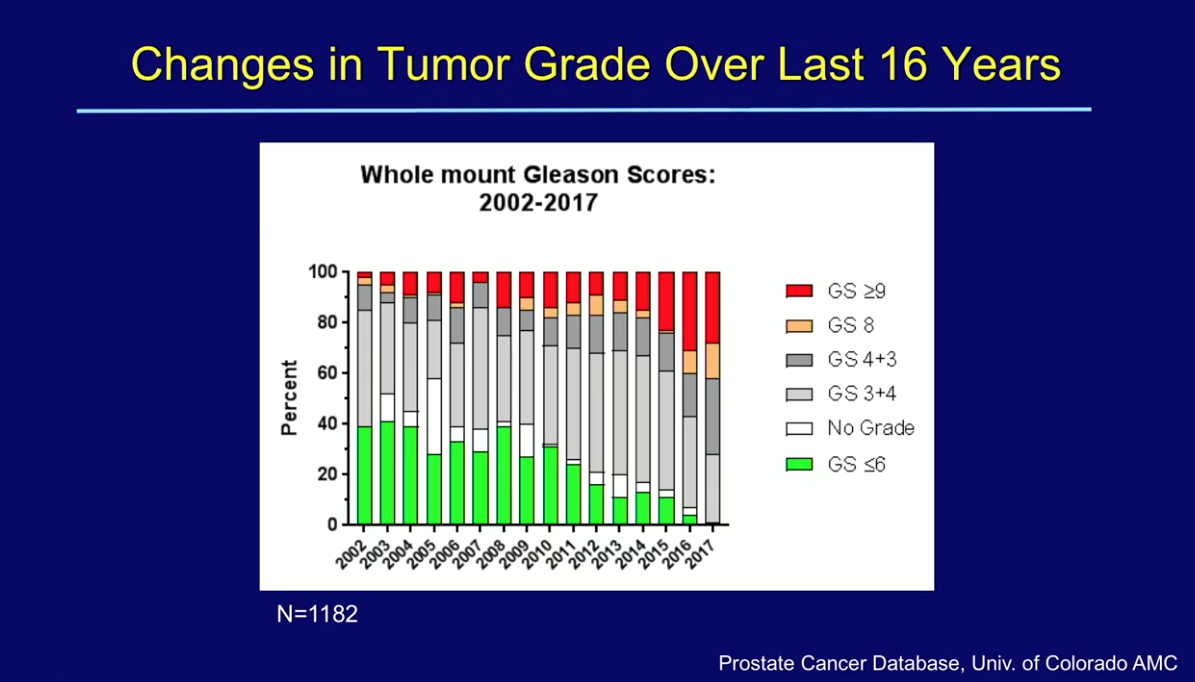
Upon assessing prostatectomy specimens, which the institution has been processing as whole-mounts with 3D-reconstruction over the last 16 years, there was an observed shift toward higher tumor grades, volumes, and more advanced stage. Gleason grade ≤3+3 tumors previously represented almost 40% of cases.
These tumors now represent only a small percentage of surgical tumors, while high-grade disease, Gleason grades ≥4+3, represent the majority of cases. Non-organ-confined disease has risen from under 30% in the years prior to 2013 to almost half of all prostatectomies in 2017. Node-positive disease has risen almost two-and-a-half fold in that time. Yearly mean tumor volumes that remained at approximately 2 cc prior to 2012 now average between 3-4 cc.
While changes in pathological grading can certainly impact Gleason score at RP, the more recent findings of increased stage and tumor volume implicate current clinical practices in contributing to patients with more aggressive and advanced tumors at the time of surgery. Further investigation is necessary to determine if these shifts could possibly impact long-term outcomes.
About the Southwest Prostate Cancer Symposium
The Southwest Prostate Cancer Symposium (SPCS) is a multi-day conference that seeks to educate urologists, radiation oncologists, medical oncologists, and other healthcare professionals involved in the treatment of prostate cancer. The topics focus on current technical aspects of diagnosis and treatment of localized and advanced disease, particularly regarding imaging, technology, and training in the related devices. Dr. Lucia presented this lecture during the 24th SPCS in 2019. In 2020, the 25th SPCS will also offer training sessions involving imaging, scanning, and prostate cancer treatment related devices on site. Please visit this page in order to register for future SPCS meetings.
ABOUT THE AUTHOR
M. Scott Lucia, MD, is Professor and Vice Chair of the Department of Pathology and Director of Anatomic Pathology and of the Prostate Diagnostic Laboratory at the University of Colorado Anschutz Medical Campus (UCAMC) School of Medicine. He also serves as the Director of the Prostate Cancer Research Laboratories at UCAMC and of the UCAMC Biorepository Core Facility. Dr. Lucia received his MD from the University of Colorado School of Medicine in 1988. He completed his internship and residency in pathology at the University of Colorado in 1993. He was a research fellow in the Laboratory of Chemoprevention at the National Institutes of Health from 1993 to 1995, before returning to the University of Colorado in 1995.
Dr. Lucia served as the primary pathologist for the Prostate Cancer Prevention Trial (PCPT) and Vitamin E and Selenium Chemoprevention Trial (SELECT), sponsored by the Southwest Oncology Group; the Medical Therapy of Prostate Symptoms (MTOPS) trial, sponsored by the NIDDK; and the Reduction with Dutasteride of Clinical Progression Events in Expectant Management of Prostate Cancer (REDEEM), sponsored by GlaxoSmithKline. He directs the operation of several tissue and serum biorepositories for prostate and prostatic diseases, including those for the PCPT, MTOPS, SELECT, and the University of Colorado Cancer Center Prostate Biorepository. He has authored or co-authored over 180 peer-reviewed articles, reviews, editorials, and book chapters. His primary areas of interest include pathology of prostate cancer and hyperplasia, early detection and prevention of prostate cancer, prostate cancer biomarkers, and mechanisms of carcinogenesis.