Leonard G. Gomella, MD, presented “Thromboembolic Complications in Bladder Cancer” during the 3rd Annual International Bladder Cancer Update on January 23, 2019 in Beaver Creek, Colorado.
How to cite: Gomella, Leonard G. “Thromboembolic Complications in Bladder Cancer” January 23, 2019. Accessed Jun 2025. https://grandroundsinurology.com/thromboembolic-complications-in-bladder-cancer-2/
Thromboembolic Complications in Bladder Cancer – Summary:
Leonard G. Gomella, MD, FACS, discusses the highly thrombogenic nature of bladder cancer and the burden of thromboembolic complications in patients undergoing radical cystectomy. He then reviews optimal methods and duration of prophylaxis to reduce the risk of these complications.
Abstract:
Radical cystectomy is a complex, extirpated operation that violates two organ systems. The procedure has alarming rates of complications and 90-day mortality, readmissions, and costs. Furthermore, there have been no significant changes in rate, type of, or severity of 30-day radical cystectomy-related since 2010.
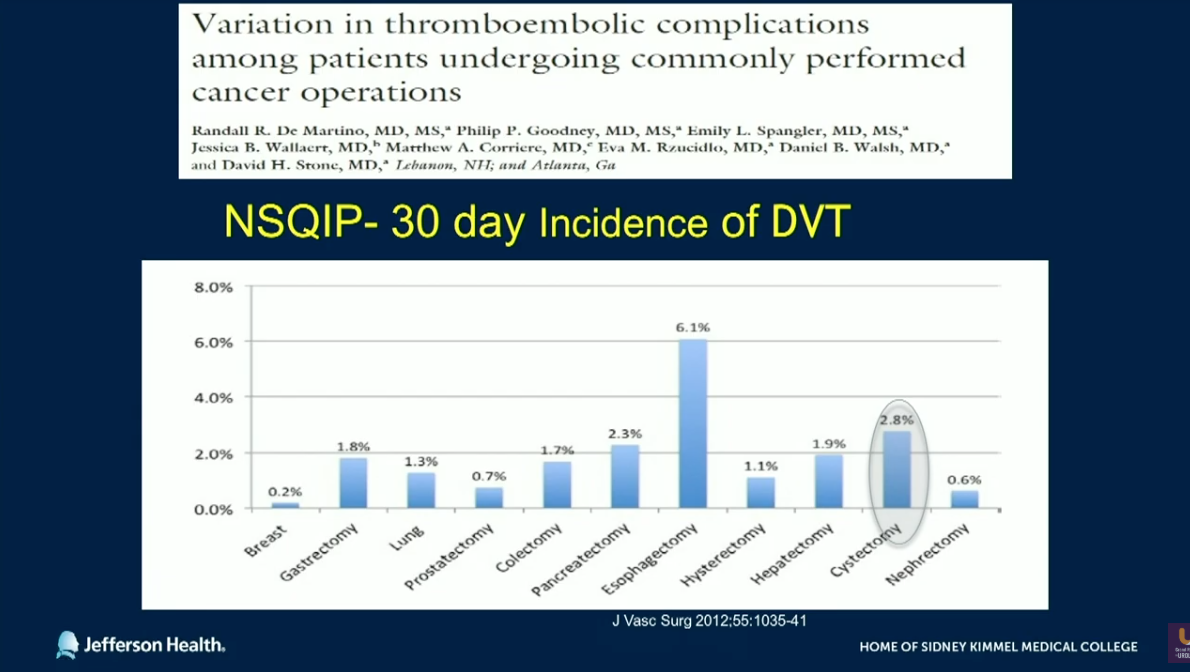
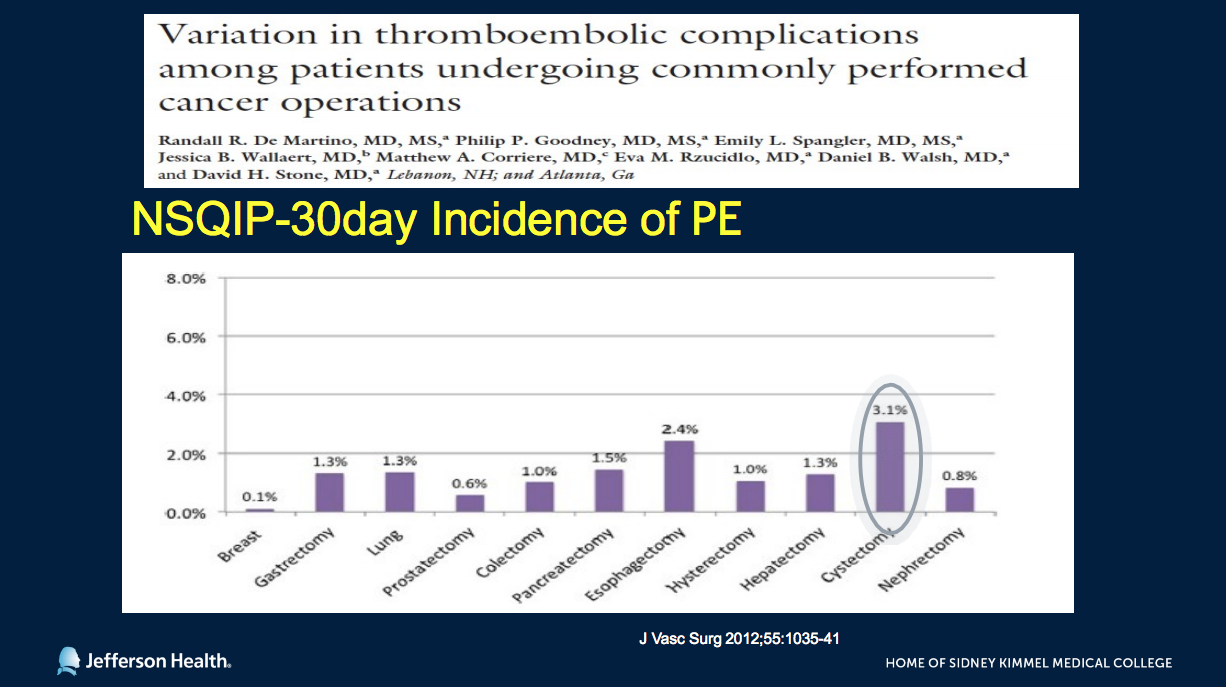
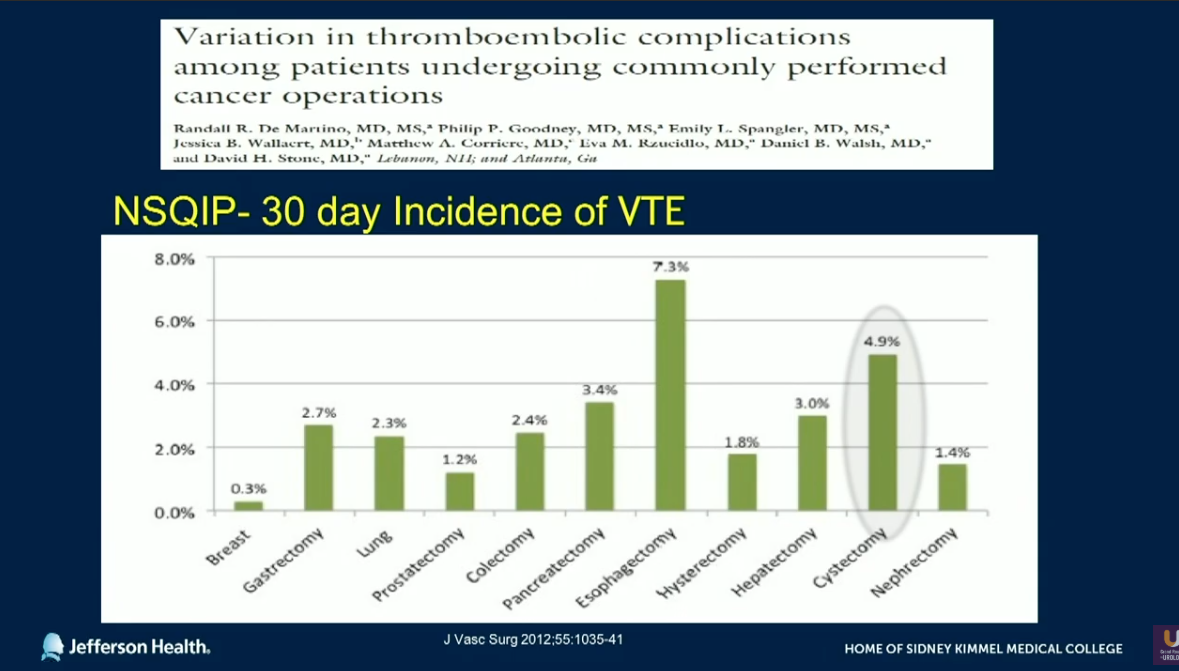
Of these complications, bladder cancer patients are particularly susceptible to thrombogenic events due to disease-related factors that induce hypercoagulability, common bladder cancer patient characteristics, and consequences of treatments. Because of these factors, cystectomy ranks second in the incidence of deep venous thrombosis (DVT) and venous thromboembolism (VTE) among commonly performed cancer operations. It also ranks first in pulmonary embolism (PE).
Evidence shows that the use of robotic robot-assisted radical cystectomy rather than open radical cystectomy leads to little improvement rates of PE and VTE complications. Similarly, studies have shown little benefit to using Enhanced Recovery After Surgery (ERAS) protocols in radical cystectomy complications. However, methods that could decrease the risk of these complications include perioperative chemoprophylaxis and compression boots, early ambulation, and extending DVT prophylaxis beyond patient discharge. Options for perioperative parenteral anticoagulation include unfractionated heparin and low molecular weight heparins.
This presentation discusses safety, efficacy, and cost of extended prophylaxis, as well as optimal duration of VTE prophylaxis, specifically if it should extend longer than 4 weeks post-cystectomy. The conversation also covers the risk of arterial thromboembolism (ATE) in patients undergoing cystectomy, and the impact of neoadjuvant chemotherapy on thromboembolic events.
About the International Bladder Cancer Update
The International Bladder Cancer Update (IBCU) is an annual one-day CME conference focused on bladder cancer treatment updates. IBCU takes place during its sister conference, the International Prostate Cancer Update (IPCU). The conference’s faculty consists of international experts, and the event caters to urologists, urologic oncologists, and other healthcare professionals. In addition to didactic lectures, IBCU features interactive discussions, a panel roundtable, debates, and case presentations. Dr. Gomella presented this lecture during the 3rd IBCU in 2019. Please visit this page in order to learn more about future IBCU meetings.
ABOUT THE AUTHOR
Leonard G. Gomella, MD, FACS, is the Bernard W. Godwin, Jr. Professor of Prostate Cancer and chair of the department of urology at Sidney Kimmel Medical College of Thomas Jefferson University in Philadelphia, Pennsylvania, where he also serves as senior director for clinical affairs. Originally from New York, Dr. Gomella completed medical school and general surgery and urology training at the University of Kentucky in Lexington. After a urologic oncology fellowship in the surgery branch of the National Cancer Institute, National Institutes of Health in Bethesda, Maryland, he joined Thomas Jefferson University in 1988 and was appointed chair of the urology department in 2002. From 1998 until 2020 he was urology chair for the Radiation Therapy Oncology Group (RTOG) (now NRG Oncology) and from 2008 until 2019 he was clinical director of the Sidney Kimmel Cancer Center Network.
Dr. Gomella is involved in translational basic science and clinical research developing new diagnostic tests and treatments for prostate, bladder, and kidney cancer through the Sidney Kimmel Cancer Center where he has co-led the Biology of Prostate Cancer Program. Dr. Gomella's team was first to use molecular techniques (RT-PCR) in 1992 to detect circulating prostate cancer micrometastases, the first report of “liquid biopsy,” a discovery that led to a new field of investigation in this disease. Dr. Gomella is also recognized for developing the multidisciplinary clinic approach to prostate cancer and was an early contributor to urologic laparoscopy. He led the urology effort in the 2017 and 2019 Philadelphia Prostate Cancer International Consensus that provided the first multidisciplinary guidance on genetic testing for prostate cancer.
Dr. Gomella has given over 600 presentations nationally and internationally and written over 600 papers, chapters and monographs in urology. He has authored and edited 63 editions of 17 different books for medical students, residents, and practicing physicians, many of which have been translated into foreign languages. Dr. Gomella has consistently earned recognition for urologic oncology and prostate cancer, including a 2015 national recognition in Newsweek. In 2007, Men’s Health Magazine listed Dr. Gomella as one of the 20 top urologists in the US. Among other awards, in 2018 the Society of Urologic Oncology presented him with a “Distinguished Service Award.” In 2019, Dr. Gomella was named Enterprise Urology Vice President for Jefferson Health. Additionally, the American Urological Association (AUA) awarded him “Honorary Membership” status in 2023 in recognition for his contributions and leadership in urologic oncology. Dr. Gomella has been president of the Mid-Atlantic section of the AUA and elected to the American Association of Genitourinary Surgeons and the prestigious Clinical Society of Genitourinary Surgeons.