Sam S. Chang, MD, MBA, presented “Robotic Cystectomy Versus Open Cystectomy—What do we Know?” at the 2nd Annual International Bladder Cancer Update on January 27, 2018 in Beaver Creek, Colorado
How to cite: Chang, Sam S. “Robotic Cystectomy Versus Open Cystectomy—What do we Know?” January 27, 2018. Accessed Nov 2025 . https://grandroundsinurology.com/Robotic-Cystectomy-Versus-Open-Cystectomy/
Summary:
Sam Chang, MD, MBA, delineates the benefits and shortcomings of both robotic and open cystectomy, specifically in terms of morbidity, compilation, and recurrence rates for patients, and the learning curve associated with each method for clinicians. He also discusses how the financial cost of robotic surgery factors into this comparison.
(Twitter Question) Reveal the Answer to Audience Response Question #1
Compared to an open cystectomy, robotic cystectomy and dissection results in fewer lymph nodes removed at time of PLND.
- True
- False
Reveal the Answer to Audience Response Question #2
The following statement is true in regards to robotic cystectomy versus open cystectomy:
- A. Robotic cystectomy results in longer hospital stay.
- B. Robotic cystectomy results in increased blood loss.
- C. Robotic cystectomy results in increased pain scores.
- D. Robotic cystectomy results in higher hospital costs.
- E. Robotic cystectomy results in increased transfusions.
Reveal the Answer to Audience Response Question #3
Learning curve estimates in regards to decreasing operative length of time with robot cystectomy requires at least how many cases?
- A. 5
- B. 20
- C. 100
- D. 200
Reveal the Answer to Audience Response Question #4
A 72-year old man is told that a robotic cystectomy results in improved cancer outcomes and decreased complications. Is this TRUE or FALSE?
- True
- False
Robotic Cystectomy Versus Open Cystectomy—What do we Know? – Transcript
Click on slide to expand
Radical Cystectomy
So I start off with radical cystectomy as a group. We know the morbidity and the possible mortality associated with the procedure is significant. It requires a learning curve, the surgical expertise that we know is out there, and it is a combination of not only having local control but also distant and long-term oncologic control is essential, and discouragingly within our residency programs the average number of cystectomies in diversion done are actually four by a graduating resident. That is the average number, now there area number of institutions that are way on one end, but there are institutions where a graduating resident will have one cystectomy diversion completed. And so you are talking about a very complicated procedure, one in which has significant morbidities and issues with this.
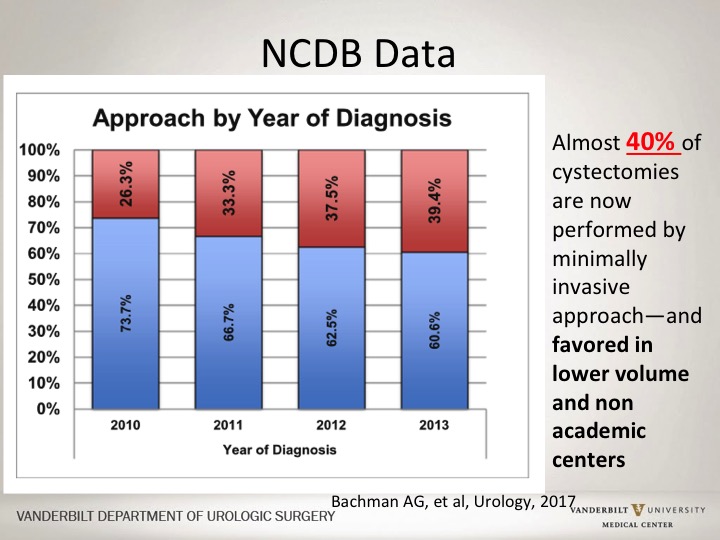
NCDB Data
So the question is is a robotic approach vis-à-vis a open approach, does it have any impact in terms of outcomes, in terms of things are being done? This is actually a recent slide looking at the National Cancer Database where almost 80% of cancer patients in the U.S. are actually captured, and if you look at actually over time the number of robotic cystectomies have increased dramatically so that almost 40% now of cystectomies are done with a robotic approach, and interestingly enough the robotic approach in this database which is academic, it’s private, a combination of all different types of centers, the majority of individuals who actually have lower number of cystectomies done and in centers that are non-academic, a higher percentage of those are being done actually via robotic approach.
Comparison Points
So, if you look at different types of comparison points between the two different types of approaches, these are the things that I think we should focus on.
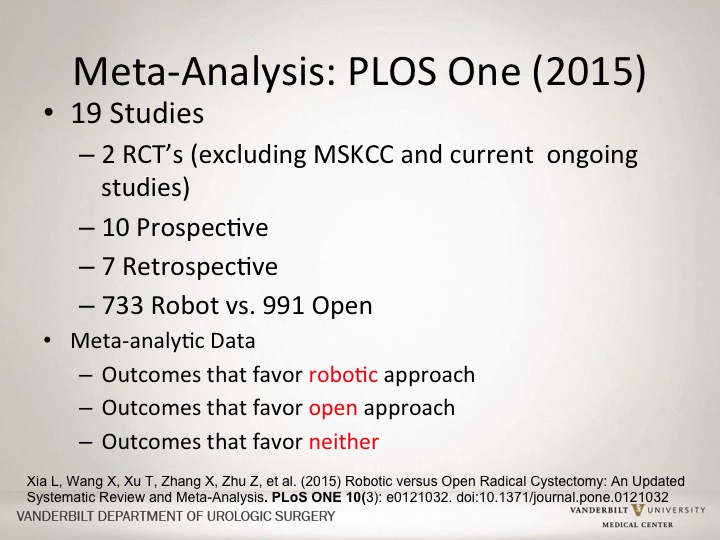
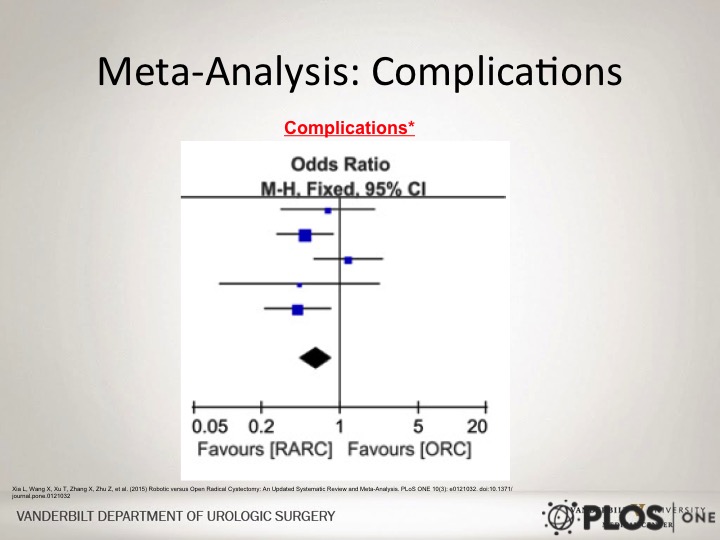
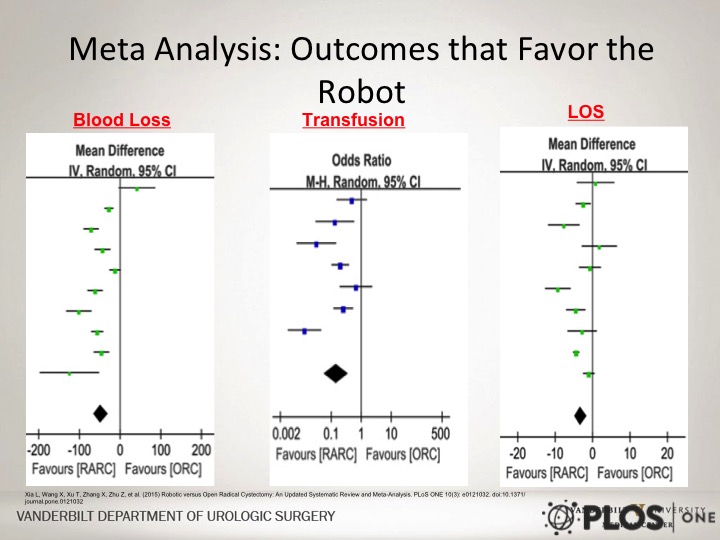
Meta-Analysis: PLOS One (2015)
A lot of this data comes from a large meta-analysis that was completed a couple of years ago looking at a combination of both randomized, controlled trials as well as prospective and retrospective studies looking at robotic approaches versus open approaches.
Morbidity/Complications
Let’s look at morbidity and complications specifically under that complications the mortality and readmission risk.
Radical Cystectomy
If you look at cystectomy historically, if you look at the complication rate, 30% to 60% mortality rate around 3% within the 30-day time period. At Vanderbilt, our complication rate all-comers is more than 40% within the 30-day time period. So, one that has significant complications associated with it.
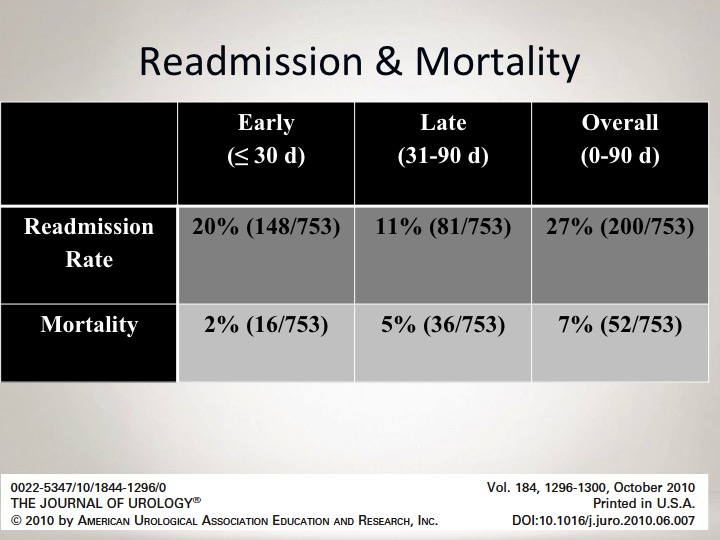
Readmission & Mortality
If you look at our readmission and our mortality rate, this is something that I tell our patients, that our 90-day mortality rate, 90-day mortality rate is 7% associated with this procedure, so in essence the combination of morbidity, both short-term 30 days as well as within 90 days is quite significant.
Meta Analysis: Complications
If you look at the complications in this meta analysis looking at robotic versus open, overall looking at all of these types of studies that were compared, there is actually a slight favor in terms of robotic versus open approach, in terms of overall complications.
Meta Analysis: Outcomes that Favor the Robot
But if you look at specific complications there are some things that are more clearly advantageous at least in this meta analysis for the robotic approach, and that would include less blood loss, fewer transfusions, and a slightly shorter length of stay. Now, importantly this can be significantly impacted by the use of ERAS protocols that Peter just discussed, and so in essence whether or not length of stay truly is caused by just this robotic approach is difficult to say. But I think the data regarding blood loss and transfusion loss is pretty clear.
NO Differences in Re-admissions
This is a recent study looking again actually within a specific large national US health insurer, and showed that it was actually no difference in re-admission rate between robotic versus an open approach. The majority of these were open. A smaller percentage were robotic. The length of stay was shorter for the robotic, but the key was there was no difference then in the 30-day readmission rate, and no difference in the length of stay if those patients were readmitted.
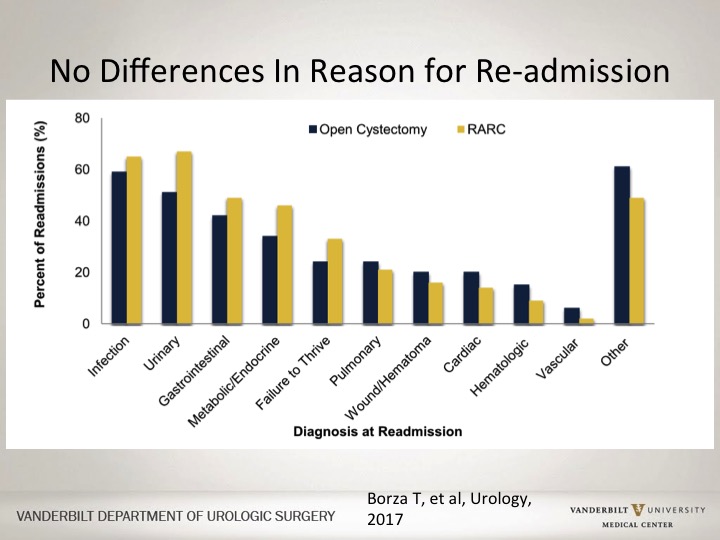
No Differences in Reason for Re-admission
If you look at the different causes for patients to be readmitted, there was no cause that was more likely to be associated with robotic versus open approach.
Re-admission Length of Stay the Same
And if you look at the length of stay so somebody came back in after a robotic operation or after an open operation, how long they stayed after the readmission was actually no difference between the arms at all.
BUT Cystectomy is Just a Portion of the Procedure
Importantly, when you look at a robotic cystectomy, that is just part of the procedure. The vast majority of these trials are talking about a robotic approach with the removal of the bladder, and then you make an incision to do the diversion. None of them have really focused on the combination of both intracorporeal reconstruction as well as removal of the bladder.
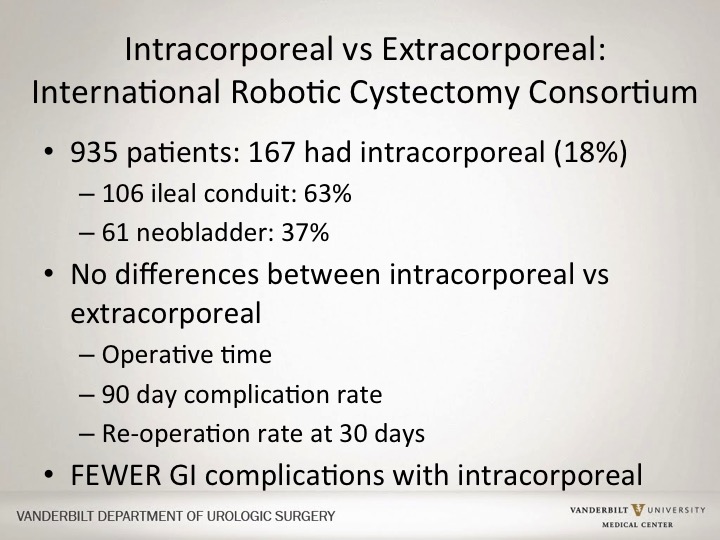
Intracorporeal vs. Extracorporeal
So this is the robotic cystectomy consortium. This is a large number of institutions that have gotten together to pool their data. They specifically looked at this whether or not an intracorporeal approach would be more likely to have complications associated with a robotic approach. The majority of these is you would imagine would be ileal conduit, but they actually showed there would be no difference when it came in terms of operative time, complication rate and reoperation rate, now you know, in truth the fact that their operative time was really no different I think is the most impressive finding of this, but they said that in fact the only difference they saw was fewer GI complications when there was an intracorporeal approach used.
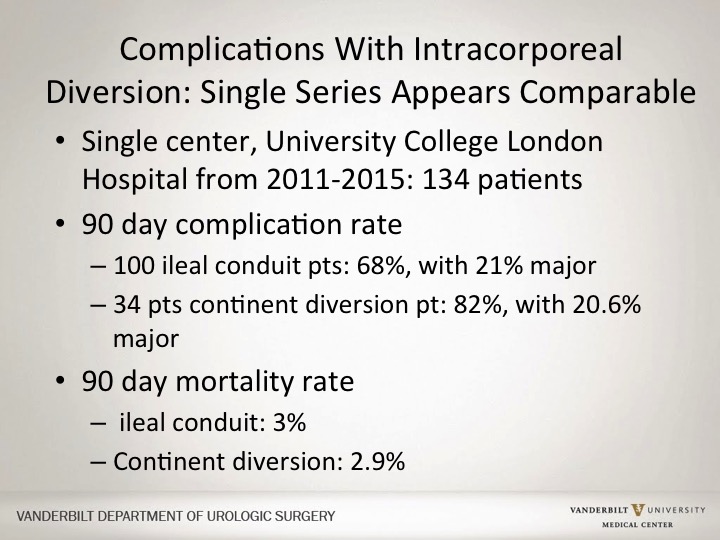
Complications With Intracorporeal Diversion: Single Series Appears Comparable
There was a single series, a small one looking at more recently whether or not there was a difference with intracorporeal rate versus their open rate. This was based out of England, and looking at their 90-day complication, their 90-day mortality rate different types of diversions, and they found overall that there was no difference again between that.
Learning Curve
We talked about complications. What about the learning curve? Transitioning from an open approach to any robotic approach I think is quite difficult, and I think that was much more telling, probably a decade ago. But right now there is really very little reporting, and not published anything at all regarding the transition learning specifically regarding cystectomy, and really now the question is is it easier now because of the prevalence of robotic prostatectomies. 90% of prostatectomies done are done robotically in the US. The vast majority of residency training programs, the number of open prostatectomies that are actually performed by the residence is probably average in the single digits.
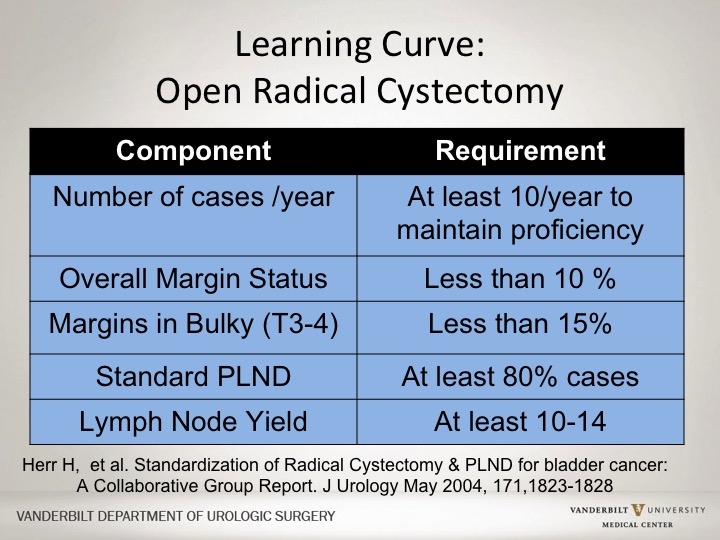
Learning Curve: Open Radical Cystectomy
If you look at the learning curve that was projected for open radical cystectomy, the thought was and these are guidelines for the SUO fellows was that you should probably do at least 10 a year, you should have a margin status less than 10% being positive, you should do at least a standard pelvic lymph node dissection and they should at least get 10 to 14 nodes. These are totally made up minimum criteria, but it is an attempt to standardize in some way what should be done for the open surgeon at the time of radical cystectomy.
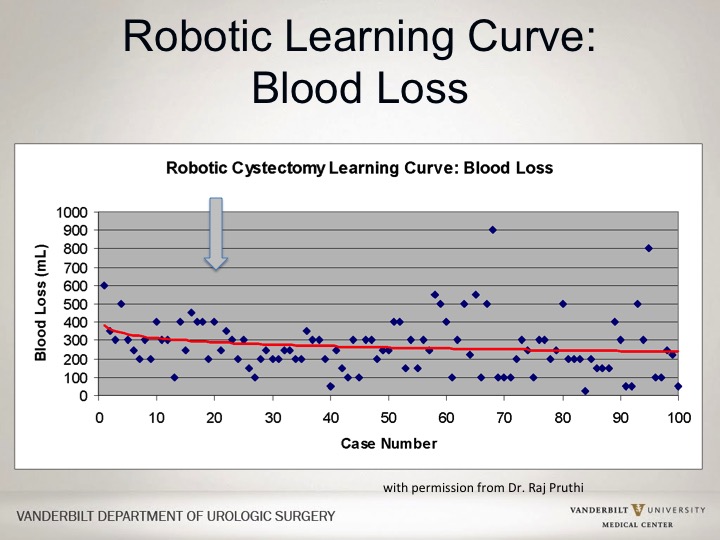
Robotic Learning Curve: Blood Loss
If you look at the robotic curve, there clearly is more experience gained over time, and these are slides actually I showed last year from Raj. They still haven’t published this yet regarding the overall change in inflection point, so after a number of cases you get actually a flat line in terms of blood loss. So with blood loss after 20 or so of these robotic cystectomies you didn’t have less blood loss as a whole.
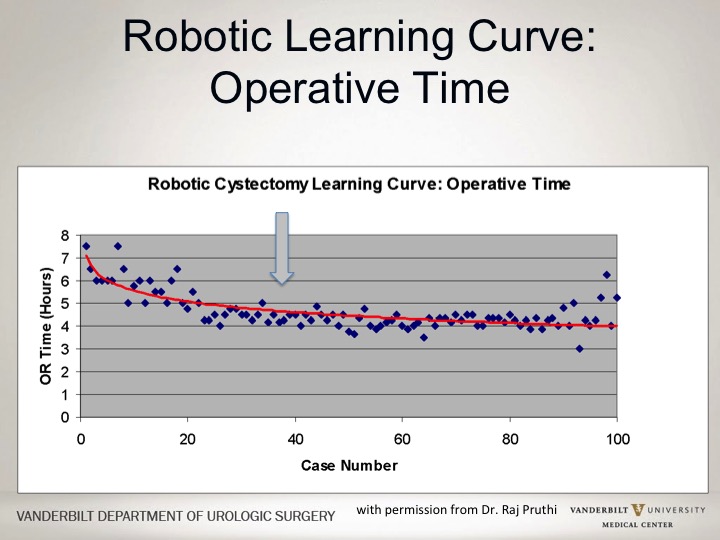
Robotic Learning Curve: Operative Time
In terms of operative time, it took a little bit longer to get more speedy on the robot, about 40 cases after that actually your learning curve flattened out.
Robotic Learning Curve; LN Count
If you looked at a lymph node count, similarly about 20 or so once you did 20, your number of lymph nodes didn’t necessarily increase or you didn’t do a more complete lymph node dissection so clearly earlier on in the procedure you experience a curve the less likely you are to do a complete dissection, the longer it will take you the more likely to have more blood loss.
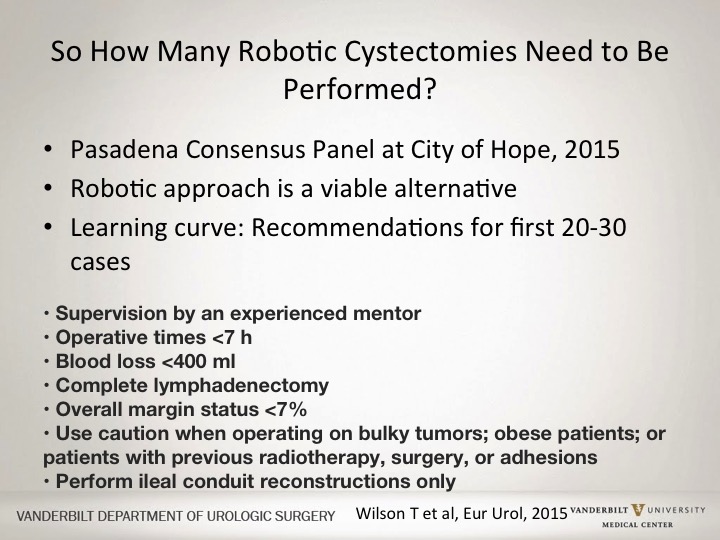
So How Many Robotic Cystectomies Need to Be Performed?
So how many robotic cystectomies really then need to be performed? This was a consensus panel a couple years ago of robotic surgeons, self-proclaimed experts who basically say that you should do at least 20 to 30 before you actually have some level of competence, and they define actually the experience of a surgeon, the very experienced surgeon as someone who has done more than 100 of these cystectomies and can then tackle these procedures that are more difficult, have an average blood loss less than 300cc, able to do a complete lymphadenectomy as well as different types of diversions with an aim of length of stay of 5 to 10 days. Again, self-proclaimed experts who basically say this is what you should be able to achieve, once you get to more than 100 robotic removals.
Financial Costs
What about cost? If you look at the cost of a robotic procedure versus an open procedure, as a whole there is no debate the robotic approach is going to be more expensive. To add up costs, you have the fixed cost of the robot itself, and then you have the variable cost that really make a difference, the length of time within the operating room, importantly the OR personnel used, as well as disposable equipment that are required for the robotic approach as opposed to the open approach, and then you add on how long the patient stayed. So it’s a combination of both intraoperative variables as well as post-operative in-hospital stay.
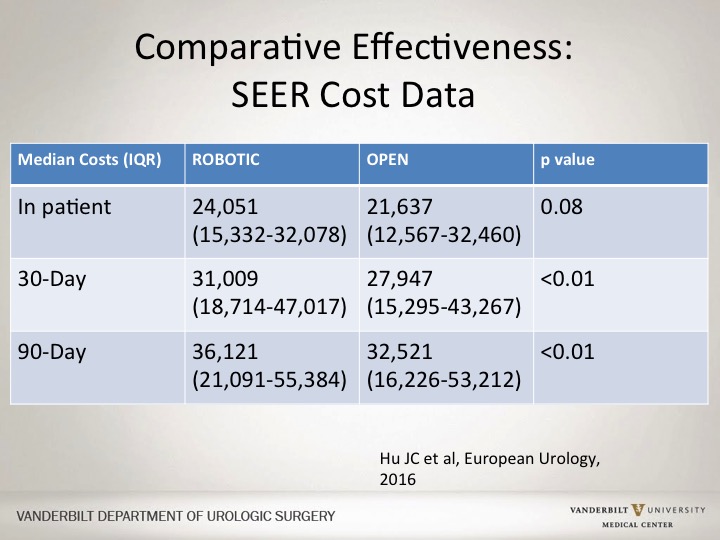
Comparative Effectiveness SEER Cost Data
So if you look at SEER data, and there are other institutional trials looking at MSK data, the robotic consortium data have all basically stated that the OR time is a little bit longer and as a result the costs are actually a little bit higher. SEER data would have actually showed that similarly that overall for a robotic approach it tends to be more expensive. But actually, as you go out over time, there doesn’t seem to be as much a difference, but there continues to be a difference.
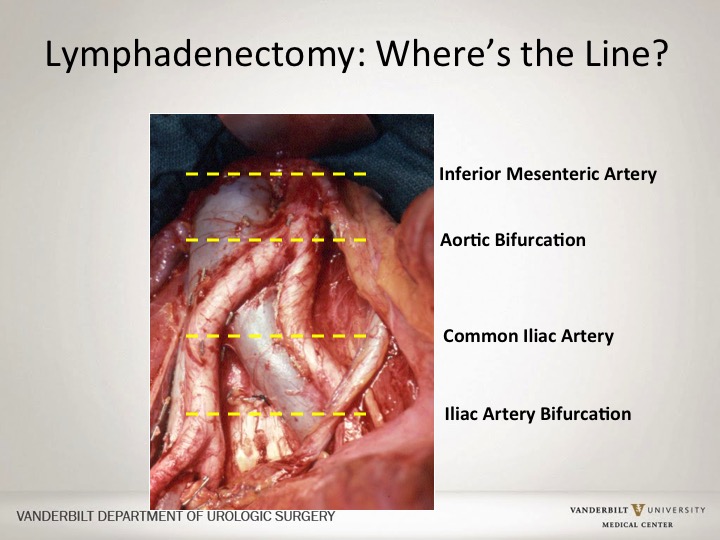
Lymphadenectomy: Where’s the line?
Within oncologic issues I think you have to determine lymphadenectomy is it important to go here by the bifurcation, is it the common iliac artery, aortic bifurcation, all different levels of an extended lymph node dissection. I think those folks that have seen surgeons that do a robotic approach they are able to think adequately do a lymph node dissection and actually the folks at MD Anderson looked at lymph node dissection and going back in after robotic dissection was done by an open surgeon. And the adequacy of the lymph node dissection I think is quite good up to the level of probably the common iliac artery. The dissection any higher is a little bit more difficult, nor has it been studied well.
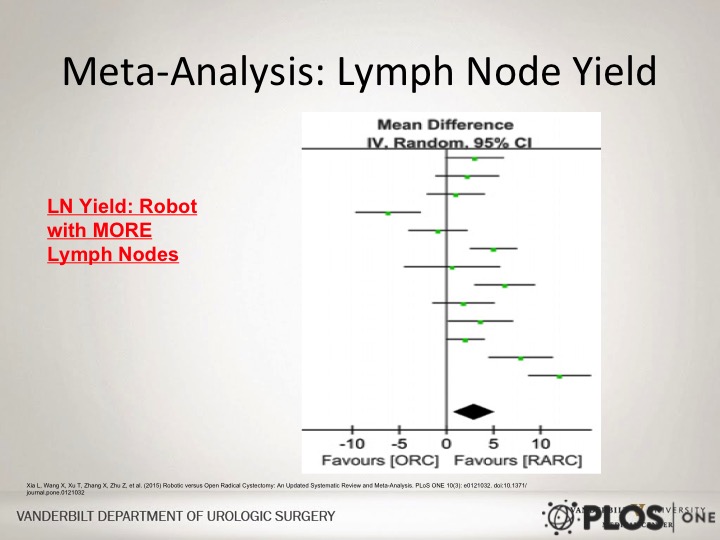
Meta-Analysis: Lymph Node Yield
If you look at the meta-analysis regarding lymph node yield, the lymph node yield says that there is a slightly higher lymph node count with the robotic approach. In all honesty, I think the dissection in terms of the anatomic detail in the template you are able to achieve that robotically versus open whether or not the lymph node count is higher or less I think really doesn’t make much difference.
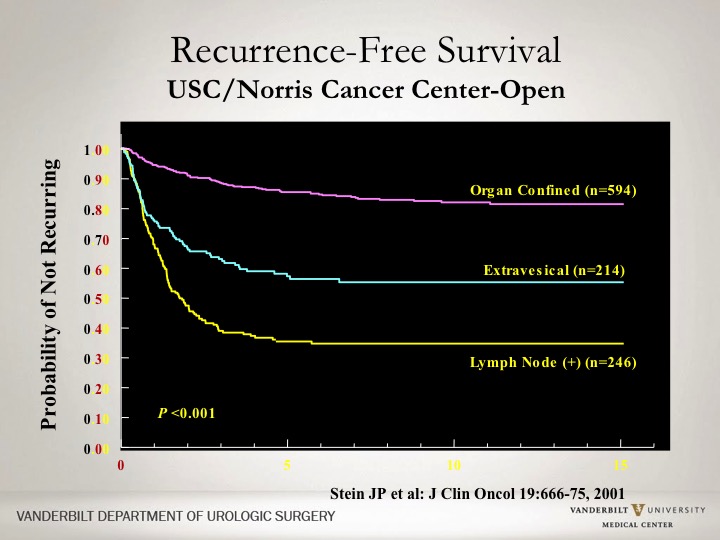
Recurrence-Free Survival
So under oncology, you have the adequacy of the lymph node dissection. I mean the nitty gritty is what about outcomes, what about cancer survival? This is a curve that people have seen quite a bit regarding the USC series and historically how patients have done depending upon if they had organ confined disease, disease that was extravesical or more extensive disease with lymph node involvement. So this curve basically shows you probability of not recurring or cancer free survival for a significant long period of time.
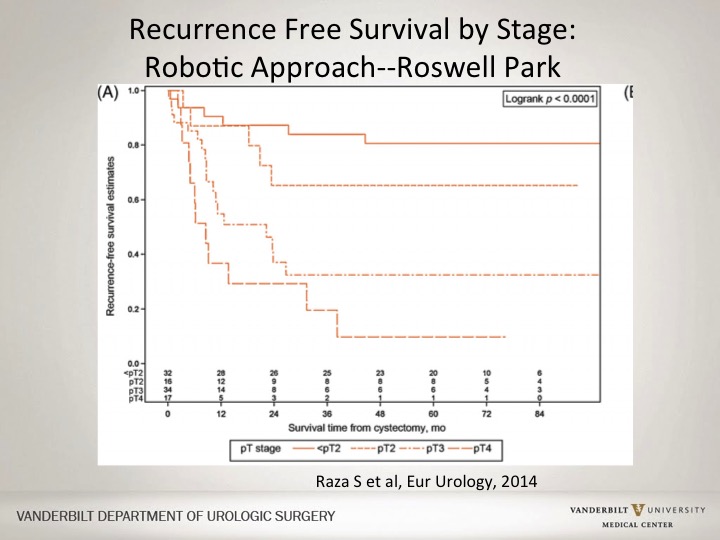
Recurrence Free Survival by Stage: Robotic Approach—Roswell Park
The robotic curves are not too dissimilar. This is a single institution series, very similar to the US series but with much smaller numbers. This is from Roswell Park showing a very similar curve in terms of outcomes at the five-year mark. These are not ten-year marks, not 15-year marks, but show similar outcomes for organ-confined versus extravesical disease and for PT4 disease.
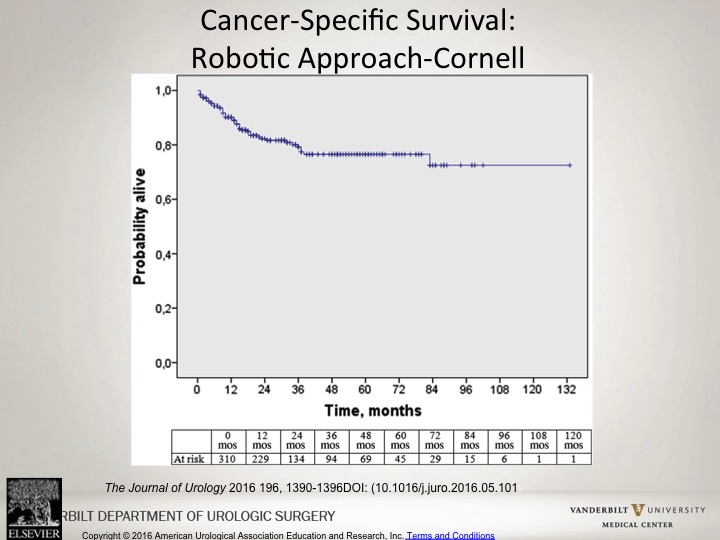
Cancer-Specific Survival: Robotic Approach—Cornell
Similarly if you look at the robotic approach at Cornell, you would see a similar overall probability alive in terms of cancer free rates with those patients that undergo robotic approach.
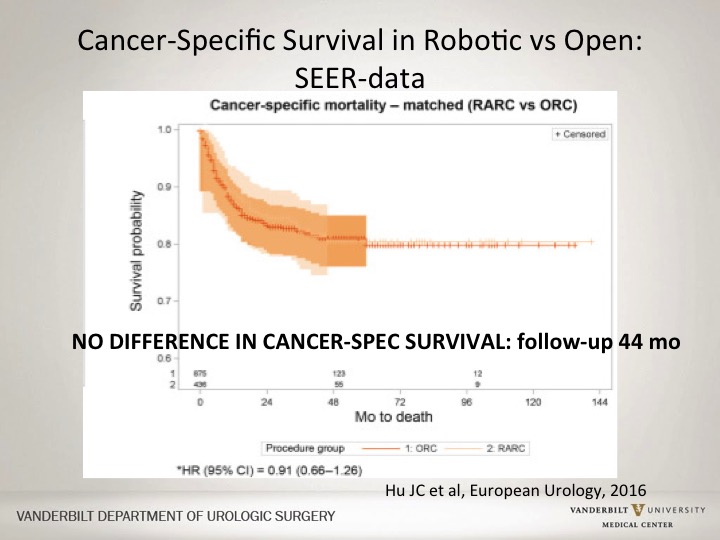
Cancer-Specific Survival in Robotics vs. Open: SEER-data
If you look at SEER data, again real world data with both the advantages and disadvantages of SEER data, but in terms of looking at overall robotic versus an open approach, there was actually no differences in cancer-specific survival at a follow-up of about four years. So at this point this is not head-to-head prospective data but looking at single institution as well as large institutional databases there seems to be no significant difference.
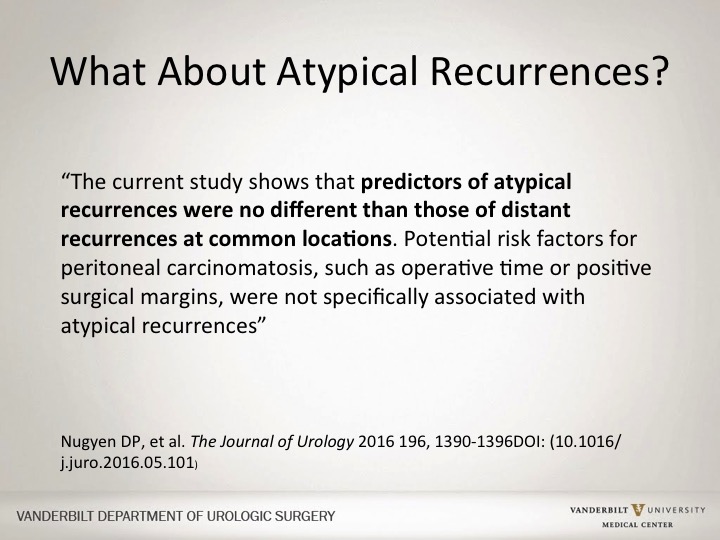
What about atypical recurrences?
I think there was a valid concern and still in the back of my mind there is still concern about atypical recurrences, recurrences with a robotic approach or a laparoscopic approach wherein which there are occurrences at locations that you normally do not see with an open approach. The folks at first actually considered this, people in Europe mentioned this as well as the people at Cornell. They were the ones who actually first published the possibility of about up to 10% of these atypical recurrences. They went back and actually looked at their data regarding who actually recurred, what sites, the location of disease, and they actually found that there was no specific predisposition for those patients that underwent a robotic approach versus an open approach, and that there were no differences in these uncommon locations. Everybody also has their anecdotal cases where there was tumor spillage, where there were issues or concerns, there is something here that probably shouldn’t have occurred is it published? No. Do I think there are more atypical recurrences, I think definitely possibly if the surgery just like any open surgery isn’t done carefully.
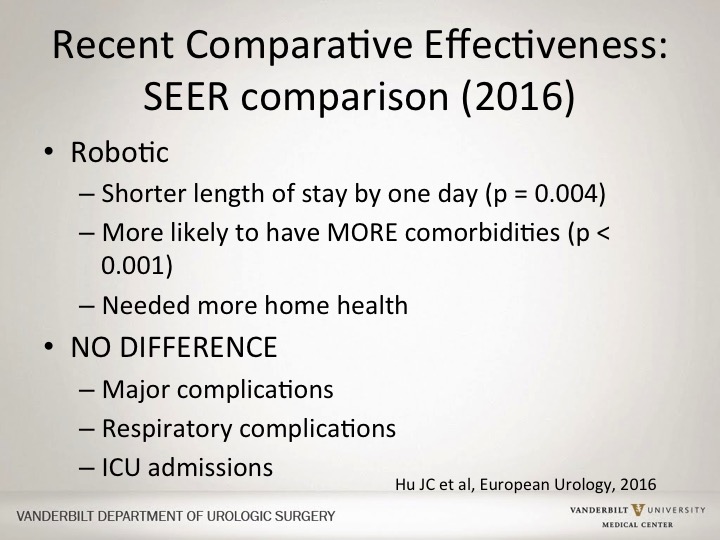
Recent Comparative Effectiveness SEER Comparison (2016)
Then overall in terms of comparative effectiveness data, from the same SEER evaluation overall the robotic approach tended to have patients had a shorter length of stay. They were more likely actually to be sicker, have more comorbidities and they needed more and longer home health evaluations and treatments afterwards, probably more likely due to their initial comorbidities as opposed to the approach, and there was no difference in major complications, respiratory complications or ICU admissions.
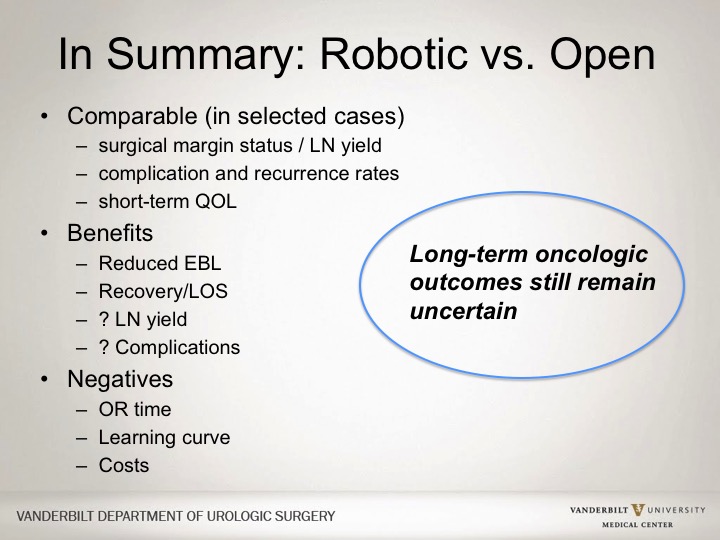
In Summary: Robotic vs. Open
In summary, I think the benefits of the robotic approach, less blood loss, perhaps an impact on length of stay. I think really no difference in terms of lymph node yield or complications in some ways equivalent. I don’t think necessarily superior and clearly I don’t think worse. The negatives clearly are the OR time, the learning curve, and the cost, I think the OR time does improve with time. I think the cost improves with better efficiency. The learning curve is similar to the learning curve with any procedure. The learning curve with an open cystectomy also requires time. The learning curve with a robotic approach also takes time. But I think the evolution of how we do things now robotically has made that learning curve easier.
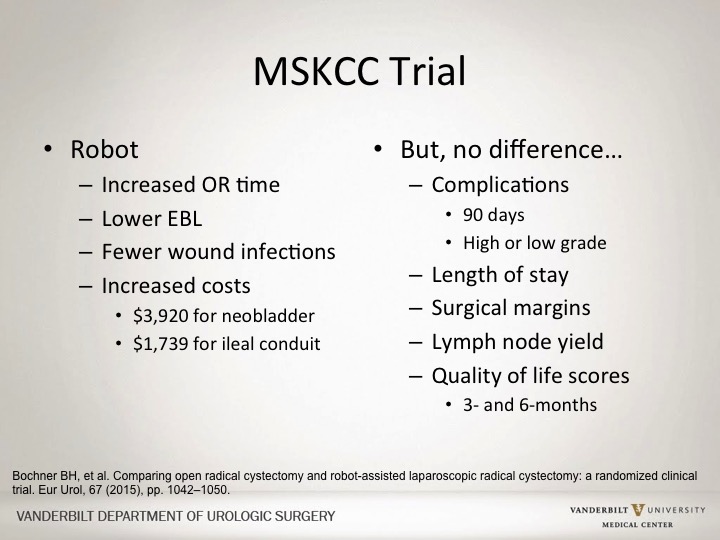
MSKCC Trial
The MSKCC trial is a single institution trial, randomized. The primary endpoint was actually looking at complications and what they found was the robotic approach had a longer time, less blood loss, but no difference in complications, no difference in length of stay, no difference in surgical margins, and no difference in quality of life. And so their conclusion was that there was no significant advantage of robotic approach.
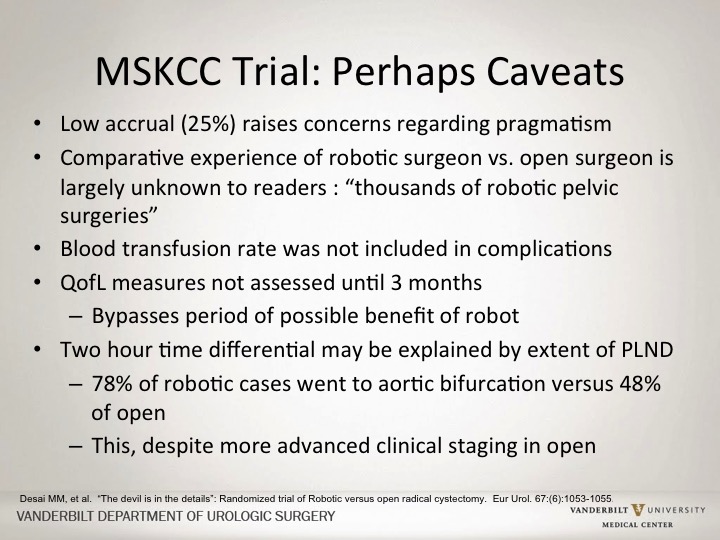
MSKCC Trial: Perhaps Caveats
There are some concerns with this trial. Caveats being in terms of the low overall enrollment within these patients. The idea of comparing open surgery done for decades and decades at Memorial with a single surgeon who had never done a robotic cystectomy prior to this trial blood transfusions were not included as a complication just the blood loss was monitored, and the actual number of blood transfusions were significantly less in the robotic arm. And the idea of the differential in the time of the case may be associated with the extent of the lymph node dissection.
RAZOR Trial
The RAZOR trial, I think the RAZOR trial is kind of the elephant in the room. The Razor Trial is a large multi-institution trial funded by the government looking specifically at a combination of complications and outcomes. The primary outcome was basically equivalence in terms of primary outcomes in terms of cancer control. It’s a non-inferior design, and it was presented at the AUA this spring. It has not been published. And the findings this spring was the fact that there was a significant higher positive surgical margin rate with the robotic arm compared to the open arm. All of the other outcome factors actually were not different. I can tell you now and so I’m not going to show a slide, there was a re-evaluation of the data by the authors and it is currently in submission at a Journal with reviews and revisions, so I can’t tell you the final outcome in terms of the oncologic outcomes, but I’m still not sure what the final outcome of that trial is going to be until it’s published, but importantly I think that will be very important in terms of the robotic approach versus the open approach.
So What Approach Do I use for Radical Cystectomy?
So what approach do I use? I do both. And I think the ongoing studies will be essential. If you ask me how many cystectomies did I do open versus robotic, probably 75% of cases now I do robotically as opposed to open for many different reasons, but all of my urinary diversions are still done with an extracorporeal approach. I’ve only done probably 10 intracorporeal approaches. So I’ll stop there. Happy to take questions, and then, Mike, I don’t know if you want to do a few minutes of the panel or what you want to do but I’m happy to take any questions.
ABOUT THE AUTHOR
Sam S. Chang, MD, MBA, is the Patricia and Rodes Hart Endowed Professor of Urologic Surgery and Oncology and the Chief Surgical Officer of the Vanderbilt Ingram Cancer Center in Nashville, Tennessee. Dr. Chang is a graduate of Princeton University and Vanderbilt University Medical School. He completed his uro-oncology fellowship at Memorial Sloan-Kettering Cancer Center and obtained his MBA at Vanderbilt’s Owen School of Business.
Since his return to Nashville, Dr. Chang has focused on urologic oncology and education and has led efforts in integration of evidence-based medicine in clinical pathways, enhanced national guidelines formulation, and improved urologic cancer staging. He has orchestrated the initiation and expansion of multiple cancer-related treatment protocols at Vanderbilt and elsewhere. Dr. Chang has served as Chair of the Society of Urologic Oncology (SUO) Panel on Hormone Refractory Prostate Cancer, Chair of the American Joint Committee on Cancer (AJCC) GU Staging Task Force, the facilitator and Vice-Chair of the Renal Malignancy Follow-Up AUA Guidelines Panel, the chair of the AUA/ASCO/ASTRO/SUO Guidelines on Nonmetastatic Invasive Bladder Cancer, and Chair of the AUA Prostate Cancer Core Curriculum Committee. He completed his term (2018-2022) as Assistant Secretary of the American Urological Association in charge of International Relations with Europe and the Middle East and served as a member of the initial AUA Task Force on Diversity and Inclusion.
Dr. Chang was a member of the AUA Renal Mass Guidelines as well as the AUA Upper Tract Cancer Guidelines and is a current member of the National Comprehensive Cancer Network (NCCN) Bladder Cancer Panel. His current leadership roles include Secretary of the SUO (2022-2026), Chair of the American Board of Urology Examination Committee (2020-2024), and Trustee for the American Board of Urology (2024-2030).
While maintaining a busy clinical surgical practice, Dr. Chang has authored more than 300 original publications and multiple book chapters. He has also edited several textbooks. For his academic efforts, he received the SUO’s first-ever Distinguished Service Award, aCaPCURE Young Investigator Award, and has been named multiple times as a Journal of Urology’s Best Reviewer. Dr. Chang was named as the 2011 recipient of the American Urologic Association Gold Cystoscope Award and was nominated as Fellow of the Nashville Health Care Council in 2016. His education and mentorship efforts have been recognized with his Department's Best Teaching Faculty Award as well as the Christine Manthos Mentoring Award from the Society of Women in Urology (SWIU).