Philip J. Koo, MD, presented “Update on Radiopharmaceuticals— Choosing a Companion Drug to Radium-223” at the International Prostate Cancer Update on January 27, 2018 in Beaver Creek, Colorado
How to cite: Koo, Philip J. “Update on Radiopharmaceuticals— Choosing a Companion Drug to Radium-223” January 27, 2018. Accessed [date today]. https://grandroundsinurology.com/Choosing-a-Companion-Drug-to-Radium-223/
Summary:
Philip J. Koo, MD, describes the mechanism of action of radium-223 in prostate cancer treatment, options for combining and layering radium-223 with other drugs, and how the field of radiation is evolving. He also addresses the controversial ERA 223 trial results.
(Twitter Question) Reveal the Answer to Audience Response Question #1
Prospective clinical trial data has proven radium 223 to be safe and effective in combination with:
- A. Abiraterone
- B. Enzalutamide
- C. Sipuleucel-T
- D. Docetaxel
- E. None of the above
Update on Radiopharmaceuticals— Choosing a Companion Drug to Radium-223 – Transcript
Click on slide to expand
Radium 223 is best used in combination with:
And then, additional disclosure is- I’m a simple-minded nuclear radiologist, but I’m not going to be speaking about imaging. And Dr. Reiter’s talk was awesome, so I don’t think there’s any need to talk about imaging.
Good to Great
Oh, so when I was first invited to give this talk, and I was given this topic, you know, in my mind I was thinking about Radium-223 and I was thinking about all of the experience I had giving Radium-223, and then using the available data to sort of come up with a story that made sense. That being said, things changed on November 30th, when there was an announcement, and we’ll go into those details later. But it sort of reminded me of this book, Good to Great, written in 2001. It was published in 2001.
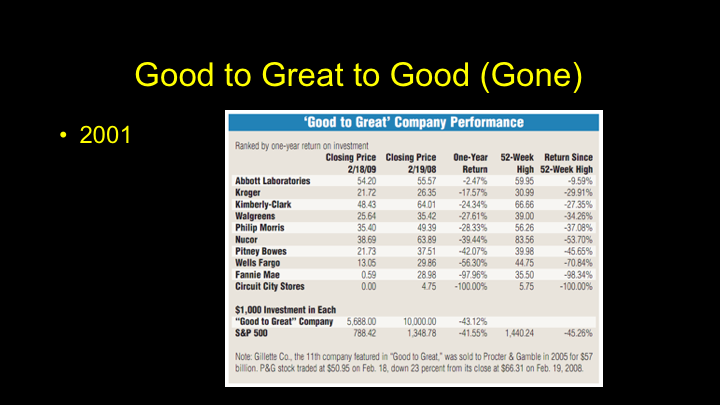
Good to Great to Good (Gone)
And then, if you look at the various companies that were actually talked about in the book, it is interesting to see how they performed, so it’s good to great to good, or maybe even gone. Circuit City, wow, if you invested in that company based on that book you’d be broke. Fannie Mae was D-listed from the NYCE. Wells Fargo had their own set of issues with fraud, and these companies during the economic recession, actually underperformed the S&P 500 during that time. So, it was kind of an eye-opening lesson that you have to change.
How the Mighty Fall
And Jim Collins being the thought leader that he is wrote a book How the Mighty Fall and I think it’s kind of ingenious that he would follow up with that.
Change
I think we all know that change is going to happen. Change is real, and I think one of the great things about this meeting is that we really embrace change and a lot of discussion about change occurs. I was talking to Jim – – at dinner last night, and he actually made this comment. Coming to this meeting helps him stay three years ahead in his practice, which I think is pretty remarkable. LUGPA now a partner in this meeting clearly is a change meeting, and they’ve talked about various things. They’ve made a huge difference, and now with the APMs I think that urology is in really good hands. Something magical won’t happen if we don’t do anything. We actually do need to act.
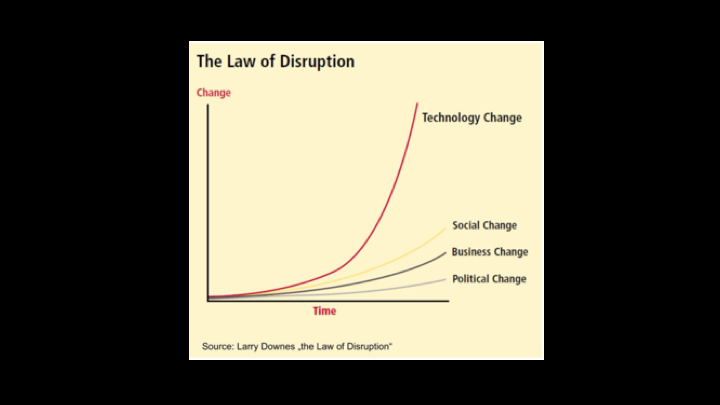
The Law of Disruption
When we think about change, I think clearly technology changes much faster than anything else, and then I think social change occurs, next business change, and political change. When we think about change in medicine, I think it actually lags much lower than anything else, which is a concern.
Target on our Backs
Which is a concern, because I think we have a target on our backs. And disruption is real, and if I think about radiology, my field, when I went into radiology everyone told me, oh, why are you going into radiology. Teleradiology, all of your cases are going to be outsourced, and that might have been true, but I think our society embraced the technology and really made it work to our advantage, and artificial intelligence, machine learning, that is real, but we’re taking very active steps to embrace it and use it in ways to actually improve patient care and reduce cost, and I think if we all—urology the same thing, advanced prostate cancer clinics, and the changes that are undergoing in urology have really helped us and create a roadmap for the ways that we can change from our societies perspective.
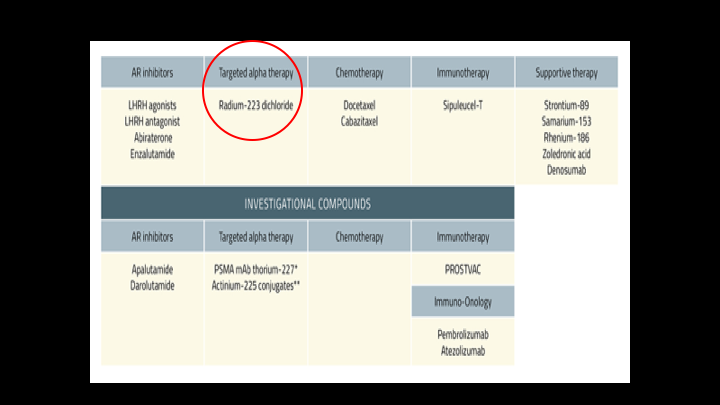
Targeted Alpha Therapy
That being said, we’re going to talk about targeted alpha therapies and Radium-223, and this sort of lists out some of the other drugs in that CRPC space.
Back to the Future
This is really going back to the future, because these systemic unsealed sources of radiation that we’re injecting were actually used in the past, but we’re re-visiting them, and I think there is a lot of potential for these in the future.
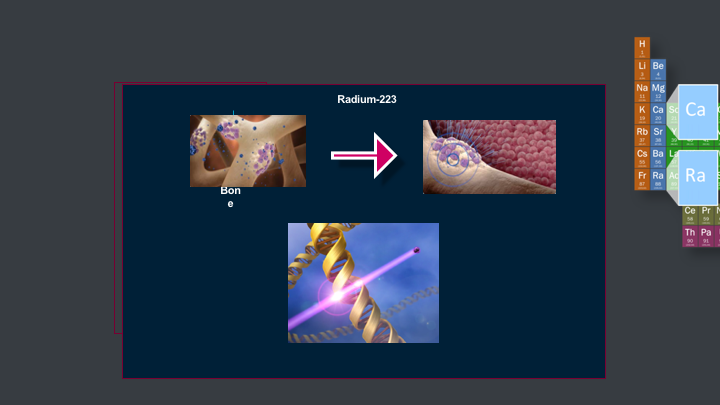
Radium-223
You inject it intravenously slow over one minute. It circulates throughout the body, and then it is going to localize to bone. It’s going to localize to areas that have metastatic disease to a higher degree because there’s greater perfusion to those areas, and the surface area of bone in those areas area actually going to be greater. Once it localizes to those lesions in bone, it’s actually going to give off this alpha particle, and create these double-stranded DNA breaks, and there’s actually small animal models that talk about Radium-223 causing changes in the tumor microenvironment that make it less hospitable to mets for the future.
Alpha Range – Beta Range
This is sort of the real key to how these alpha particles work. The alpha particle, you notice that the particle mass is multiple, multiple times greater than beta emitters, which is what we use in a lot of other therapy. So it is like getting hit by Mike Tyson as opposed to Floyd Mayweather, which by the way Floyd Mayweather he is a great boxer, but clearly he doesn’t have a lot of power. It’s range in tissue is much shorter, so that is significant because the radium is going to stay localized to the areas that it lands as opposed to beta particles which are going to go much further and affect healthy marrow cells, which is something that you don’t want to do.
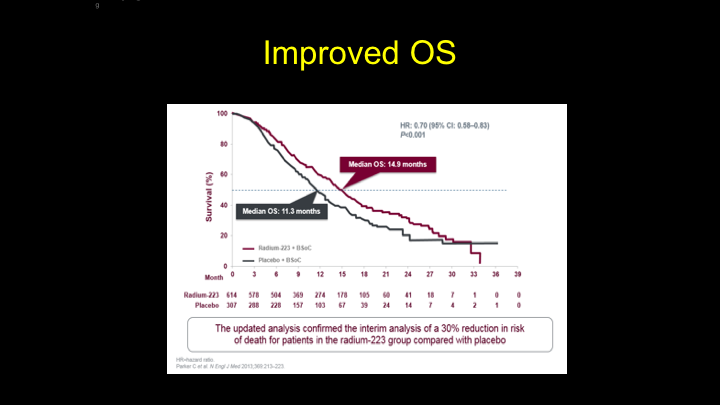
Improved OS
That is why we saw this improvement in overall survival from the ALSYMPCA Trial that—but we also saw an increase in time to your symptomatic first symptomatic skeletal event, so there was sort of this bone protective aspect to Radium-223 as well.
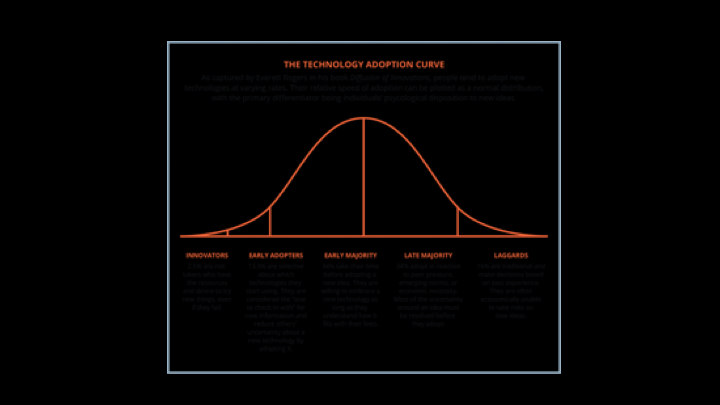
The Technology Adoption Curve
So I think it was approved four or five years ago, and we’re seeing more and more adoption of this.
How do we adopt change?
We’re seeing greater acceptance and greater ownership of this, and it was interesting to hear Dr. Crawford at the first talk, where he talked that there were actually 54 clinical trials actively using Radium-223 on clinicaltrials.gov, so I think that is a sign that we are really trying to dig deeper into how we use this.
Why?
I think the search for a combination therapy or a therapy that you use together really makes sense for Radium-223 because of the mechanism of action. It localizes the bone, and it is really disease agnostic. It just gives off an alpha particle wherever it can, and causes DNA breaks if there are cells there. So it is bone targeted. A problem with Radium-223 is that PSA rise, right, so you do see a slow rise in PSA, and we know that is probably coming maybe from other cells like other tissues, like soft tissues, nodal disease, and what not, so it makes sense to find something with a different mechanism of action where you can target various sites of disease. I think the other reason why it makes sense is because the drug has been proven to be safe in the ALSYMPCA trial.
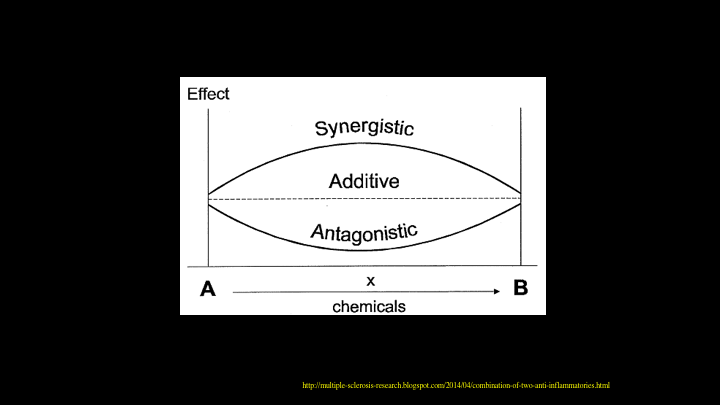
Effect
So, when we look for some sort of combination therapy, I think ideally you find something that is synergistic. And this comes from a multiple sclerosis website. If it’s additive, that’s not bad either. In this case, if you have something that is hitting the bone and something that is hitting the soft tissues, and they are additive, that works as well. Clearly, you don’t want something that is antagonistic, in which case, you wouldn’t move forward with such a therapy.
Radium-223 Plus Targeted Therapy
So we’ll start off with Radium-223 plus Targeted Therapy, and this morning, hearing Dr. Glode’s talk on PARP inhibitors was great for me, because it really opened up my understanding of PARP inhibitors.
PARP Inhibitor Plus Radium 233
And there are currently a couple of Phase 1B and Phase 1 and 2 trials looking at PARP inhibitors, and this makes sense. You know, if you have Radium-223, these alpha particles that can cause double-stranded DNA breaks, there are going to be times when it only causes single-stranded DNA breaks, and in those cases, if you have the combination with a PARP, it makes sense that you will lead to more cell death.
NMC
So, we will await the results from that. So, that led me to think, all right, imaging. I think a lot of times, we don’t really use imaging to assess response, especially in prostate cancer, but this is something that we did for targeted therapies, BRAF, MEK inhibitors in melanoma where we actually had baseline scans, follow-up scans, and we actually looked at response and correlated that with overall survival. So, I think the further we go along with these targeted therapies and combination therapies in prostate cancer, I would encourage some of the scientific people in this audience to think about ways that we could incorporate some of these newer imaging technologies into our protocols.
Radium 223 plus Immunotherapy
So radium 223 plus immunotherapy. Dr. Concepcion gave a great talk in immunotherapies, and I’ll be honest.
The Abscopal Effect
This whole experience has been very humbling. Medicine has been very humbling, and I remember when I first heard about the abscopal effect, I laughed. I thought that is impossible. That makes no sense at all, and I just sort of really dismissed it. Shame on me. We started seeing cases like this, and this case comes from the literature, where you had a liver lesion that was treated with external beam radiation, and that liver lesion was gone on a follow-up PET CT. Interestingly, a lesion in the left lower lobe of the lung disappeared even though it wasn’t radiated, and this lesion in the left sacrum also disappeared, and that is sort of the idea of the Abscopal effect. It’s a little different, because the abscopal effect was really meant for targeted therapy to a single lesion that releases antigens, and Radium 223 is a little different, because it’s systemic.
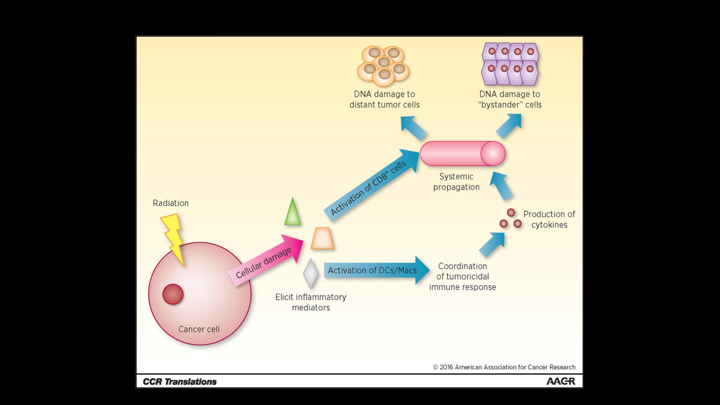
CCR Translation
The whole idea is you know, you have radiation, it releases various inflammatory mediator cytokines, antigens, and then if you can combine that with something that stimulates the immune response, it could lead to greater targeting and attacking of the cancer cells.
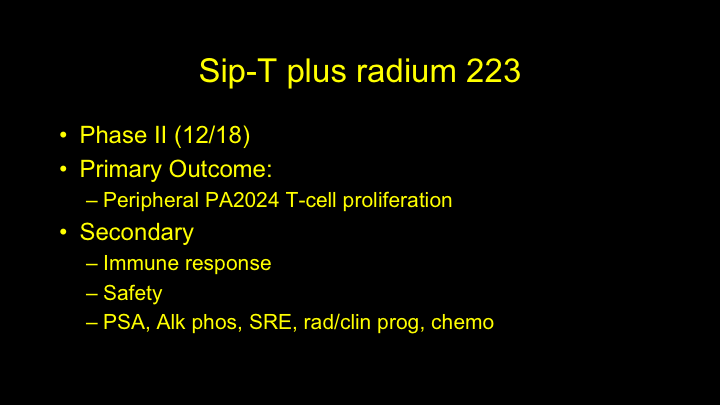
Sip-T Plus Radium 223
So, there are several studies looking at this currently. There is a Phase 2 trial that was originally scheduled to complete in December of 2018. I think it might be a little delayed from what I hear, but it is going to look at peripheral T-cell proliferation, immune response, safety, PSA, alk phos, radiographic and clinical progression, and time to chemotherapy. So, I think this holds a lot of promise to see, when done together, if there is actually an improvement and a synergistic effect to the two, which would be very promising.
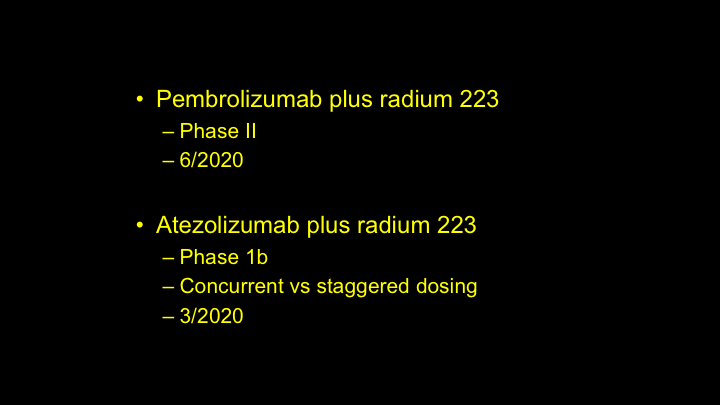
Pembro/Atezo
So, then you have the PD1 and PDL1 inhibitors that are actually being used right now in clinical trials, but those won’t be completed for a little later, but it’s encouraging to see the use of some of these other, more second generation immunotherapies used in clinical trials with Radium 223.
March-April 2015
The discussion of radium 223 really brings into—it gives us the opportunity to talk about immunotherapy and radiology, and I think this is something that we’ve noticed and gave us an opportunity for a former colleague of mine, Jennifer Kwak, to write a great review article about this in RadioGraphics, because you will see immune mediated adverse events. And oftentimes, they will show up on the scans that you get for follow-up, CT scans. You will get colitis, which can be life-threatening, you will get hypophysitis, you can get various things, pancreatitis, just inflammation to normal cells, and it’s important to recognize that these aren’t signs of disease progression. It’s just actually the drug working, and in fact there was a study published in the American Journal of Radiology that talked that the greater number of immune adverse events you had on imaging, the better the response was clinically. So, I think it is something to be aware of. Oftentimes, things will look stable before they get better, or things could potentially look worse before they get better. Be careful if you see something that talks about progression, especially if it is a single time point. One thing we always request—well, we don’t request it since we’re on the same EMR, but we often—we look through the medical record, we look when they started immunotherapy, because that will have a huge impact as to how we interpret those images. So for those of you practicing, make sure that you have a good working relationship with your radiology team so they understand that.
Radium 223 Plus Chemotherapy
All right, so Radium 223 plus chemotherapy. This was one area that I really sort of was incredulous, and I didn’t think this would be successful.
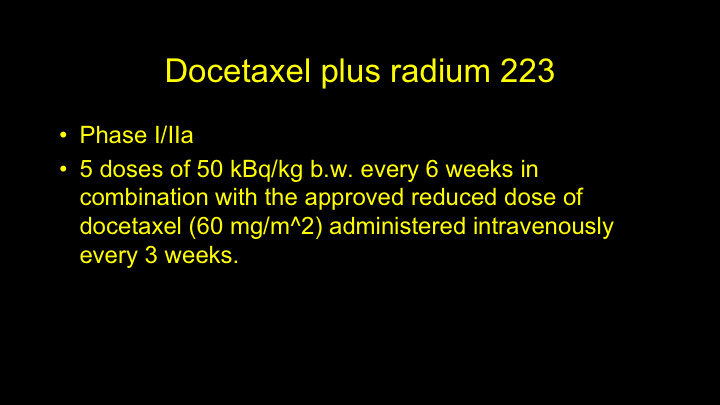
Docetaxel Plus Radium 223
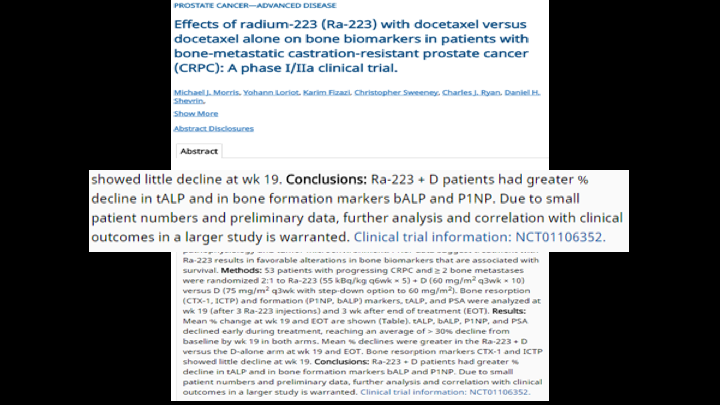
So far, the preliminary data shows that it could be safe, and maybe it has some efficacy. So, Phase 1/2a trial had five doses of Radium at 50 kBq, I think right now it’s 55 kBq’s every six weeks in combination with a reduced dose of docetaxel. This was administered intravenously every three weeks.
Prostate Cancer—Advanced Disease
This was from, I forget, GU ASCO maybe a year or two ago, I think two or three years ago, talked about the safety profile, that it was actually safe, and they saw a response in the total alk phos, and P1NP, which is a bone turnover marker, so again I think this actually holds some promise.
Phase III
Again, I think this actually holds some promise, and Phase III trials I think are currently in development looking at metastatic castration sensitive prostate cancer, and those patients will get hormones, docetaxel and radium versus hormones and docetaxel. And also in CRPC, we’re looking at docetaxel vs docetaxel plus the radium.
Radium 223 Plus AR Inhibitors
So Radium 223 plus the AR inhibitors, this was sort of the low-hanging fruit, and I think most people would agree, when we were thinking about this year ago, this was sort of the easiest hurdle to overcome, and this was probably the first combination that would be approved.
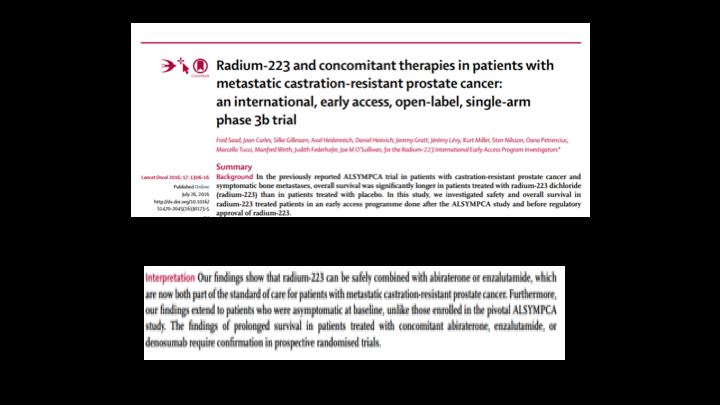
Radium-223 and concomitant therapies in patients with metastatic castration-resistant prostate cancer: an international, early access, open-label, single-arm phase 3b trial
This comes from the expanded access trial. Fred Saad published this et al in Lancet Oncology in 2016. This I think included maybe 7 or 800 patients that actually showed that it was safe in patients who actually received abiraterone, enzalutamide, and denosumab with Radium 223. Not only did they find that it was safe, they actually saw some findings that suggested a prolonged survival in those patients that actually received abi, enza, and denosumab, with the Radium 223. This was designed similar to ALSYMPCA where patients were given Radium and kept on their normal standard of care therapy. In ALSYMPCA I don’t believe any patients received abi or enza.
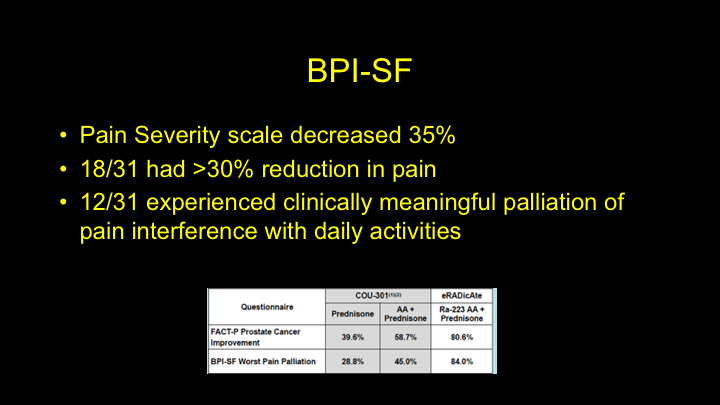
BPI-SF
They also reported that it was save. The pain severity score decreased in 35%. 18 out of 31 had a greater than 30% reduction in pain, and 12 of 31 patients had clinically meaningful palliation of pain, so good results here with regards to quality of life and pain. And also safety.
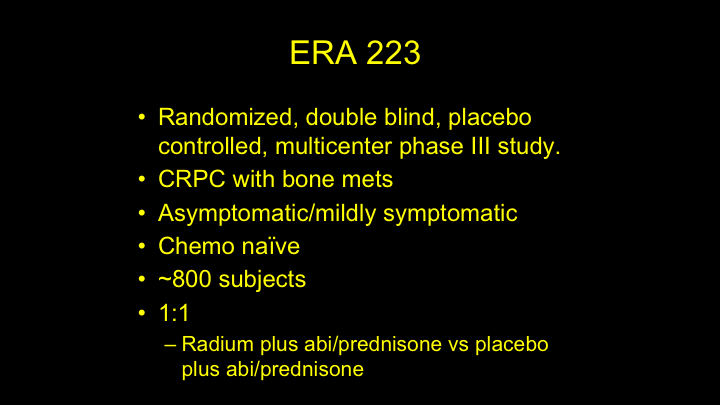
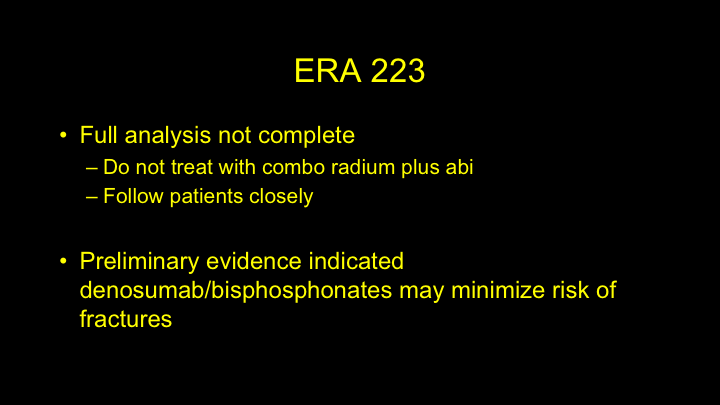
ERA 223
So, November 30th we’ll talk about ERA 223. So this is a randomized double-blind, placebo-controlled, multi-national, multi-center Phase 3 study that is looking that is examining patients with CRPC with bone mets, and the patients were asymptomatic or mildly symptomatic. They were chemo-naïve, and it included roughly 800 patients, and they were randomized in a 1:1 ratio to either radium plus abi and prednisone versus placebo and abi and prednisone.
Important Drug Warning
So November 30th, 2017, I think I was in Chicago for – – and this red box warning comes out.
November 30, 2017
The Independent Data Monitoring Committee reported an increased incidence of deaths, and fractures, and they required that the study be unblinded. So, there’s very limited information, but they did report that the incidence of fractures was 24% in the treated arm versus 7% in the placebo arm, and deaths were 27% versus 20%.
ERA 223
So the full analysis isn’t complete, and I don’t think we’ll see the data form that for at least a few months, but the current recommendations are not to treat anyone with radium plus abiraterone, and for those that were treated, to follow them closely. Interestingly none of these—all of the doses of radium were actually completed much earlier so this was during the follow up phase.
They also did announce that there was some preliminary that indicated that denosumab or bisphosphonates may minimize the risk of fractures, but again that’s all we have, and we don’t have more data on that.
Stratification
In that study, the patients are stratified based on geography, their use of denosumab/bisphosphonates, and total alk phos. So, it will be interesting to see that data to see if geography played a role in some of this, and also to see how denosumab and these bone protective agents actually helped.
Failure is success if we learn from it.
So failure is success if we learn from it, and I think that’s true. And we’ve seen a lot of quotes about failure all the time, and I think, you know, we can’t take failure as a reason to stop trying or just totally pivot 180 degrees.
A Successful Failure
Chuck Ryan wrote an interesting blog post on – -Today recently about this trial, and talking about equating it to the Apollo 13 mission, and for those of you familiar with that, it went up, the mission was to land on the moon. There was an explosion due to an oxygen tank that exploded because of an uncovered wire. Obviously, that is catastrophic when you’re in space, but they actually figured out away to get back to earth safely, so that was a successful failure. So, I think this sort of just puts things in perspective that we don’t need—shouldn’t overreact.
Hypothesis
I think we need to look at things carefully, and we need access to that data to really dissect what are the areas that went wrong, what are the, you know, what is it telling us? That is why we do these clinical trials, and that is why we need access to this data to really see where we go from here, but in the meantime, I think it is kind of fun to hypothesize with regards to why this might have happened, and when I talk about it with Neal, and Dave, and various other people, I think one possible hypothesis is that maybe there is a flare response. We do know there is a flare response with abiraterone. So, in the Phase 3 trial looking at abi and prednisone, there was a flare response, and they saw a discordant bone scan in 12 of 23 patients, so discordant in the fact that the bone scans looked worse, but the PSA went down greater than 50%, and those bone scans that looked worse, 80% of those scans actually improved on follow-up. So flare was seen in 43% of responding patients. And this goes back to Dr. Reiter’s point, that bone scans aren’t very good, and yet we incorporate them into all of our clinical trials.
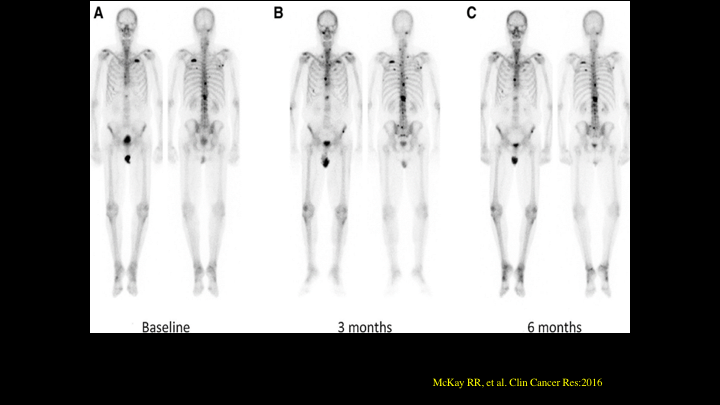
McKay RR
This is an example of flare published in 2016, but again we have seen this for years, but you take a case at baseline and you look at him at three months, and you look at them at six months, and you see a sternal lesion that will look hotter, a little worse at that three-month scan, and it sort of stabilizes. And again oftentimes you see this, especially in breast cancer patients if they have osteolytic disease. They often get treated. The bone scans look terrible, and they stabilize or look better. And again, that is most likely bony reparative response to these lesions being treated.
Radium 223 Flare
Radium 223, we’re learning more about Radium 223 and how it works, and how it reacts on imaging, and there was a recent study published in 2017 that talks about bone flare and that bone flare is pain flare and/or radiological flare. So bone pain increased in 27% of those patients. It decreased in 49%, and they saw an increased number of lesions in 26%. 74% were stable at three months.
Combination vs Layering?
So the big question is, maybe there is a difference between combination versus layering, so if you look at the expanded access trial, you look at Neal’s ERADICATE trial, maybe the difference here is combination versus layering. In ERA 223 these patients were started on abiraterone with Radium 223 within a three-day window simultaneously. In ERADICATE, one-third of patients I believe were started on abiraterone at least a month before and two-thirds of patients, two-thirds of the patients were actually started on abi 60 days at least 60 days before they were started in Radium. So again, maybe that’s one of the differences. Maybe you sort of clear that flare response in the beginning, and then you add the radium, and that is why we’re seeing those improved survival rates, when it’s layered as opposed to combination. Again, we don’t know this for sure, but just kind of fun to speculate.
PEACE III
PEACE III is another trial. It’s a randomized multi-center, phase III trial comparing enza versus enza plus Radium 223. Very similar to the ERA 223 trial, so that will be interesting to see what that reports, and that is scheduled to be completed in November 2019.
Donald Rumsfeld
You know, when this quote first went up or was mentioned years ago, it was confusing, and I know a lot of us laughed, but the more you think about it actually it kind of makes a lot of sense, and “There are known knows, these are things that we know that we know. “There are known unknowns, that is to say there are things that we know that we don’t know, but there are also unknown unknowns, there are things that we don’t know we don’t know.” That’s mind-boggling right, and it actually makes a lot of sense.
Every day I’m reminded that there are so many things that I don’t know I don’t know, and it’s kind of –it makes life a little more interesting, so kudos to Donald Rumsfeld for being able to articulate that on the spot.
Radium 223
So anyway, “Radium 223:” I think the personal ad is still out, “Enjoy bone seeking journeys and long walks on hydroxyapatite crystals. I help patients live longer while promoting safety. Seeking like minded partner who likes bone as well but ideally could treat soft tissues as well,” because that would be a marriage made in Heaven. I like that there as well.
ABOUT THE AUTHOR
Phillip J. Koo, MD, is the Chief of Diagnostic Imaging at the Banner MD Anderson Cancer Center in Phoenix, Arizona. Prior to this, he was Chief of Nuclear Medicine and Associate Professor of Radiology at the University of Colorado School of Medicine in Aurora, Colorado. He completed his fellowship at the Harvard Medical School Joint Program in Nuclear Medicine in Boston, Massachusetts. Dr. Koo is a diplomate of both the American Board of Radiology (ABR) and American Board of Nuclear Medicine(ABNM).