Mitchell R. Humphreys, MD, presented “Updates in LUTS: Treating Overactive Bladder and Nocturia” during the 28th Annual Perspectives in Urology: Point Counterpoint on November 14, 2019 in Scottsdale, Arizona.
How to cite: Humphreys, Mitchell R. “Treating BPH: Comparing HoLEP, Rezūm, UroLift, and Aquablation” November 14, 2019. Accessed Jun 2025. https://grandroundsinurology.com/treating-bph-comparing-holep-rezum-urolift-and-aquablation/
Treating BPH: Comparing HoLEP, Rezūm, UroLift, and Aquablation – Summary:
Mitchell R. Humphreys, MD, reviews the current society recommendations addressing when to intervene with surgical management in patients with lower urinary tract symptoms (LUTS) secondary to benign prostatic hyperplasia (BPH). He provides an overview of new minimally-invasive surgical therapy technologies for these patients.
Abstract:
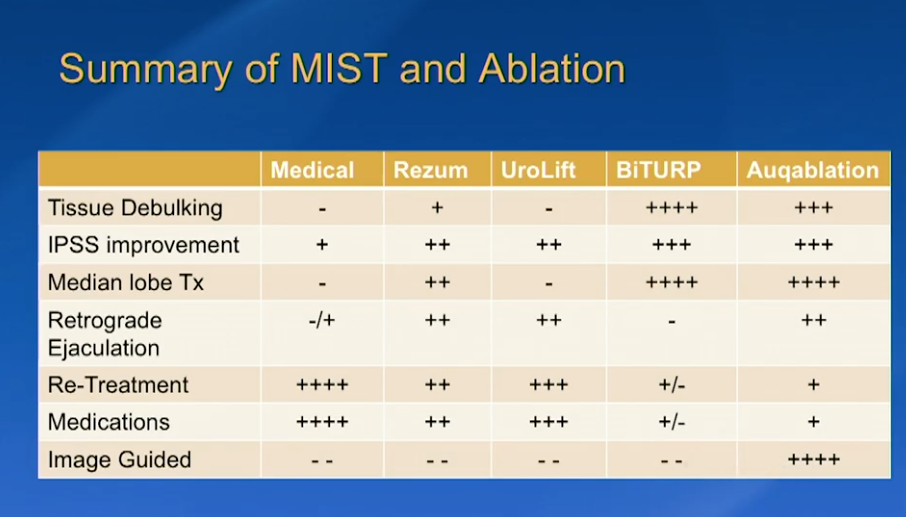
While medical therapy remains the most prevalent treatment for lower urinary tract symptoms (LUTS) attributed to benign prostatic hyperplasia (BPH), there are indications for surgical intervention, including renal insufficiency, refractory urinary retention, recurrent urinary tract infections, bladder stones, and gross hematuria. Minimally-invasive surgery therapies (MIST) play a large role in treating individuals who have smaller prostates, cannot tolerate anesthesia, or are concerned with preserving antegrade ejaculation.
There is a host of new MIST technologies that may provide better options for these patients. Firstly, prostatic urethral lift (UroLift) showed a rapid and durable improvement in LUTS and quality of life (QOL) in 5-year results from a randomized study. However, a significant number of these patients had surgical retreatment or were taking medications at 5 years.
Comparatively, 4-year results of a randomized controlled study of water vapor thermal therapy (Rezūm) showed durable symptom relief and QOL improvement, but also a lower rate of patients having surgical retreatment or going on medical therapy.
Aquablation is a next-generation surgical therapy that involves an image-guided, robotically-controlled, high-velocity water jet that provides precise and rapid removal of tissue. Results from a trial comparing aquablation to transurethral resection of the prostate (TURP) favored aquablation in terms of maximum urinary flow rate, anejaculation rate, and mean resection time. This technique demonstrated feasibility, safety, and a relatively short mean operating time when treating large prostates as well.
While holmium laser enucleation of the prostate (HoLEP) has historically raised concerns regarding incontinence, large series data of this procedure has shown a long-term stress and urge incontinence rate of 1.4%. Prospective data also supports the feasibility and safety of HoLEP as a day-case procedure. Furthermore, when compared to robotic-assisted simple prostatectomy (RSP), HoLEP overall resulted in better perioperative outcomes.
About Perspectives in Urology: Point Counterpoint
Perspectives in Urology: Point Counterpoint (PCP) is an annual, multi-day, CME-accredited conference devoted to discussing and debating the latest topics in men’s health and general urology, as well as management of bladder, renal, and both localized and advanced prostate cancer. More than didactic lectures, the conference’s format includes debates, point-counterpoint discussion panels, and unique case-based presentations. Dr. Humphreys presented this lecture during the 28th PCP in 2019. Please visit this page in order to register for future PCP meetings.
ABOUT THE AUTHOR
Mitchell Humphreys, MD, is a Professor and Chair of the Department of Urology at the Mayo Clinic in Scottsdale, Arizona. He holds dual appointments in the Department of Urology in the Mayo College of Medicine and in Clinical and Translational Sciences in the Mayo Graduate School. In addition, he serves as the Dean of the Mayo Clinic School of Continuous Professional Development and as the Endourology Fellowship Director. Dr. Humphreys completed his residency at the Mayo Clinic in Rochester and an Endourology and Stone Disease Fellowship at Indiana University. Since that time, he has been on staff at the Mayo Clinic in Arizona. His clinical focus is on surgical and metabolic stone disease, BPH (with a special focus on HoLEP), and minimally invasive GU oncology. In addition to the publication of over 100 peer-reviewed manuscripts and multiple book chapters, he is a journal editor and reviewer for several international urology journals. He is an active member of the Endourology Disease Group for Excellence (EDGE) research consortium. Outside of his work with the Mayo Clinic, he serves on the Board of Directors of GSD Healthcare, LLC, promoting basic healthcare initiatives in underserved and impoverished areas around the globe. He also serves as a member of the Columbia College Board of Trustees.