John F. Ward, MD, presented “Does the PROMIS Trial Impact Prostate Cancer Screening?” during the 24th Annual Southwest Prostate Cancer Symposium on April 11, 2019 in Scottsdale, Arizona.
How to cite: Ward, John F. “Does the PROMIS Trial Impact Prostate Cancer Screening?” April 11, 2019. Accessed Feb 2026. https://grandroundsinurology.com/does-the-promis-trial-impact-prostate-cancer-screening/
Does the PROMIS Trial Impact Prostate Cancer Screening? – Summary:
John F. Ward, MD, FACS, discusses methods to improve prostate cancer detection in a way that avoids overdiagnosis. He focuses on multiparametric MRI (mpMRI) and the evidence evaluating its ability to guide biopsy targeting, or potentially allow for the avoidance of biopsy altogether.
Abstract:
Through the traditional approach to prostate cancer diagnosis, patients with rising PSA who have an initial negative biopsy will continue to receive annual PSA screening and re-biopsies. This persistent routine of testing eventually finds disease. Unfortunately, even if this disease is insignificant and may not require treatment, overdiagnosis may be psychologically detrimental to the patient.
The goal of a contemporary approach to managing a patient with rising PSA is to detect clinically significant disease while avoiding overdiagnosis of insignificant cancers, as well as to minimize the cost, patient discomfort, and complications of biopsy. Also in this paradigm, diagnostic information should guide personalized medicine. Methods developed in an effort to improve this approach include PSA nomograms for assessing prostate cancer risk and increasing the number of biopsy samples, as well as urine, blood, and tissue biomarkers.
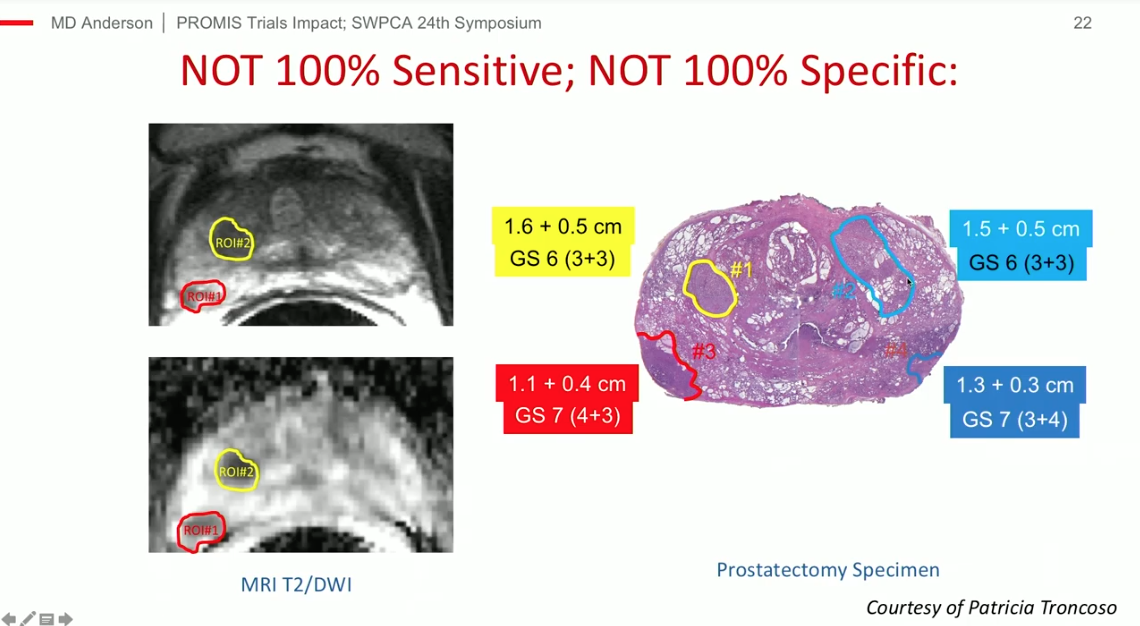
Arguably, a more effective technique for reaching the contemporary goals of prostate cancer detection is image guided biopsy. However, mpMRI remains challenging in terms of image acquisition and interpretation. Furthermore, mpMRI quality is dependent on the hardware and software a center possess, and has limited sensitivity and specificity.
This presentation reviews data comparing targeted and standard biopsy. It also covers evidence about the negative predictive value of MRI and the possibility for a negative MRI to allow patients to avoid a primary biopsy from the PROMIS trial, and data from the PRECISION trial, which compared MRI with or without targeted biopsy to standard transrectal ultrasound-guided biopsy.
About the Southwest Prostate Cancer Symposium
The Southwest Prostate Cancer Symposium (SPCS) is a multi-day conference that seeks to educate urologists, radiation oncologists, medical oncologists, and other healthcare professionals involved in the treatment of prostate cancer. The topics focus on current technical aspects of diagnosis and treatment of localized and advanced disease, particularly regarding imaging, technology, and training in the related devices. Dr. Ward presented this lecture during the 24th SPCS in 2019. In 2020, the 25th SPCS will also offer training sessions involving imaging, scanning, and prostate cancer treatment related devices on site. Please visit this page in order to register for future SPCS meetings.
ABOUT THE AUTHOR
John F. Ward, MD, FACS, is an Associate Professor of Urology in the Division of Surgery at the University of Texas MD Anderson Cancer Center in Houston. He is a clinical scientist with exclusive focus on the management of prostate and testicular cancers. He is recognized as one of the early thought leaders in prostate cancer imaging and focal therapy. His contributions laid the groundwork that has helped this approach gain recognition as an acceptable therapeutic strategy for select patients with prostate cancer. He helped develop ablative techniques using a variety of energy and imaging techniques, and was involved in the early studies of interstitial laser ablation, focal cryotherapy, and high-intensity focused ultrasound, the latter work leading to the FDA US approval. He is equally involved in the development of urine and blood biomarkers of prostate cancer, as well as image-guided targeted prostate biopsy. As a busy clinician, Dr. Ward not only pioneered the MD Anderson Cancer Center Prostate Cancer Imaging and Focal Therapy program while performing 200+ robotic assisted prostatectomies a year, but he also developed the MD Anderson technique of robotic retroperitoneal lymph node dissection, and has now expanded this surgery into the post-chemotherapy setting and as primary treatment for metastatic seminoma.
A native of Pittsburgh, Pennsylvania, Dr. Ward is a Graduate of the University of Notre Dame and Georgetown Medical School. He received his urologic oncology training at the Mayo Clinic in Rochester, Minnesota, before completing a career with the US Navy. He joined the faculty at MD Anderson Cancer Center in 2006.