Dr. Ryan P. Terlecki presented “Prostate Physiology: The Most Diseased Organ in the Male Body” at the 26th Annual Perspectives in Urology: Point-Counterpoint , November 10, 2017 in Scottsdale, AZ
How to cite: Terlecki, Ryan P. “Prostate Physiology: The Most Diseased Organ in the Male Body” November 10, 2017. Accessed Jan 2026. https://grandroundsinurology.com/prostate-physiology-diseased-organ
Summary:
Dr. Ryan P. Terlecki, MD, FACS, outlines prostate physiology and the prostate microbiome, explaining how both lend themselves to a cancer-prone or an infection-prone status, especially as men age.
Prostate Physiology: The Most Diseased Organ in the Male Body
Edited Transcript:
I was glad to be assigned this topic because it was a nice review for me, especially as someone who deals with students, residents, and then a lot of fellow colleagues from the community. So, the title of this lecture was handed to me. When I saw the subtitle “The Most Diseased Organ in the Male Body,” I had to step back and wonder, is it really the most diseased organ?
Now, here are the objectives for this lecture. I’m going to go over relevant prostatic anatomy and physiology and discuss data regarding association between inflammation and benign enlargement in prostate cancer. Then, I’m going to present some data regarding the microbiome of the prostate, which is an exciting area of research at the present, and its potential influence on the state of disease.
To start, I’m going to ask some questions to test your knowledge. Among the soft tissues in the human body, the prostate has the highest level of one certain substance. Which one it is out of zinc, magnesium, cholesterol, prostaglandin E2, and sodium? The answers most people in this room chose were zinc and prostaglandin E2. That’s very interesting.
Okay, here is your next question: Research has noted which of the following in the majority of tested prostate cancer specimens and prostatic intraepithelial neoplasia lesions: E. coli, Klebsiella, Proteus, Candida, or Propionibacter acnes? Most people chose E. colli or P. acnes – very interesting. This is going to be great.
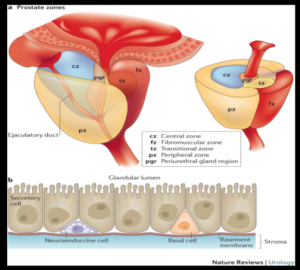
In terms of the anatomy of the prostate, Lowsley, as in the famous Lowsley retractor, initially described the prostate as having five lobes. However, unlike in the rat, humans have distinct zones within a relatively uniform gland. It’s organized like a bunch of grapes, or like alveoli suspended in fibrous gelatin.
There are a variety of cell types in the prostate.
There are secretory epithelial cells which make up the tall, columnar epithelium. They release a lot of proteins. At the base of the secretory cells, there are basal or stem cells. After that, there are neuroendocrine cells. Then, there are a combination of stromal cells including smooth muscle cells, fibroblasts, and endothelial cells.
In this schematic, you see the different prostate zones. The zones urologists talk about most about are the peripheral zone and the transitional zone. This schematic is a layout of the secretory component. You can see the secretory cells and the lumens. At the base, you cans see neuroendocrine cells and basal cells. Then, the basement membrane separates these cells from the stroma.
The basement membrane is composed of extracellular matrix. This membrane is important, not only for structure, but also for its role in developing the gland and controlling cellular functions. It also appears to have a pivotal role in the inflammatory response within the prostate.
Who needs a prostate? Why do we need it?
Well, it’s essential for fertility. You could make an argument that, in present day, you could extract sperm and go the route of ICSI. But, the prostate serves the role as a trigger for ejaculation, activation of sperm, and capacitation.
Now, here is an interesting fact that I either never knew or forgot I knew, until now. Prostate epithelial cells are the only healthy human cells that produce energy by glycolysis, as opposed to the Krebs cycle. We’ll talk about why this may be important for certain areas of research and therapy as we move forward.
The prostatic fluid is not a simple fluid.
It has a number of components. Kallikreins, which includes PSA, were discovered in 1979 and constitute a significant portion of prostatic fluid. It’s also composed of citrate and zinc. The prostate has the highest level of zinc of any soft tissue. There is the answer to one of the questions I asked earlier. Remember that for later. Moving on, prostatic fluid also has spermine, which may protect from infection.
Now, there are also prostaglandins in the prostatic fluid – I don’t know why I didn’t realize this in medical school or residency, but I never put the terms “prostaglandin” and “prostate gland” together. Prostaglandins were named for the prostate, but it’s actually a misnomer. They’re more heavily concentrated in the seminal vesicles.
Cholesterol serves to stabilize sperm. Seminin is the component related to the odor of semen. Finally, you will find acid phosphatase in the prostatic fluid. E. David Crawford and Robert Donohue, who you could say are mature urologists, used acid phosphatase to screen men for prostate cancer in the past.
Why is Zinc important? It gets press for a number of reasons.
Certainly, in fertility, we hear a lot about it. 4% of your body’s total content of Zinc accumulates within the epithelial cells of the prostate. This is possibly supported by prolactin stimulation. Zinc blocks the Krebs cycle and causes citrate accumulation, which is what sperm need for energy.
Zinc also causes temporary inactivity of the kallikreins. The major transporter, called Z1P1, is either decreased or absent in prostate cancer tissue when compared to either normal or BPH tissue. Z1P1 has been hypothesized to be tumor suppressor.
The overwhelming majority of your testosterone in the blood is bound to protein, mainly albumin and sex hormone-binding globulin. SHBG has several different names in the literature now. Only 2% of circulating testosterone is available to diffuse into the prostate. The majority of testosterone is converted to dihydrotestosterone, which has a flatter shape and higher binding affinity for the androgen receptor than testosterone.
So, Dihydrotestosterone (DHT) binds to the androgen receptor and goes to the nucleus. Then, you get transcription followed by ribosomal translation of mRNA. Translation produces a number of proteins. These proteins are cytokines, which include several growth factors, secretory proteins, and enzymes, including PSA. Remember, PSA is a serine protease. These cytokines stimulate cell growth via receptors located on both the epithelium and the stromal cells. The proteins are secreted into the lumen following neurological stimulation at the point of ejaculation.
In this cart oon, you can see that this process starts with a signal from the hypothalamus. So, GNRH, sometimes called LHRH, will then stimulate the pituitary to release a luteinizing hormone, which then goes to the testicles. The Leydig cells in the testicles release about 90 % of the man’s testosterone, but 10 % comes from the adrenal glands.
oon, you can see that this process starts with a signal from the hypothalamus. So, GNRH, sometimes called LHRH, will then stimulate the pituitary to release a luteinizing hormone, which then goes to the testicles. The Leydig cells in the testicles release about 90 % of the man’s testosterone, but 10 % comes from the adrenal glands.
Testosterone then diffuses and converts to DHT by 5α-reductase. DHT binds to the androgen receptor. The heat shock protein is displaced. The androgen-receptor-bound DHT enters the nucleus, where transcription, translation, and a lot of other great things we’ll talk about in more detail later, happens.
This is regulated through androgens.
The gene for the androgen receptor is referred to as a master gene in prostate physiology. There are two forms, A and B, that can be transcribed. As of yet, there’s no evidence for different roles for these two forms. The expression is essential for homeostasis, or for keeping everything in balance. When we talk about relative hormone concentrations or targeting the prostate, we are essentially talking about a battle to keep the status quo. Over 300 androgen receptor mutations have been identified in prostate cancer cell lines.
As men age, testosterone levels, and therefore, dihydrogen testosterone levels, go down, impairing gland functions. This reduces the ability to maintain healthy levels of zinc, citrate, and kallikreins. Fertility reduces in many men and weakens the ability to inhibit the Krebs cycle, which then favors a cancer-prone status.
We know from studies on eunuchs that, in addition to their wonderful voices, the prostate doesn’t grow in prepubertal castrates. Also, castration in mature males will cause gland regression, mainly through apoptosis. This is actually reversible with androgen replacement. It’s been shown that if you expose female embryos to androgens, they will develop prostates.
As I mentioned about hormone regulation, estrogens act in concert with androgens to promote and inhibit growth. There’s an estrogen alpha receptor and an estrogen beta receptor. They’re concentrated in different areas of the prostate and appear to have different functions.
In terms of innervation, adrenergic and noradrenergic receptors within the prostate are typically well known by providers. Everyone’s pretty familiar with using alpha blockers, for example. Recent research also shows that, with norepinephrine, for example, you can accelerate metastasis of prostate cancer in animal models. So, you may want to send your cancer patients to yoga or something.
There’s evidence for multiple muscarinic receptors within the prostate, namely M1, M2, and M3. They’re located in different areas. Data suggests these receptors may modulate growth in the prostate cancer setting. Cholinomimetics have been shown to contribute to proliferation. I’ll talk more about anti-cholinergics as they relate to benign disease later on today.
Regarding immunoactivity, the prostate is an immunocompetent organ, similar to the lung and the intestine.
It’s populated by lymphocytes, macrophages, and mast cells. The immune responses in the prostate tissue are likely influenced by sex hormones. This can affect susceptibility to inflammation.
Remember, we talked about the fact that lymphocytes secrete cytokines. These regulate growth, both within the stroma and in the epithelium. Both are paracrine mechanisms and autocrine mechanisms.
When we start to discuss hormone regulation and immunoactivity clinically, remember that estrogen is pro-inflammatory. Obesity is associated with higher estradiol levels and higher inflammation. So, relate that to metabolic syndrome. There’s some data suggesting that lower urinary tract symptoms improve with reduction in obesity.
Through the course of this talk, I’m speaking to a room of urologists, of whom I assume are predominantly clinical. I think that going through this information helps to prepare you for your reading as it comes through the pike of current research and therapeutics. I know it does for me, as someone who doesn’t primarily treat cancer. I’m trying to tie in some current research and therapeutics as we go, as I have found this has been helpful for me.
Can we call the prostate the most-diseased organ?
It is the number one non-skin cancer, and the number two cancer killer in men, after lung disease. Wael Sakr, who was at Wayne State where I did residency, got funding and did autopsy studies. This was quite some time ago. The autopsy date demonstrated invasive cancer in 64 % of men approaching 70 years of age. He categorized the data by decade, and the percent of invasive cancer in men gradually went up as they aged.
This led to the comment that, “If we live long enough, we all get prostate cancer.” BPH is the most common urologic disease in older men. Therefore, this is a highly relevant sub-specialty in primary care. Nearly 50 % of men in their 80s have BPH.
Prostate cancer and BPH generally, not always, form in different areas of the prostate. Remember the review of different zonal anatomy earlier. Prostate cancer and BPH are considered chronic diseases with slow progression. Their prevalence rises with age. Both are hormone dependent, and both have been associated with inflammation.
Prostatitis is a real condition in some men, but a lot of times, it’s a diagnosis that gets attached to some men when we’re not sure what’s going on. Men could have bothersome symptoms. It could be pain, or it could be a urinary symptom. It could be a histologic diagnosis, which technically, it should be.
Prostatitis’s prevalence is 5 to 13 % in the United States. Over 2 million hospital visits per year are attributed to this condition. It was seen in over three-quarters of the men on the REDUCE trial. There are a variety of classifications for prostatitis: acute and chronic bacterial, inflammatory, noninflammatory, and asymptomatic. It was suggested to be causative for BPH as early as the 1930s.
What about prostatitis’s relationship to cancer? Well, in the California Men’s Health Study, in which nearly 70,000 men were involved, the relative risk was 1.3. This was significant. If the men had a longer duration of prostatitis, they had even higher risk. Then, a meta-analysis of 20 studies also showed a significant association.
Research has shown that daily intake of NSAIDs, primarily aspirin, has been associated with a 39 to 66 % risk reduction for prostate cancer. This was surprising to me, but if you tie inflammation and cancer together, it somewhat makes sense. By a show of hands, how many people advise men to consider NSAIDs for cancer prevention? Yeah, so nobody, right? The data is there, but whether or not it’s quality data, and whether or not it’s had any impact on practice patterns, appears unlikely.
What about the prostate microbiome?
We now have the ability to do an analysis through molecular-based assays. The prostate is not a sterile environment, just like how the urine is not as sterile as we thought it was according to data. The bacterial populations within the prostate seem to differ in the settings of benign and malignant disease. It’s unclear, however, which promotes which. Does one type of environment favor certain types of bacteria, or do the bacteria change the environment?
The concept of infection resulting in cancer is not a new concept. Think about Virchow’s triad back in the 1800s. We’re all familiar with the example of H. pylori as it relates to gastric disease. Now, this relationship was first proposed for prostate cancer back in the early 1950s. Some association between prostate cancer risk and gene variance of COX-2, RNASEL, and toll-like receptor protein 4 have been identified in cases of hereditary prostate cancer.
Just to review, when you think about COX-2, you’re thinking about inflammation. RNASEL is mostly for protection against viral disorders through the interferon pathway. Toll-like receptor 4 recognizes the LPS, or the lipopolysaccharides, of gram-positive and gram-negative bacteria. In radical prostatectomy specimen analysis, it has been shown that over 70 % of specimens contain Enterobacter.
Let’s talk about Propionibacterium acnes, or P. acnes. It is abundant in prostate tissue. It’s also abundant within vaginal tissue, and frequently found in the urine. Its population is increased by men taking testosterone. Think back to puberty.
P. acnes has a pro-inflammatory role, has been associated with prostate cancer, and has been found absent in normal tissue. It’s been suggested as both an initiator or a promoter for disease. It’s been reported in 78 to 95 % of prostate cancer specimens and 100 % of PIN lesions, and is predictive of cancer on subsequent biopsies for elevated PSA.
Okay, so let’s ask our questions from the beginning again and see how well we do. Among the soft tissues in the human body, the prostate has the highest level of one certain substance. Which one it is out of zinc, magnesium, cholesterol, prostaglandin E2, and sodium? See, if I make the questions easy, it makes me look like a good teacher. Awesome, everybody chose Zinc. That is correct.
Let’s go to the next one. Research has noted which of the following in the majority of tested prostate cancer specimens and prostatic intraepithelial neoplasia lesions: E. coli, Klebsiella, Proteus, Candida, or Propionibacter acnes? Everybody chose Propionibacter acnes. Fantastic, that is correct.
In conclusion, the prostate is an immunocompetent, androgen-dependent organ of fertility, but the direct target for a number of both benign and malignant diseases. Impairment of the the epithelium status can decrease accumulation of zinc and citrate, and it can affect kallikrein secretion. Inflammation is associated with both BPH and prostate cancer, but the data cannot truly confirm causality. Thank you.
ABOUT THE AUTHOR
Ryan P. Terlecki, MD, FACS, is a reconstructive urologist for Atrium Health Wake Forest Baptist Medical Center, an academic Level 1 trauma center in Winston-Salem, North Carolina. Dr. Terlecki holds the rank of Professor and the title of Vice Chair of Research for the Department of Urology. In addition, Dr. Terlecki is Director of the Men’s Health Clinic, Director of Medical Student Education, and Fellowship Director for Reconstructive Urology. He holds a joint appointment in the Department of Obstetrics and Gynecology.
Dr. Terlecki earned his medical degree from Wayne State University School of Medicine and completed residency in general surgery and urology at Detroit Medical Center. Following his residency, Dr. Terlecki completed two separate fellowships in reconstructive surgery. He completed a fellowship at the University of Colorado’s Denver School of Medicine and at UT Southwestern Medical Center in Dallas, Texas.
Dr. Terlecki’s publications cover multiple areas of trauma and reconstruction and his research is focused primarily on models of wound healing and regeneration in the lower genitourinary system. Dr. Terlecki’s areas of expertise include urethral stricture disease, male sexual dysfunction, male incontinence, Peyronie’s disease, chronic testicular pain, hypogonadism, and infertility. He is a member of the Society of Genitourinary Reconstructive Surgeons (GURS), a member of the American Urological Association (AUA), and past president of the North Carolina Urological Association (NCUA).