Dr. Peter Black, MD, FRCSC, presented “Perioperative Pathways—What We Know Works” at the 2nd Annual International Bladder Cancer Update on January 27, 2018 in Beaver Creek, Colorado
How to cite: Black, Peter. “Perioperative Pathways—What We Know Works” January 27, 2018. Accessed Apr 2025. https://grandroundsinurology.com/Perioperative-Pathways/
Summary:
Peter Black, MD, FRCSC, provides an overview of the current Enhanced Recovery After Surgery (ERAS) protocol in the setting of radical cystectomy, recommendations from the ERAS Society, and how the practice increases bladder cancer patients’ quality of life. He also touches upon the possibility of adding alvimopan to ERAS protocol in the near future.
Reveal the Answer to Audience Response Question #1
Which of the following is not a recommended component of standard ERAS protocol?
- A. Intraoperative goal-directed fluid administration
- B. Avoid post-operative nasogastric intubation
- C. Intravenous PCA for pain control
- D. Post-operative gum chewing
- E. Auditing of protocol compliance and outcome
Answer Explanation:
The answer is Option C. We want to avoid systemic narcotic use, so we try to avoid the PCA.
Reveal the Answer to Audience Response Question #2
Case Study: A 72-year-old female is preparing for radical cystectomy and ileal conduit. Which of the following is not part of the instruction package for optimal GI tract management?
- A. Preoperative mechanical bowel prep before cystectomy conduit.
- B. Preoperative oral carbohydrate loading.
- C. Clear fluids recommended up until two hours before induction of general anesthesia.
- D. Post-op nausea/vomiting prophylaxis.
- E. Early oral nutrition starting on the day of surgery.
Answer Explanation:
The evidence would suggest that we don’t need to do mechanical bowel prep any more before cystectomy and conduit.
Perioperative Pathways—What We Know Works – Transcript
Click on slide to expand
Disclosures
So getting right into the talk, these are some disclosures. I highlight Merck here because I had worked with Merck Canada on bringing alvimopan into Canada, which is not yet on the market.
What is ERAS?
I’m going to start with—I’m going to go over what is ERAS, and I’m going to talk about some of the individual elements of an ERAS protocol, where the evidence is, and then I will finish off just showing overall the evidence of any given ERAS protocol in the cystectomy population.
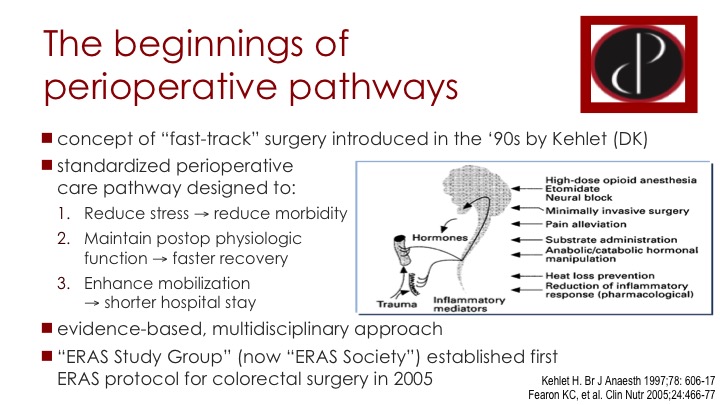
The Beginnings of Perioperative Pathways
So the ERAS protocols go back to the so-called fast track surgery pathways. Back in the 90s, so it’s not that old really, comes primarily from Scandinavia, Denmark, Sweden, and also a lot from the UK, and the idea was that if you standardize perioperative care before, during, and after surgery, that you could reduce the stress on the patient and thereby reduce the morbidity and enhance the recovery. You would maintain patient physiology as best as possible to hasten recovery, and you would hopefully shorten the hospital stay in the process. The idea was to make it evidence-based and to engage all parties involved in the patient care. This evolved into ERAS, enhanced recovery after surgery. There is an ERAS study group, which is now the ERAS Society, and the first protocol they put out was for colorectal surgery in 2005. A lot of what we do in the cystectomy population is based on colorectal surgery and other major abdominal and pelvic surgery.
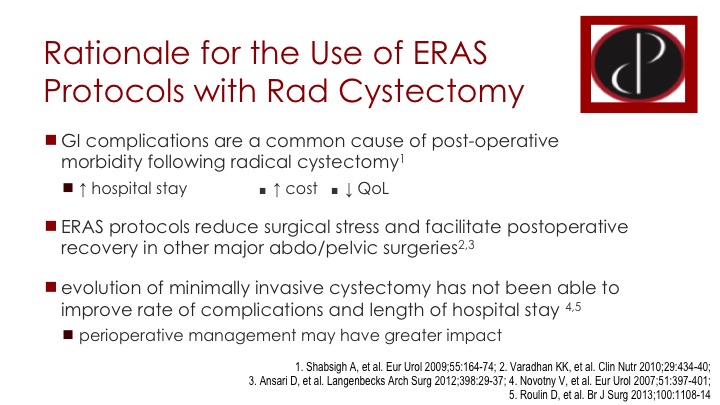
Rationale for the Use of ERAS Protocols with Rad Cystectomy
So why ERAS in the context of radical cystectomy? This is something that we might not consider for example in the context of a partial nephrectomy or other diseases or surgeries but for cystectomy it really makes a lot of sense. GI complications are a big part of our postoperative management of these patients and they cause a lot of concerns, morbidity and cost. They also affect quality of life. ERAS protocols in the other disease sites are able to decrease these complications and facilitate recovery so it makes sense that they should work also in the cystectomy population. In the cystectomy setting it looks like minimally invasive surgery doesn’t have as big an impact as it might in other settings. So we really need to rely on better perioperative management, and not just a switch to laparoscopy or robotics.
“Fast Track” Peri-op Care Plan for Radical Cystectomy
Sam Chang at Vanderbilt and Raj Pruthi at UNC have been some of the early adopters of fast track perioperative care plans for radical prostatectomy going back more than 10 years at this point with various pre-op, intra-op and post-op parameters that I will come to.
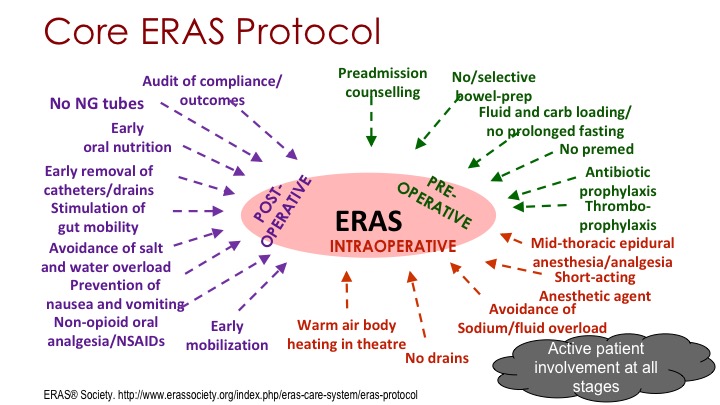
Core ERAS Protocol
If you look at the core ERAS principles that the ERAS Society puts out, there are 20 individual items on this slide that you can roughly divide into the same pre-op, post-op, intra-op, and the evidence for any given one may not be that solid, but together we would consider this the optimal management of these patients, and we want to remember that the patient, him or herself always has to be in the foreground and has to be involved in all stages of this protocol.
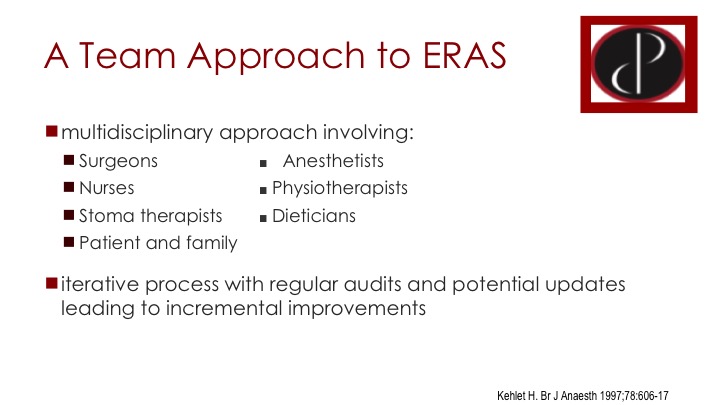
A Team Approach to ERAS
A key to highlight is the fact that it really requires multi-disciplinary engagement. It’s not just up to the urologist or the surgeon. You need the nurses, pre-op nurses, intra-op nurses and up on the floor, post-op, the stoma therapists, the physiotherapists, the anesthetists of course are critical. It involves a lot of different parties and ultimately to institute or implement successful ERAS protocol in your hospital you will need buy-in from the administration to get all of these parties together to make it happen.
Also important to highlight is that it is an iterative process that needs to be audited regularly to make sure that compliance is happening to see where the issues are and potentially update the protocol as the evidence evolves.
The evidence for individual ERAS components
What is the evidence for the individual ERAS components?
Clinical Nutrition
Well the ERAS Society put out the summary document, a guideline for cystectomy ERAS back in 2013.
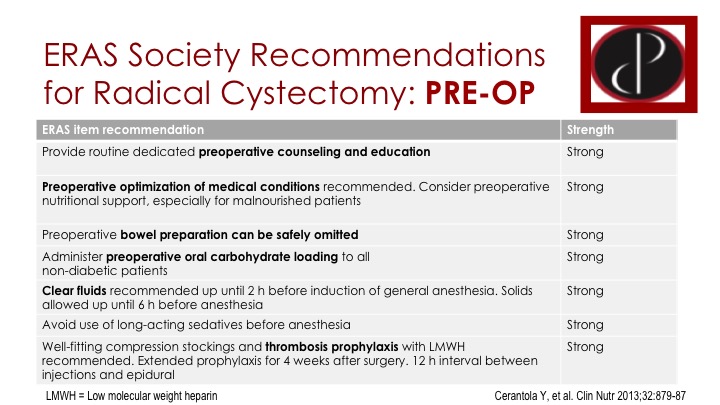
ERAS Society Recommendations for Radical Cystectomy: PRE-OP
A lot of the evidence is really from the colorectal surgery domain, and they rate their recommendation simply as strong or weak levels of evidence. There is a list here. These are seven different parameters that are considered important in the pre-op setting. Some of these will be very familiar with you. The first one, counseling, education is an important part of it. Medical optimization of course is something that we take for granted these days. Bowel prep can be omitted. I think that is important, but most of us have advanced to that. Preoperative oral carbohydrate loading, I will show you a little bit of data on that. I think that is something that probably few centers are doing, but the evidence is fairly compelling. And then there are other things in there as well.
Pre-operative Bowel Prep: Evidence in Cystectomy
If you look at the bowel prep, again it’s being standard of care for colorectal surgery for a long time not to do a bowel prep, and there are only a couple of studies in the cystectomy population that are relatively low quality studies, but they reinforce that it is not important to do a bowel prep, and you are not taking a risk by not doing it. First study was only 62 patients, they had a three-day standard bowel prep versus just going NPO eight hours before surgery, and there is no difference in morbidity or length of stay. A second study of 86 patients again a standard bowel prep versus no bowel prep and there is really no difference so these studies are both highlighting the fact that it is not dangerous not to do a bowel prep, but there is some evidence that it might actually be beneficial to avoid the bowel prep, that it is better for bowel health and better for bowel recovery. So the ERAS Society clearly recommends not to do a bowel prep.
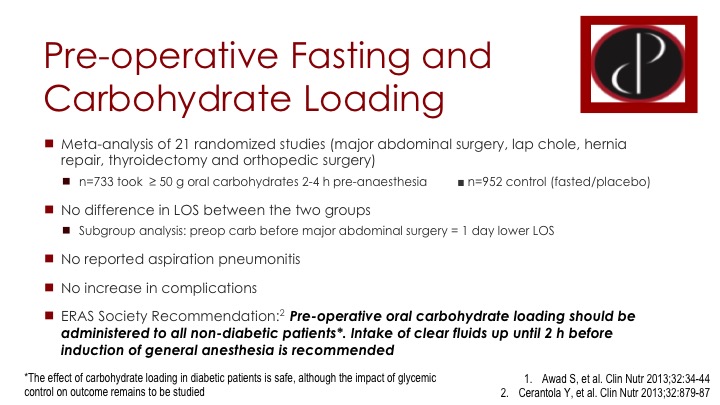
Pre-operative Fasting and Carbohydrate Loading
The carb loading and lack of fasting pre-op I think this has taken our anesthetists, anesthesia colleagues a while to warm up to this idea, and I think if you introduce it in your hospital, they really need to take a look at the evidence and convince themselves but there is this meta analysis, which is already several years old. This is from 2013, and it looked at 21 different studies of quite a variety of different surgeries, not just major abdominal surgeries, but also other things like thyroid and orthopedic surgery, and there are about 700 patients who had preoperative carb loading compared to 900 patients who did not, they were fasted in the usual manner, or some of them even had a placebo, basically water loading. There was no difference in length of stay between the groups as a whole, but there was a decreased length of stay for the patients with major abdominal surgery who had the preoperative carb loading. There was no aspiration pneumonitis and no increase in complications, and those are both important points because you would worry of course that you might have complications from having stomach contents at the time of induction of anesthesia. So it is considered very safe and considered potentially beneficial again for post-operative bowel recovery.
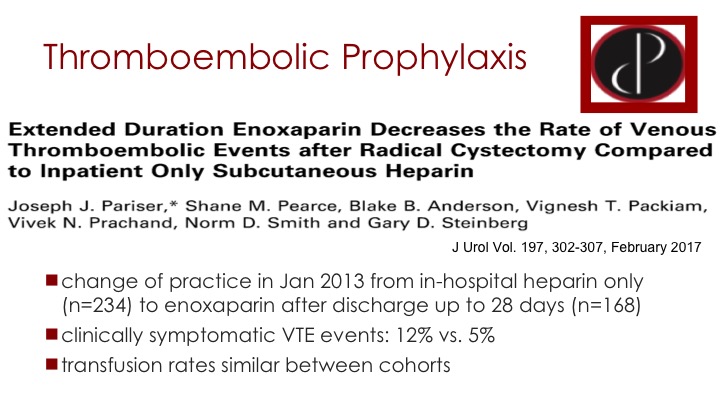
Thromboembolic Prophylaxis
This I’m just going to jump over. The thromboembolic prophylaxis is obviously an important part of ERAS, but I think Joni has really discussed that in detail.
ERAS Society Recommendations for Cystectomy: INTRA-OP
For intraoperative parameters here we are again more relying on our anesthesia colleagues. The first point on this list is thoracic epidural, and it’s interesting the group at USC have been big proponents of ERAS and have published a lot on ERAS, and they actually consider lack of epidural as a key component of their ERAS protocol because they use regional block with a tap block or a rectus sheath catheter. So there are alternatives. The idea with the epidural is you are avoiding systemic narcotics, but if you are putting narcotics into your epidural you may end up with the same problem. Minimally invasive approach is important in a lot of surgeries, maybe not as important for cystectomy. If it is, it is just one element in the ERAS protocol and not the key element by any means. Another thing on this list is this goal-directed fluid therapy and in our protocol in Vancouver, it has been the one component that we have had the most difficulties with as far as compliance. There are too many anesthetists, each one does it a little bit differently and ultimately they are not doing the fluid resuscitation intraoperatively based on objective measures.
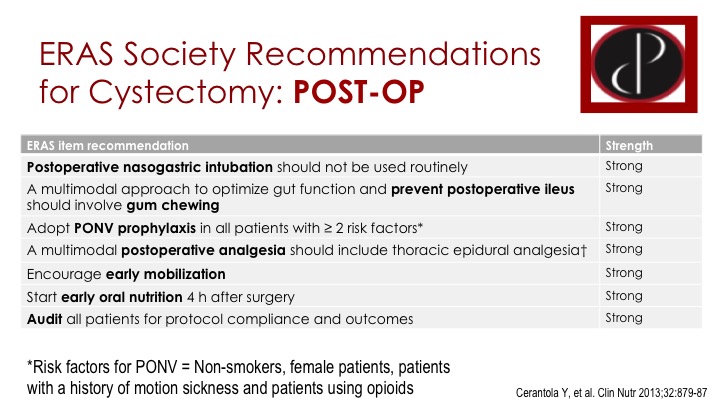
ERAS Society Recommendations for Cystectomy: POST-OP
Post-operatively these are things that again are followed more in our domain as the surgeons. We certainly want to avoid the post-operative NG tube. I’ll show you some data on that. There are measures to prevent ileus including gum chewing, and there is some data, which I will show you, early mobilization is I think a no-brainer these days. And we like to start nutrition early, and I think this is one thing in the cystectomy population that may differ from the colorectal population. I think it is more difficult to start feeding patients earlier, they are more likely to end up with nausea and vomiting if you give them too much too soon.
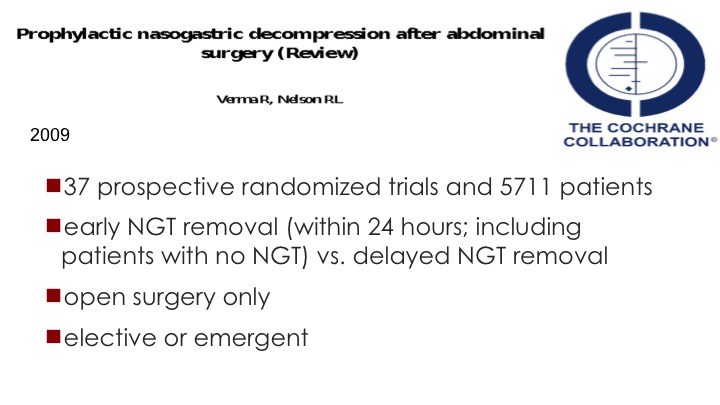
Prophylactic nasogastric decompression after abdominal surgery (Review)
The NG tube, I think most of us have abandoned this now a long time ago. I know when I was a resident it was still very popular, but things have changed. This was a Cochrane review of 37 prospective randomized trials in over 5,000 patients, not necessarily including any cystectomy patients but it compared early NG tube removal within 24 hours and this includes patients who had no NG after surgery versus delayed NG removal. It was only open surgery, and it could be elective or emergent.
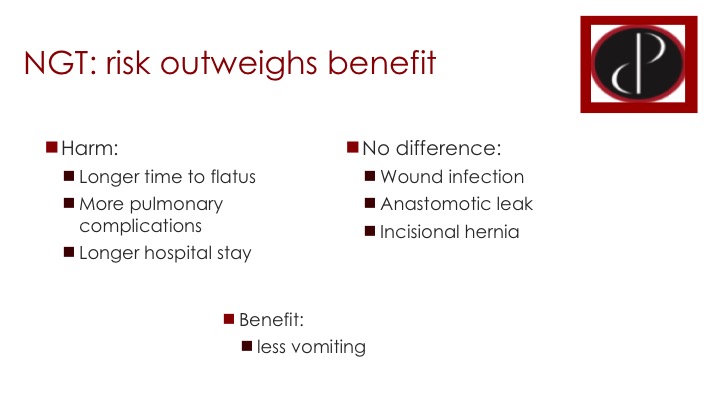
NEPHROLOGIST: Risk Outweighs Benefit
There are a lot of forest plots in this review paper but I have summarized them just here. There are clearly some harms with an NG tube, with leaving it in after surgery. So the time to flatus across these studies was clearly increased. There were more pulmonary complications with an NG tube, and the hospital stay was longer. There was no difference with respect to wound infection, anastomotic leak, or incisional hernia. The benefit of leaving the NG tube in there was less vomiting, but overall the risks clearly outweigh the benefit.
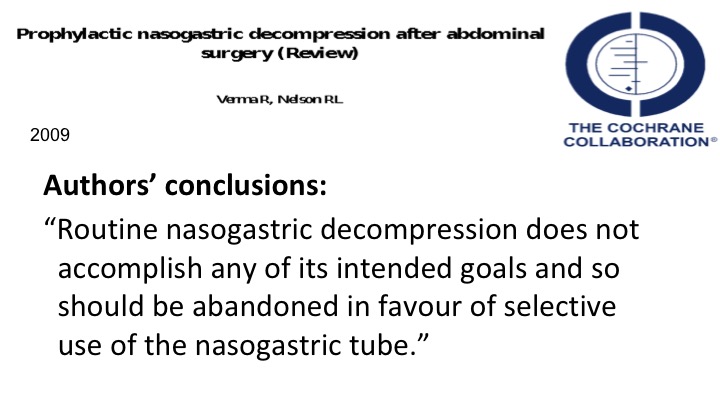
The Cochrane Collaboration
The author’s concluded, “Routine NG decompression does not accomplish any of its intended goals and so should be abandoned in favor of selective use of NG tube.”
Gum Chewing
Gum chewing is very simple. Our biggest obstacle to gum chewing is that the hospital doesn’t provide it so the patients have to get it themselves. But it’s so easy to do. There are two trials that have looked at this, one in Asia, I think it was in Korea and the UNC group has also looked at it. One of the trials was with an ERAS type protocol, and the other was not ERAS so the gum chewing was the only difference. Patients had quicker return to flatus and first bowel movement, no difference in morbidity and length of stay. I don’t think we can expect too much from gum chewing, but it is so easy to do. And there might be a quality of life benefit with the time to flatus and BM.
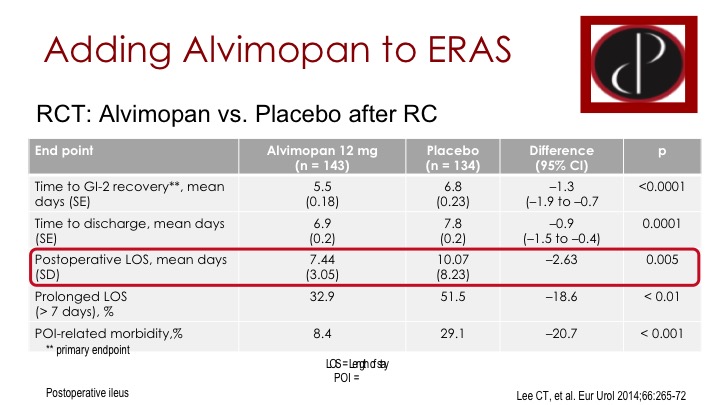
Adding Alvimopan to ERAS
Now, Alvimopan has not entered into the ERAS Society protocol because it is newer than the protocol but it of course has also become an important component in the US and wherever it is approved. This is a Phase III trial in a sort of ERAS protocol, so this was multi-centers across the US. Cheryl Lee led it from Michigan. I know USC and MD Anderson were in it, I’m not sure if Mike and Sam if you guys were part of it as well. So there were components of ERAS, but it wasn’t a complete ERAS protocol, and then it was either patients were randomized to alvimopan or placebo. There are some very important endpoints here that were improved with the alvimopan. So time to recovery of bowel function, essentially time to discharge, hospital stay were all improved and even the post-operative ileus related morbidity was improved.
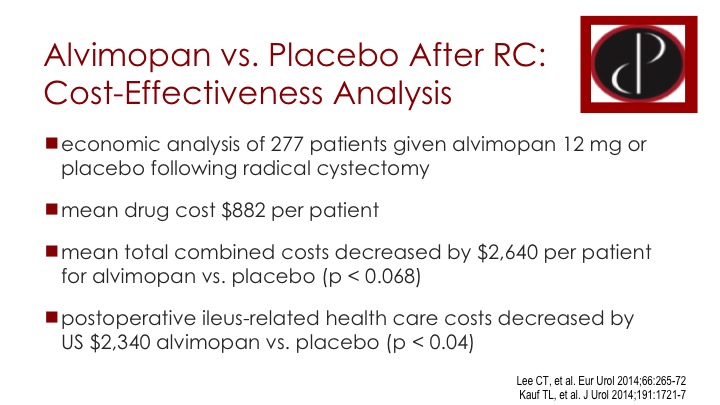
Alvimopan vs. Placebo After RC: Cost-Effectiveness Analysis
It costs approximately $100 a day, and it’s given on the day of surgery and once daily as long as the patient is in the hospital. so if the patient is in the hospital approximately 7 days, it’s approximately 7 or here in the study $880, and the cost analysis showed that the use, this additional cost is more than compensated by cost savings due to decreased complications, particularly around the post-operative ileus.
ERAS outcomes after radical cystectomy
What about if we put this all together in actual ERAS protocols? What does the evidence tell us about ERAS versus no ERAS in radical cystectomy? There are several reports in the literature. These are papers that came out prior to 2015 and were summarized in this 2016 paper, and the big criticism is three-fold First of all a lot of it is based on colorectal surgery evidence as I suggested. Second of all, you can see in the last column the number of ERAS items. Everyone is doing it a little bit differently. It’s fairly arbitrary and inconsistent. And then the third thing is there is a real lack of prospective data, and that hasn’t really changed I would say in the last couple of years.
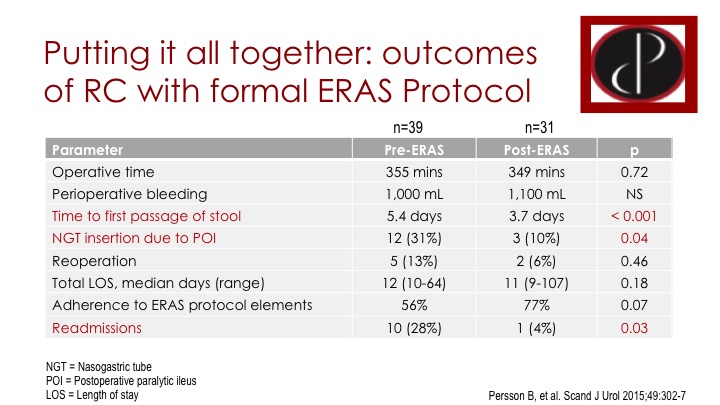
Putting it all together: Outcomes of RC with Formal ERAS Protocol
There’s a lot of this type of study. This is from Sweden where they compared their pre-ERAS population to their post-ERAS after introducing an ERAS protocol. They compare outcomes, and a lot of people have done this and published on it. In their relatively small series, they note that ERAS improves time to first bowel movement. It decreases the risk of NG tube insertion, and it reduces the rate of readmissions, which are all important outcomes.
Auditing of a Successful ERAS Protocol for Open Radical Cystectomy
Another trial, this is from the Southampton Group. They actually looked at sort of the auditing, and how they can improve their protocol. Again, it’s a retrospective review, they introduced ERAS in January 2011, and they saw a clear benefit compared to their pre-ERAS population, so length of stay decreased, it is the UK. Length of stay is longer than here. Time to flatus wasn’t really different. Ileus rate improved. The mean node yield is just an indicator of how they are doing their surgery, and it was the same. But they went back then over a year later did a formal audit, changed some things, all minor things, but hopefully targeting marginal gains, and then they looked at their experience again, and now they have gotten their hospital stay down to 7 days median, their time to flatus is a little bit better. Their ileus rate is even lower, and even though they are doing more of a node dissection, so it just is an example of the process for introducing ERAS.
Real World Experience at USC
The group at USC, so – – and colleagues have been at the forefront of introducing and studying ERAS. They published just recently their experience. This again is a comparison of ERAS versus a prior historic series without ERAS. 145, 144 patients. 65% got a neobladder, which is of course quite different than a lot of the literature, and their protocol includes some of the usual things, but this is one of the only series where alvimopan is actually part of the experience. And as I mentioned, they do not use the epidural at USC.
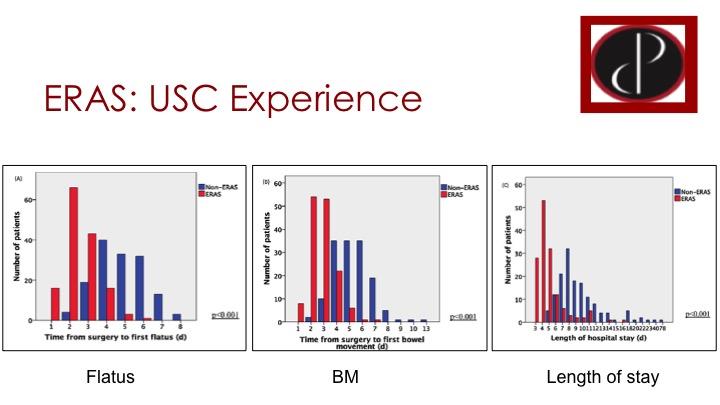
ERAS: USC Experience
So they were able to show the red are the ERAS patients and blue are non-ERAS. And time to flatus has really been moved up drastically so most patients are passing gas on day 2 and 3 instead of 4, 5, or 6. Patients are having bowel movements on day 2 or 3 again instead of 4, 5, or 6, so a huge improvement compared to the historic control, and the length of stay has also decreased dramatically and most patients are going home on days three to five, which in our environment is certainly not attainable.
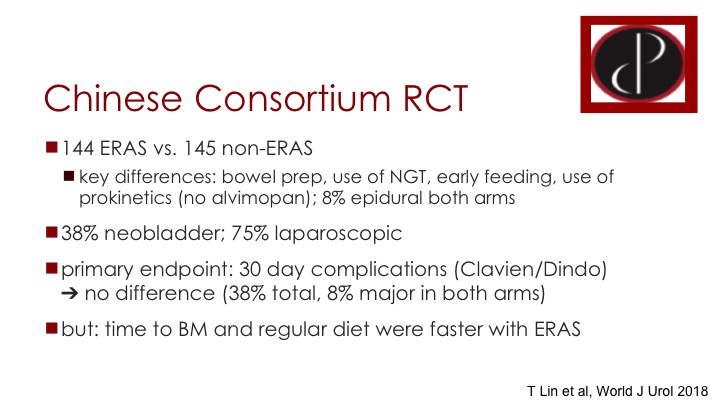
Chinese Consortium RCT
The only sizable randomized trial just appeared in the last couple of weeks, the last few weeks from China. Very interestingly exactly the same numbers as USC published the study, 144 versus 145. But this is multiple centers, over 30 centers in China randomizing to ERAS versus no ERAS. Some of the key differences are things like bowel prep, use of NG tube, early feeding, they do use pro-kinetics in the ERAS arm but no alvimopan, and they don’t use epidurals really in either arm. A good number of neobladder, so more than a third of patients had a neobladder and interestingly almost ¾ or about ¾ of patients had the surgery done laparoscopically. Their primary endpoint was the 30-day complication rate defined by the Clavien/Dindo classification so they did a rigorous analysis of complications and found no difference either overall or in the risk of major complications. They did find improvements in the usual things, bowel movement, regular diet, etc. And of course the implication here is there might be a quality of life improvement related to these factors even though the complication rate was not better.
ERAS Improves Quality of Life
Quality of life has been addressed by this one study. This is a German study from Munich, and they randomized 101 patients 2:1 ERAS versus a regular regimen. They see improvements again in a lot of the same things including wound healing disorders, fever, thrombosis, etc., but they also looked at quality of life day 3, day 7 and at discharge. Patients of course stay a little bit longer in Europe, and without going into any one of these in detail you see that there is a clear improvement in quality of life by this EORTC QLQ30 questionnaire, with the ERAS, which I think is very important.
Conclusions
So in conclusion GI complications are very common after cystectomy and can cause a lot of morbidity, prolonged hospital stays and increase cost. ERAS protocols are effective in reducing some of these complications, reducing length of stay and hopefully also in saving cost, and I think any hospital doing a significant number of cystectomies should be looking at introducing an ERAS protocol and engaging a multidisciplinary team to optimize outcome.
Acknowledgements
I just want to acknowledge that a lot of the slides here I’ve borrowed from an ERAS educational program that I helped put together with a CUA committee, Canadian Urological Association Committee that was funded by Merck. That’s it. Thank you.
Question from the Audience #1:
In medical oncology we all turn off our brains and use one click that calculates doses, timing, use of things like Neulasta and so forth in our protocols and this looks like it’s very amenable to that sort of introduction, particularly if you have a clinical trial protocol type software like EPIC or whatever goes with EPIC. Do you know if that has been instituted because nobody wants to go through all that click list and make sure every one of those things, that is how—it looks very compelling to me as a non-surgeon. You would think it could be easily introduced as an automated sort of perioperative procedure.
Dr. Black’s Answer:
We don’t have EPIC or Serner and maybe Mike can comment on that, but for us it is paper-based orders, it’s all standardized order sheets. You just sign it. You add the patient’s own medications and otherwise you just sign it, and I imagine that you may have the same in your electronic medical records.
Comment from Dr. Michael S. Cookson:
Yeah, so we don’t have EPIC yet. Sam just recently converted to it, but at Vanderbilt Sam was involved with and so was I in these clinical guidelines that lend themselves well to the impatient setting and so that works out pretty well and all of our residents it has reduced a lot of variability in the management, reduces labs, and that is incorporated into it, but I don’t know about EPIC because I don’t have it yet.
Question from the Audience #2:
Can you comment on any of the cardiac issues that have occurred with alvimopan in your studies?
Dr. Black’s Answer:
I don’t think I can. As far as I know, I thought it wasn’t thought to be a big concern. I know there is always excitement early on.
Question from the Audience #3:
In the phase 4 study that we did, so there was concern with the cardiac issues initially, there was the black box warning. But the phase 4 study that we did and several of us were a part of it, it was powered to detect any differences, and if you actually look at it, it ended up being underpowered but it showed a benefit alvimopan in cardiac outcomes, so patients on alvimopan actually had lower incidence of cardiac adverse events which obviously is a statistical anomaly but it doesn’t really affect the cardiac outcomes. That was for—all it is approved for is in-hospital use. For the longer-term methadone, that I don’t know what the data there is, but for our patients it is only approved for short-term use.
Dr. Black’s Answer:
I think there are lot more studies in other disease sites as well, so I think the cumulative evidence would suggest that it is not a concern.
Question from Dr. E. David Crawford:
I have another quick question. I was unsure about your support for epidurals in the pathway.
Dr. Black’s Answer:
I highlighted the fact that a lot of people are not keen on epidurals. We still do epidurals routinely. We actually just finished a prospective randomized trial epidural versus rectal sheath catheter and the epidural gives better pain control. And the risk of adverse outcomes is about the same, the risk of ileus and other complications is the same. So the result of our trial is that we’re going to continue to do epidurals. I think the epidurals are truly advantageous if you can avoid use of narcotics in the epidural and ultimately the patients end up getting a fair amount of fentanyl. So you are still seeing ileus related to that.
Dr. Crawford:
My feeling is—I’ve been through them several times and every time a new anesthesia group comes on they want to, oh, epidurals. – – they delay surgery, two, it’s expensive, three, sometimes you see people don’t get up and ambulate, I think the ileus is—I don’t want to use that word ileus after yesterday but delay in bowel movements are with epidurals are there, and also I mean you can also just infiltrate in the incision with bupivacaine or local anesthesia and that works pretty well too. That is what I do in my radicals but.
Dr. Black:
I think it works great for a radical but for cystectomy I mean our trial would suggest that epidural works better. But we haven’t presented or published the data yet.
ABOUT THE AUTHOR
Dr. Peter Black is a urologic oncologist at Vancouver General Hospital, a research scientist at the Vancouver Prostate Centre, and a Professor in the Department of Urologic Sciences at the University of British Columbia (UBC). He received his undergraduate degree from UBC and his medical degree from Johannes Gutenberg University in Mainz, Germany. He completed his urologic training at the University of Washington in Seattle and a Fellowship in Urologic Oncology at MD Anderson Cancer Center in Houston, Texas. He has a clinical subspecialty interest in bladder cancer. He maintains a grant-funded translational research program in urothelial carcinoma and is an active cancer clinical trialist in this field.