Mitchell R. Humphreys, MD, presented “Updates in LUTS: Treating Overactive Bladder and Nocturia” during the 28th Annual Perspectives in Urology: Point Counterpoint on November 14, 2019 in Scottsdale, Arizona.
How to cite: Humphreys, Mitchell R. “Updates in LUTS: Treating Overactive Bladder and Nocturia” November 14, 2019. Accessed Jul 2025. https://grandroundsinurology.com/updates-in-luts-treating-overactive-bladder-and-nocturia/
Updates in LUTS: Treating Overactive Bladder and Nocturia – Summary:
Mitchell R. Humphreys, MD, describes the shifting landscape of lower urinary tract symptoms (LUTS) management from a symptom-focused approach to a paradigm of altering the underlying disease progression. He focuses on changes in the medical management of nocturia and bladder outlet obstruction due to benign prostatic hyperplasia (BPH).
Abstract:
The traditional treatment of BPH focuses on removing obstruction and alleviating bothersome LUTS. However, this focus is now shifting to altering the disease progression and preventing complications associated with BPH-driven LUTS.
This shift has been reflected in changes in the medical management of these patients since 1993, in part due to FDA approval of novel medications such as alpha1-adrenergic blockers and newer uroselective agents in this class. Additionally, PDE 5 inhibitors can address LUTS by reducing urgency via afferent nerve modulation. Anticholinergic agents are now considered effective treatment alternatives for LUTS secondary to BPH, but should be used with caution in patients with a post-void residual greater than 250-300 mL. Finally, beta-adrenoceptor blockers have been shown to increase the storage capacity in the bladder, improving urgency, frequency, and quality of life.
Beyond BPH, LUTS include a broad range of diagnoses and storage, voiding, and post-micturition symptoms. Of these, nocturia, defined as voiding two or more times nightly, is one of the most common and the most bothersome.
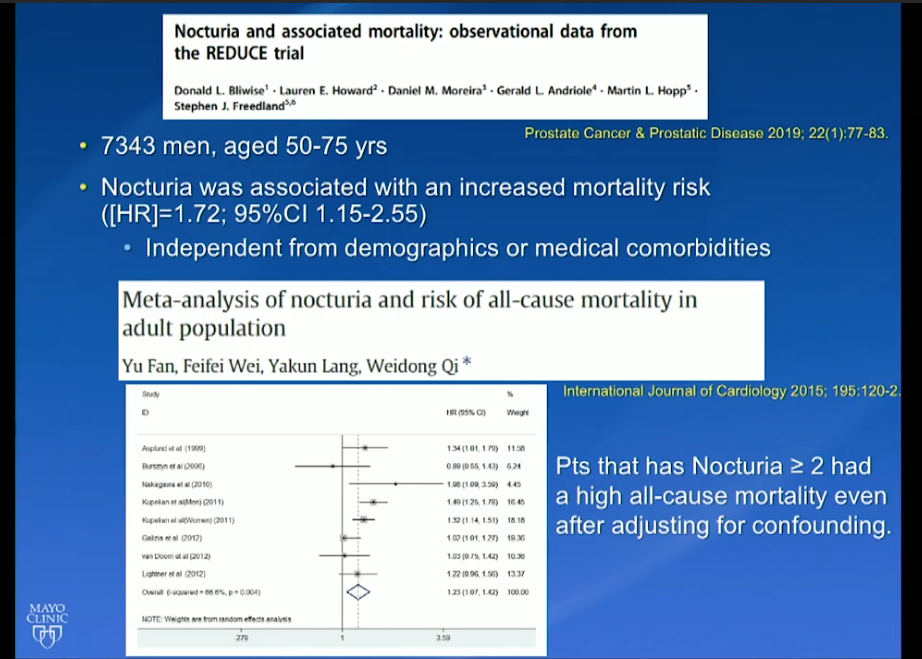
Data from the REDUCE trial indicated that nocturia was associated with an increased mortality risk, independent from demographics or medical comorbidities. While the REDUCE trial did not specifically focus on nocturia, and investigators defined nocturia as three or more voids per night, other researchers have found that patients with nocturia have a high all-cause mortality rate. This suggests nocturia, rather than being a disease in and of itself, may be a symptom of a serious physiological problem.
Traditionally, treatment focusing on reducing nocturia’s impact has featured behavioral strategies like reduction in fluid intake, double-voiding prior to bedtime, and urge suppression, among others. Recent efforts to find medical solutions led to the 2018 approval of the desmopressin analogs Nocdurna and Noctiva, which both carry risk of severe hyponatremia, but can reliably reduce symptoms.
About Perspectives in Urology: Point Counterpoint
Perspectives in Urology: Point Counterpoint (PCP) is an annual, multi-day, CME-accredited conference devoted to discussing and debating the latest topics in men’s health and general urology, as well as management of bladder, renal, and both localized and advanced prostate cancer. More than didactic lectures, the conference’s format includes debates, point-counterpoint discussion panels, and unique case-based presentations. Dr. Humphreys presented this lecture during the 28th PCP in 2019. Please visit this page in order to register for future PCP meetings.
ABOUT THE AUTHOR
Mitchell Humphreys, MD, is a Professor and Chair of the Department of Urology at the Mayo Clinic in Scottsdale, Arizona. He holds dual appointments in the Department of Urology in the Mayo College of Medicine and in Clinical and Translational Sciences in the Mayo Graduate School. In addition, he serves as the Dean of the Mayo Clinic School of Continuous Professional Development and as the Endourology Fellowship Director. Dr. Humphreys completed his residency at the Mayo Clinic in Rochester and an Endourology and Stone Disease Fellowship at Indiana University. Since that time, he has been on staff at the Mayo Clinic in Arizona. His clinical focus is on surgical and metabolic stone disease, BPH (with a special focus on HoLEP), and minimally invasive GU oncology. In addition to the publication of over 100 peer-reviewed manuscripts and multiple book chapters, he is a journal editor and reviewer for several international urology journals. He is an active member of the Endourology Disease Group for Excellence (EDGE) research consortium. Outside of his work with the Mayo Clinic, he serves on the Board of Directors of GSD Healthcare, LLC, promoting basic healthcare initiatives in underserved and impoverished areas around the globe. He also serves as a member of the Columbia College Board of Trustees.