Nocturia: Symptom or Disease?
How to cite: Rosenberg, Matt T. “Nocturia: Symptom or Disease?” August 11, 2018. Accessed [date today]. https://grandroundsinurology.com/nocturia-symptom-or-disease
Nocturia: Symptom or Disease? – Summary#
Matt T. Rosenberg, MD, discusses the multiple etiologies of nocturia and nocturnal polyuria and corresponding treatment options, emphasizing the need for shared care when managing nocturia. He then reviews the efficacy and safety of a novel version of desmopressin for reducing the kidney’s production of urine at night time.
To further expand your knowledge of the management of nocturia, visit the Nocturia Next Generation Learning Center.
The Quality of Life Burden of Nocturia and Nocturnal Polyuria #
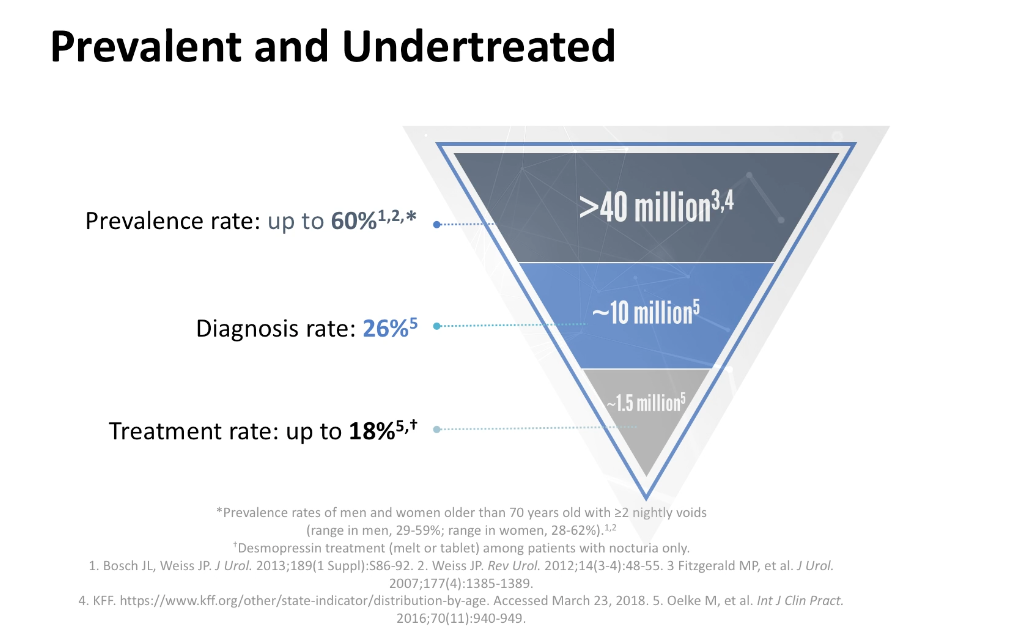
The International Continence Society defines nocturia as waking at night to urinate, with each voiding episode preceded and followed by sleep. Urologists consider waking to void twice or more per night to be clinically relevant nocturia. Nocturnal polyuria, while similar to nocturia, refers to nighttime urine production greater than 20% of the total urine volume output for younger adults, and greater than 33% for older adults.
Evaluating the Causes of Nocturia#
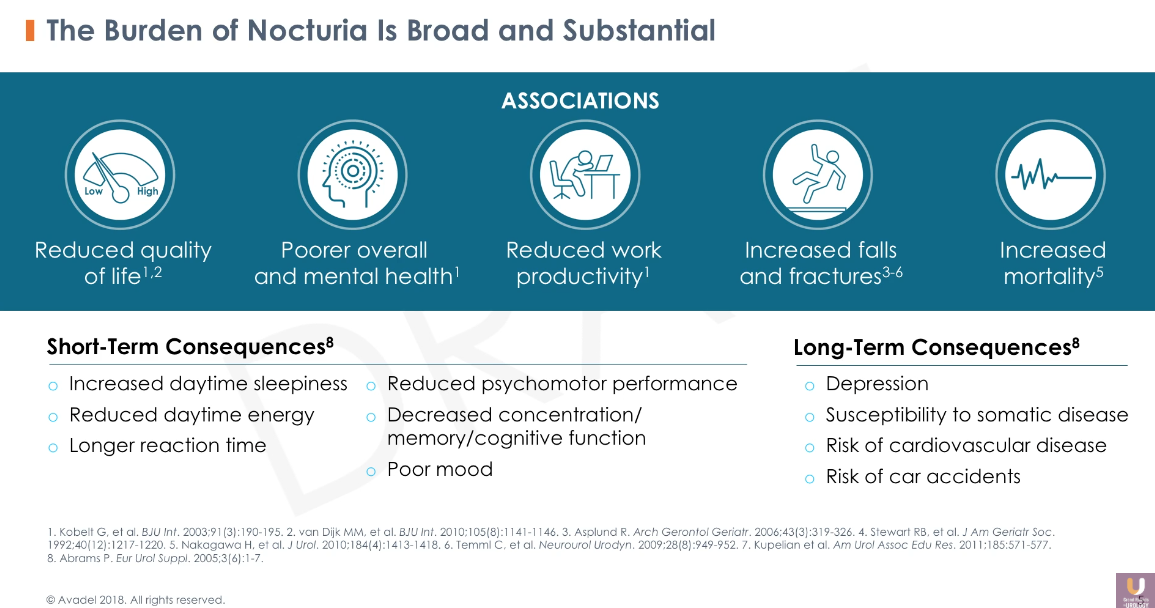
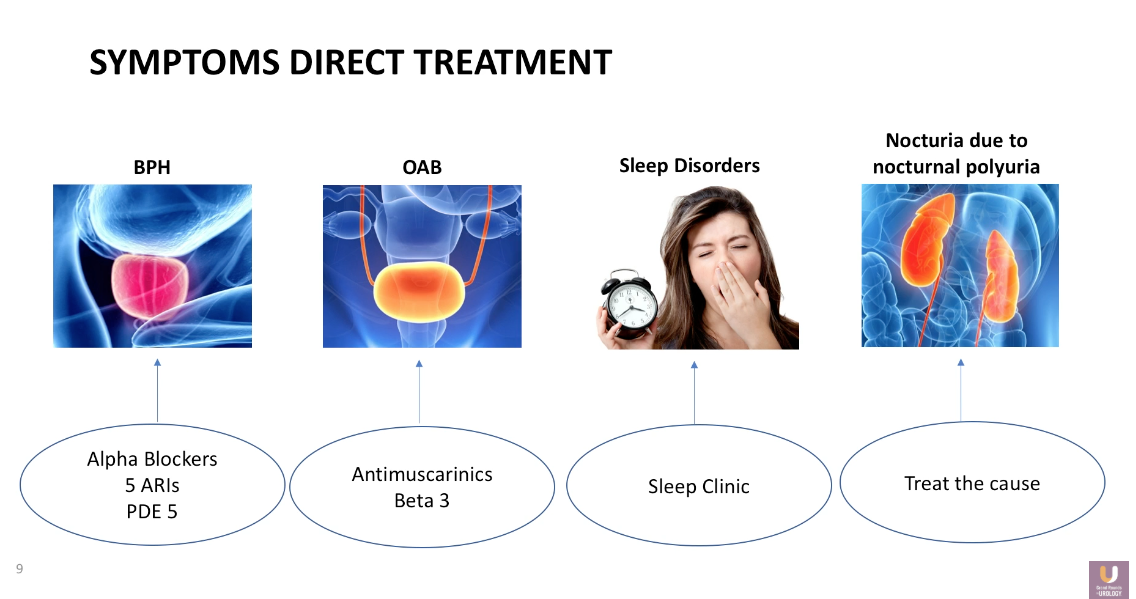
Nocturia is a multifactorial condition. Benign prostatic hyperplasia (BPH) can obstruct the bladder’s ability to empty completely, leading to a shortened filling time, and as a result, cause the patient to void more frequently at night. Similarly, overactive bladder (OAB) and small bladder capacity can lead to nighttime urination. Additionally, patient’s symptoms may be due to unrelated sleep disorders in certain cases. Dr. Rosenberg emphasizes the idea that despite the frequency or cause of nocturia, physicians should select patients to treat based on degree of bother.
The Multiple Etiologies of Nocturnal Polyuria #
Dr. Rosenberg categorizes the etiologies of nocturnal polyuria into overconsumption, overdiuresis, and too little antidiuresis. Oftentimes, patients will habitually drink water before or during the nighttime. Patient counseling can address this issue. Overconsumption can also be a challenge for patients with dipsogenic diabetes insipidus or diabetes mellitus. Patients can experience overdiuresis due to third-space fluid absorption, diuretic medications, renal conditions, and congestive heart failure. Lack of antidiuretic hormone attributes to nocturia, as well.
Nocturia Treatment Options #
Dr. Rosenberg advises physicians to first address any behavioral patterns or separate factors a patient might have when treating a patient with nocturia. For example, consider alpha blockers, 5α-Reductase inhibitors (5-ARIs), or phosphodiesterase type 5 (PDE5) inhibitors for treating BPH, antimuscarinics or beta-3 adrenergic receptor agonists for treating OAB, and refer patients to seek care from a sleep clinic for any sleep disorders they may have.
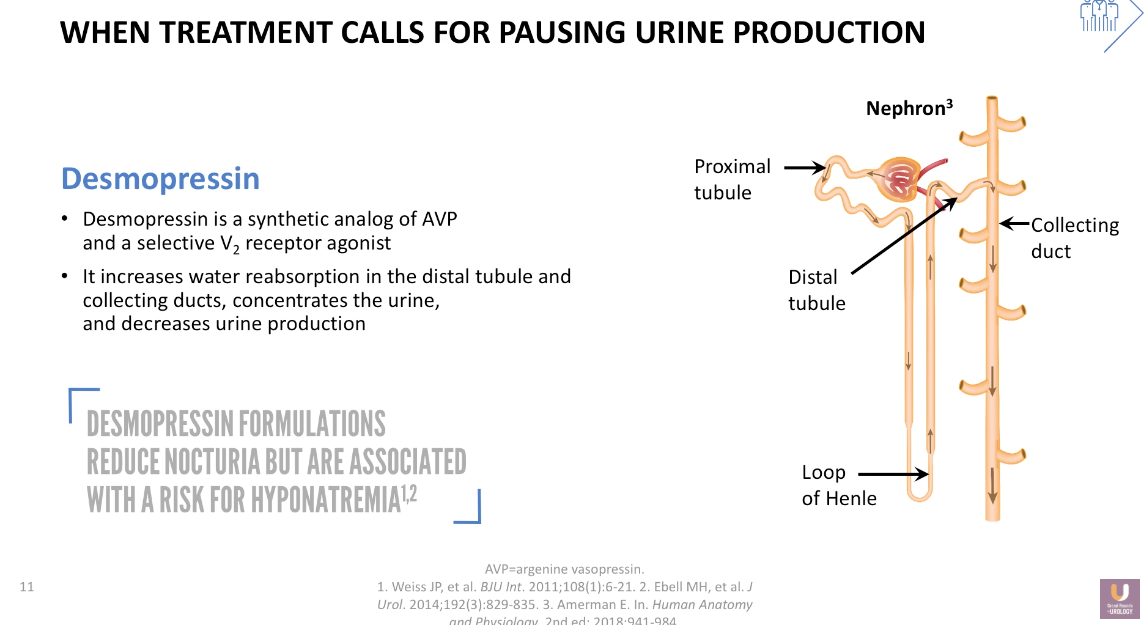
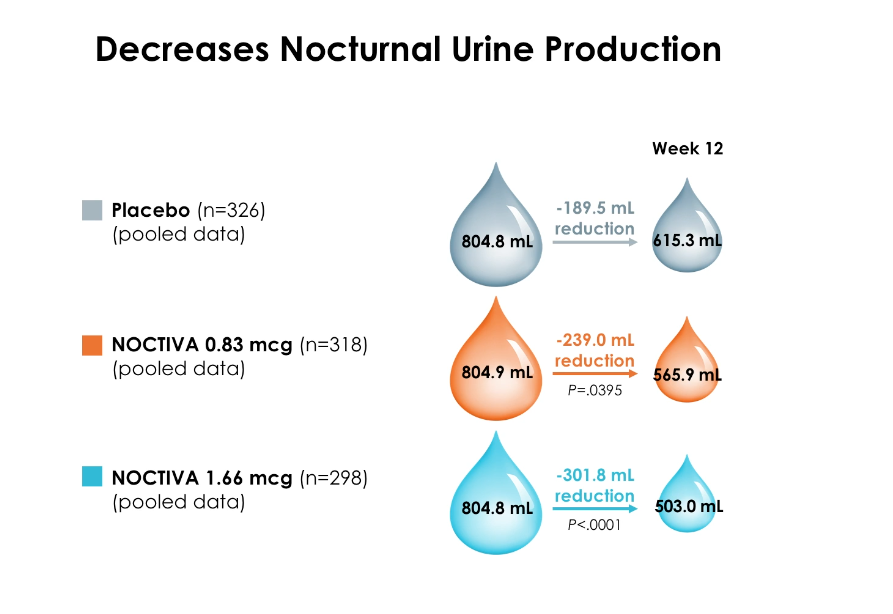
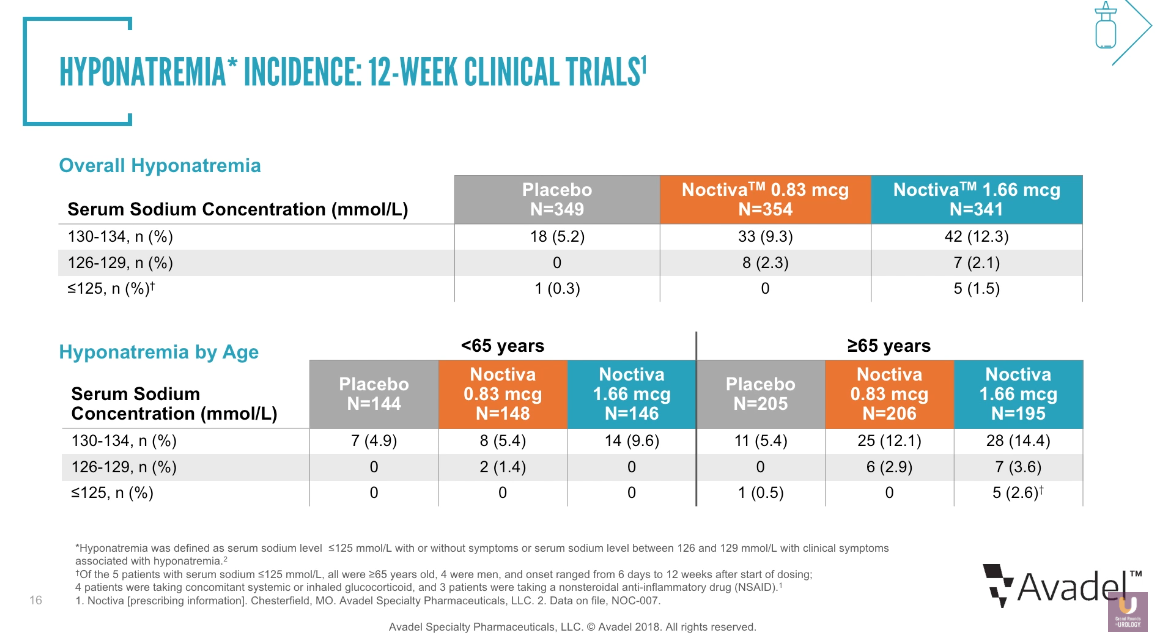
Desmopressin: Pausing Urine Production in the Kidney #
In certain cases, however, it is necessary to directly treat patients for nocturnal polyuria due to a lack of antidiuresis. Dr. Rosenberg explains that the mechanism of action for desmopressin is to increase water absorption in the distal tubule and collecting ducts, therefore decreasing nocturnal polyuria. This does not change the total volume of urine created over a 24-hour period, but instead pauses the production of urine for a small number of hours.
Which Specialty is in Charge of Urine?#
Dr. Rosenberg adequate management of nocturia requires shared care. Urologists should investigate to determine if a patient’s symptoms originate from the prostate or the bladder, while primary care physicians should investigate the kidneys. Urologists and primary care physicians also must work together in general to safely treat and monitor this condition.
ABOUT THE AUTHOR
Matt T. Rosenberg, MD, earned his medical degree at the University of California, Irvine, where he trained in general surgery. He also trained in urologic surgery at Brigham and Women’s Hospital in Boston before changing fields to general practice. Dr Rosenberg has a special interest in the medical management of urologic diseases and has authored or coauthored articles appearing in Urology, The Journal of Urology, BJU International, The International Journal of Clinical Practice, and other peer-reviewed journals. He now practices in Jackson, Michigan, serving as Medical Director of Mid-Michigan Health Centers, and on staff at Allegiance Health, where he served as Chief of the Department of Family Medicine from 2003 to 2006. Dr. Rosenberg is a Senior Editor at the International Journal of Clinical Practice and is Founder and Chairman of the Urologic Health Foundation, a nonprofit group dedicated to the education of primary care physicians in the field of genitourinary disease. In 2011, he was appointed by the AUA Office of Education to be the Coordinator of Primary Care Education.