Gerald L. Andriole, Jr., MD, presented “Image Guided Prostate Biopsy” during the 39th Annual Ralph E. Hopkins Urology Seminar on January 30th, 2019 in Jackson Hole, Wyoming.
How to cite: Andriole, Jr., Gerald L. “Image Guided Prostate Biopsy” January 30, 2019. Accessed Nov 2025. https://Image-Guided-Prostate-Biopsy/
Fluciclovine (18F) PET/CT Impact on Clinical Management of Recurrent Prostate Cancer
Gerald L. Andriole, Jr., MD, reviews the history of conventional transrectal ultrasound (TRUS) guided biopsy and the limitations of this technique that remain in the modern era. He then discusses current and emerging efforts to improve image guided prostate biopsies.
Abstract:
With the advent of ultrasound technology, the use of ultrasound guidance for prostate biopsy began in the mid 1960s. The description of distinct zones in the prostate and the ability to visualize them also informed the conventional TRUS guided biopsy. Initially, there was an expectation that ultrasound could identify prostate cancer as a hypoechoic lesion, but it quickly became clear that this was not so.
There have not been many refinements to conventional prostate ultrasonography since then, except for the addition of cores taken on systematic biopsies. Because of this, TRUS biopsy remains subject to limitations in the modern era. These limitations include the fact that this method is operator dependant and misses significant pathology which often leads to the need for re-biopsy, the issue of under- and overestimating disease grade and extent, as well as the nature of randomly arrayed cores. There is no unified consensus as to the number of cores required for prostate cancer detection, despite efforts to develop nomograms adjusting for patient-specific factors. Furthermore, there are serious complications associated with TRUS biopsy.
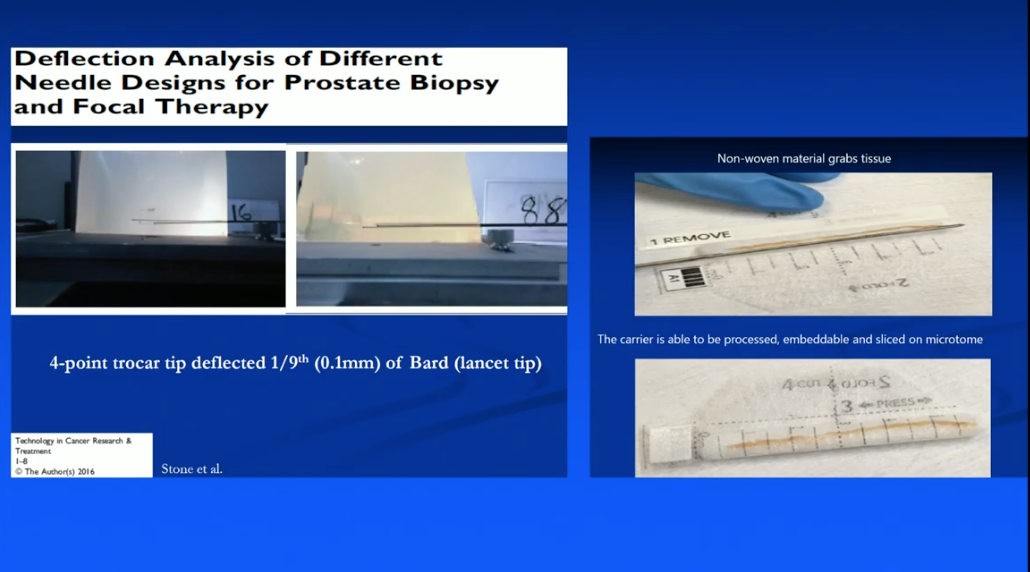
This presentation reviews recent efforts to improve image guided prostate biopsies, such as an in-office transperineal biopsy system, an under-development 3D mapping biopsy system with an enhanced needle design, and micro-ultrasound technology.
As these technologies are not yet widely available, this presentation also discusses current topics in MRI, including the value of cognitive MRI-targeted biopsy, integrating MRI findings into risk calculators, gallium 68 PSMA–11 PET/MRI, as well as the variability of MRI interpretation across radiologists and other unresolved issues.
About the Ralph E. Hopkins Urology Seminar
The Ralph E. Hopkins Urology Seminar, or Jackson Hole Seminars (JHS), is a multi-day conference that focuses on patient safety and cutting-edge updates in the assessment, diagnosis, and treatment of urologic conditions. The topics discussed include urologic cancers, stone disease, urologic reconstruction, female urology, infertility, emerging surgical techniques, and general urology. In addition to didactic expert lectures, this conference features a unique interactive critique panel. Dr. Andriole presented this lecture during the 39th Annual JHS. Please visit this page in order to register for future JHS meetings.
ABOUT THE AUTHOR
Gerald L. Andriole, Jr., MD, is the Chief Medical Officer of Prostatype Genomics AB in St. Louis, Missouri. Dr. Andriole is an internationally recognized key opinion leader in urology with a significant focus on prostate cancer. His research and clinical experience, much of which focuses on genomic testing, allows him to continue to positively impact the quality of care and outcomes for patients diagnosed with prostate cancer.