Advanced Disease — A Real Need for Understanding and Shared Care
How to cite: Petrylak, Daniel P. “Advanced Disease — A Real Need for Understanding and Shared Care” January 27, 2018. Accessed [date today]. https://grandroundsinurology.com/a-real-need-for-understanding-and-shared-care/
Summary:
Daniel P. Petrylak, MD, stresses the importance of taking a multidisciplinary approach when treating prostate cancer. Not only does this mean involving urologists, oncologists, and primary care physicians for better access to therapies and coordination of care, but also involving nutritionist, mental health professionals, and pain management experts for maintaining patients’ quality of life.
(Twitter Question) Reveal the Answer to Audience Response Question #1
- A. Hypertension
- B. Diabetes
- C. Edema
- D. All of the above
Advanced Disease — A Real Need for Understanding and Shared Care – Transcript
Click on slide to expand
Advanced Disease: A Real Need for Understanding and Shared Care
Thank you, David, for the kind introduction. That was a great talk by Mike, and I really enjoyed that, and I think it’s going to be more complex. It’s going to get more complex as we have more treatment options, but I think what is also happening too is we are seeing the use of genetics now as we see in early stage disease to help to predict prognosis. As you saw from Mike Glode’s talk yesterday when we’re talking about PARP inhibition and selecting out different treatments based upon biomarkers, I think it is going to even get more complex. When we have patients with advanced disease, David actually mentioned a case of breast cancer in a patient who was BRCA positive, or at least the sister was BRCA positive. We’re going to have to also not only share care in the patients. We’re going to have to share care in the families as well, and I think that is where we’re going to also make a major impact on patients with metastatic disease.
A Multidisciplinary Approach: Maximizing Clinical Benefits
They have to be monitored very, very carefully, and that is why the shared care and multidisciplinary approach is so important. So it’s going to involve all treating physicians, urologists, medical oncologists, radiation oncologists, potentially primary care physicians as well because we have to manage the hypertension, but I think now we have to also include genetic counselors because of the issue I mentioned before. When we have these next generation sequencing reports that come in, they are very complex. You need somebody to interpret that. We actually just published this in Lancet Oncology. We have a multi-disciplinary genetics tumor board in addition to our GU oncology tumor board, where we sit and we review the different genetic changes and try to match those patients for different trials that are out there. So again that’s PARP inhibition. We’re also looking at trials for MTOR inhibition, for prostate cancer. This is a resistance mechanism of androgen independence, so again, we’re going to need to include those specialties in this care team. So, it’s going to get more complex, and again, the need for communication.
Mental health professionals, we see depression with some of the androgen blockers and these drugs. Exercise I think is crucial to maintaining good quality of life. A nutritionist. For a man to lose a pound normally, you have to burn 3500 calories. For a man on hormone therapy, it’s 4500. These patients all right off the bat need to be counseled, and I do this counseling as well about exercise, maintaining a good muscle tone, getting a personal trainer to help them out in that particular situation to be sure that they don’t lose muscle mass, they don’t gain belly fat. Once you gain belly fat, you can’t get rid of it, and that is a really big problem with our patients, especially if you want to focus on body image.
So, I think all of these individuals are part of the care team. It’s constantly becoming expanded as the disease becomes more complex.
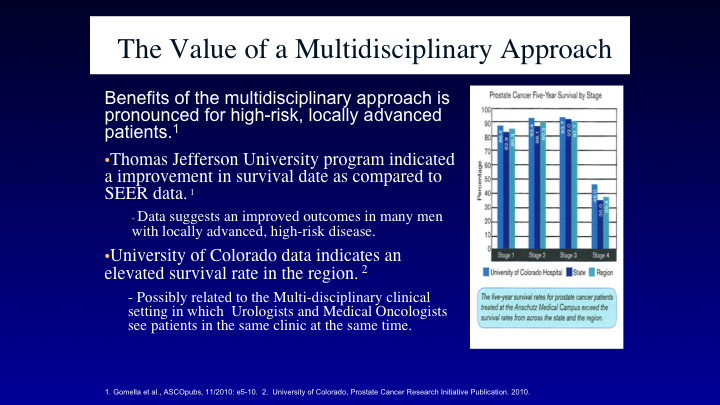
The Value of a Multidisciplinary Approach
So what is the value? I always like to show data. We’ve got two really different, good data sets that tell us that shared care and the multidisciplinary approach actually has an impact on outcome. So, Dr. Gomella and his group looked at their program, and they looked at the survival, and they compared their data to the SEER data, and what they suggested was using this multidisciplinary approach actually had a better outcome than what you would have seen from matched patients from the SEER database, and the same thing with Dave Crawford’s group at the University of Colorado. If we’re using that same shared care approach you’ve actually got a better outcome for other patients comparatively treated in the same region.
Now, it doesn’t have to actually be a physical clinic, and the way we have things set up at Yale is my office is actually in the Urology Department. So I’m right across the hall from John Colberg. Toby Chai who works a lot with bladder cancer is right down the hall, Pat Kenney, we’re all in the same area. So, we actually have our multidisciplinary discussions, not only in Tumor Board, but in off hours, and it’s not uncommon for John to drop by my office. We put the EPIC list up, and we look to see who the common patients are. And we sit and discuss them and see where they are going. The same thing after his clinic, I’ll walk down to his office, look over the list and see where things are. So again, this is our way of coordinating. I think each provider has got to come up with a different way in this situation.
The Value of a Multidisciplinary Approach #2
Our goal is optimize patient outcomes, to improve the access to specialty therapies, again as I mentioned before with the genetic tumor boards, to look at an efficient schedule. We don’t want to repeat things. To coordinate care, and again that is all important with coordination. I’ve seen things slip through the cracks. As Mike was talking about before, having an EMR is an advantage. I actually saw somebody yesterday who was a fairly interesting individual, had been bouncing around between medical oncologists, between urologists and radiation oncologists, and he had a rising PSA. He was irradiated. He was supposedly M0 at that time in the prostate bed, but everybody forgot to maintain his hormone therapy. Came to see me yesterday with a new metastatic lesion. I said did anybody check your testosterone recently, 319. So he is back on androgen blockade again. But these—if you don’t have good coordination, these are the simple mistakes that can happen, and the EMR is a big advantage to that because you have a flow sheet, and you have a timeline that everybody can look at and see if there have been things that have been missed.
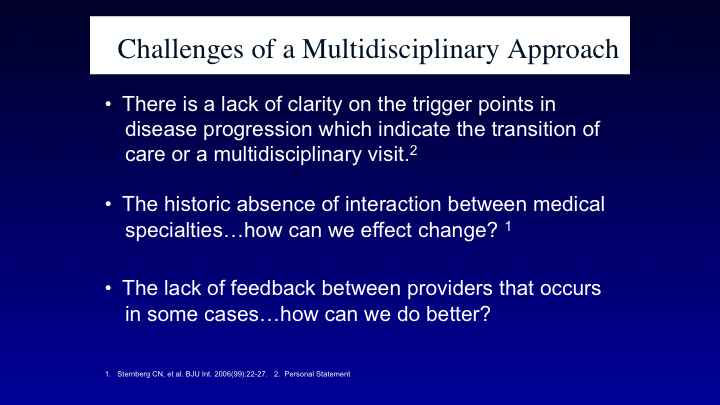
Challenges of a Multidisciplinary Approach
So what are the issues and the challenges? What is the trigger point? When do you send a patient to an oncologist or radiation oncologist? When should they have that consultation? We at Yale do it early, and as Mike mentioned before some institutions will hand the patient over when the PSA rises. That’s what we do, but the patients still see the urologist on a regular basis to maintain that continuity. So the feedback, as I said before, is really crucial to taking care of these patients.
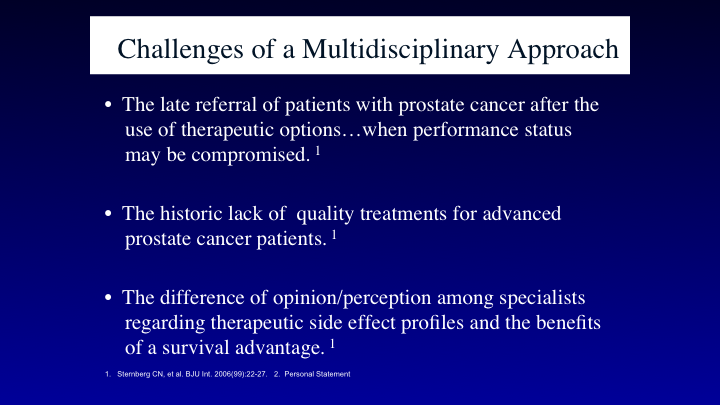
Challenges of a Multidisciplinary Approach #2
Later referral means that they can’t seek clinical trials. They can’t sequence the drugs in the proper fashion, so again, I think the early referral is better, and I don’t really think it matters who you refer to in the late stage of disease as long as they understand what they are doing, and they have access to trials and access to the most important treatments.
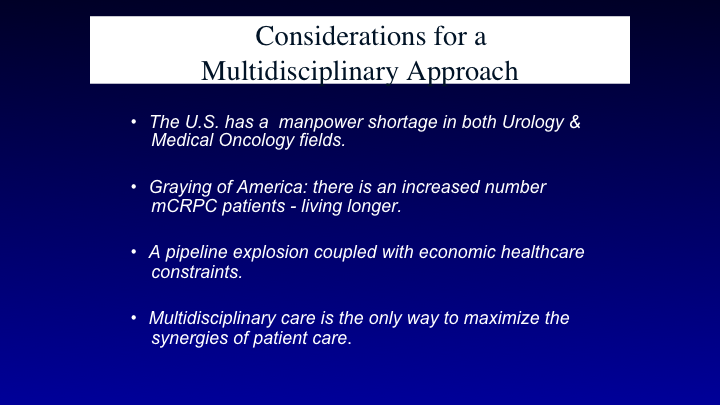
Considerations for a Multidisciplinary Approach
So we are facing a challenge in manpower in urologists and oncologists. There’s actually a shortage of oncologists across the country, and that is why we need these coordinations to be done properly. Also, again, to include advanced care practitioners, nurse practitioners. I have a terrific NP, Kristen Crowley, with my group who really helps to maintain the continuity. You need a quarterback in this situation.
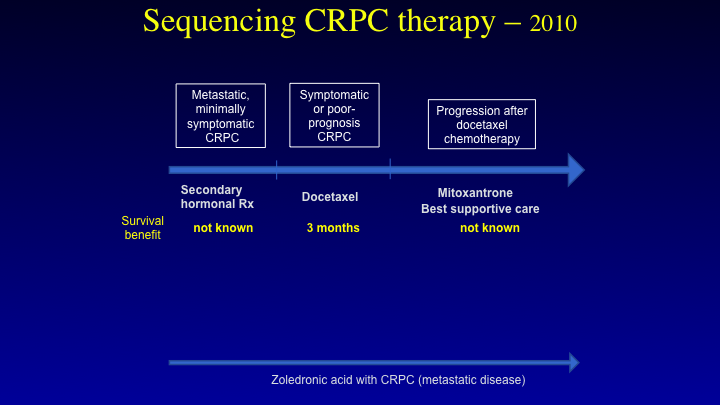
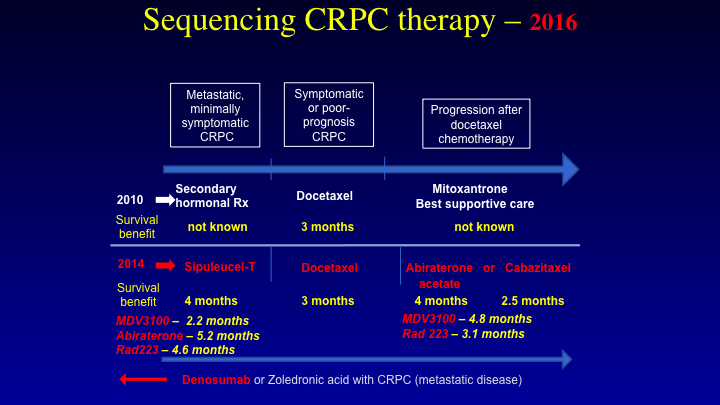
Sequencing CRPC Therapy — 2010
Let’s look at the disease. I’m going to sort of review the same things that Mike did before in how we look at treatments. Let me put some caveats in, because there are a lot of myths that have come about that have I think impacted upon how a urologist perceives the treatments that we’re giving, and then how visa versa. So, this is the therapeutic landscape in 2010. We had only one drug that we could use for castrate resistant prostate cancer. That was docetaxel. Mike mentioned before that it was a three-month improvement in median survival, and that is correct. But, what was neglected in that number was the fact that docetaxel was on the compendium list for prostate cancer. It was approved for breast cancer, but you could use docetaxel and in fact when I looked at the SWOG 9916 data, I used to have to read every chart, and some of the things that I saw were quite telling. One individual had a response to mitoxantrone and prednisone, and then they switched him over to standard of care docetaxel, or at least the docetaxel they could obtain, because he didn’t respond quickly enough. So, that number that you are seeing with three months I think is a diluted number. It’s probably higher. It’s probably a 4 to 5-month difference that was seen, and again this is where moving drugs up front you get really the pure number as to what you are seeing.
Sequencing CRPC Therapy—2018
This is where we are now in 2018. We see that sipuleucel T is approved, radium is approved, Zytiga is approved, and the same thing with enzalutamide. How do you sequence, and how do I look at this in terms of the shared care model?
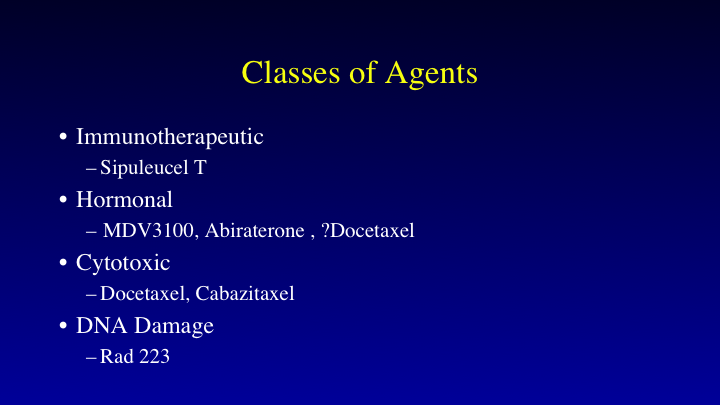
Classes of Agents
I like to look at this in terms of classes. Immunotherapy agent, sipuleucel T. Sipuleucel T I think has gotten a bad name because of the fact that we don’t see an improvement in progression-free survival, we don’t see PSA declines, although I’ve seen them with this drug, but for the most part you don’t see it. We do know that you do have activation of T memory cells, even up to five years after the implementation of sipuleucel T treatment, and in fact, the controversy was how could you have a survival benefit if you don’t have PSA declines, nor if you have any changes in progression-free survival? Well, I think now you are seeing that with the checkpoints. You don’t see a progression-free survival difference. You do see an overall survival benefit, so there is something about the immune system that is being activated over a long period of time that I think makes a difference in these patients, and I think the data is real. Hormonal agents, MDV3100 or enzalutamide, abiraterone, maybe the taxanes as well. The androgen receptor has to get to the nucleus, and has to be translocated, docetaxel, cabazitaxel will interfere with that, and they are both cytotoxic agents as well.
DNA damage is becoming more and more important. We know that radium will cause a double stranded DNA break, but the PARP inhibitors will probably get approved in the next couple of years for prostate cancer, and again, we are going to have to molecularly select those patients. Patients with BRCA mutations. CHK2 mutations also are involved in this, about three or four different mutations of DNA repair, in fact about a third of patients probably will eventually receive a PARP inhibitor. The question is- is that better than platinum, and is that better than standard therapy in that situation. The randomized trials are ongoing.
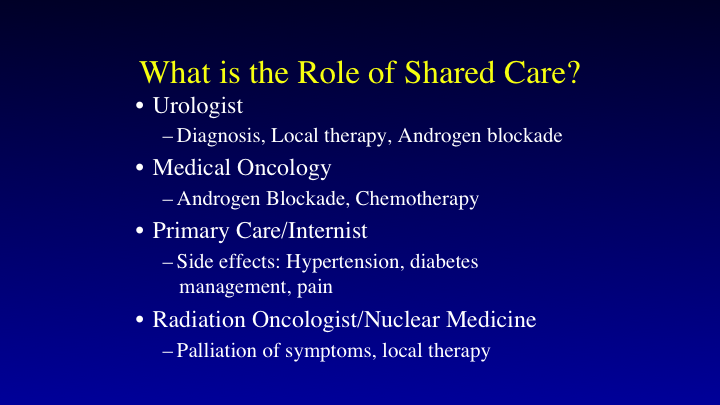
What is the Role of Shared Care?
This is the way I look at the practice team, the urologists will diagnose the patient. They will apply local therapy. They will start androgen blockade. The medical oncologist will consult the patient when they are going on androgen blockade. What is the right secondary treatment to use? Should they go with abiraterone? Should they go with docetaxel? And then what about quarterbacking with chemotherapy? I think the interaction between the two groups is most important to patient care. The primary care and the internist helps with side effects, and again this is where the advantage of the EMR is. You can actually see who the primary care doc is. You can send them a note. Is end them notes by EPIC all the time about managing hypertension, because if you’ve got complex cardiovascular issues, I don’t want to monkey around with their drugs in that situation even though I am certified in internal medicine, I’m not up on the most recent cardiovascular drugs.
Diabetes management- I actually encourage people to put patients on Metformin if they possibly can go with it, because we know there has been some reports of synergy between Metformin and agents such as abiraterone, and this actually may improve survival.
Palliative care also should be involved early, not only for pain management, but for management of other side effects as well, and there has been a trend in the country towards moving patients towards palliative care referrals earlier, and again not because you re going to give up on them and not treat those patients with these drugs, but because by managing symptoms you may be able to get a better dose in of individual drugs. You may be able to get better treatments in and prolong their treatment time so that actually I think is an important referral.
The radiation oncologist, I know it is a battle between who is going to give the isotopes, but they can palliate symptoms, take care of local treatments, administer isotopes, and again coordination is important. I work very, very closely with my radiation oncologist, Dr. Yu, up at Yale, who actually just published a very interesting paper on the role of alternative medicine in cancer treatment, and what he found was that patients who go with alternative medicine in breast cancer and in colorectal cancer actually have a poorer survival. It doesn’t make a difference in prostate cancer. That may be because of the longer course of the disease. But again it’s important to communicate with the providers.
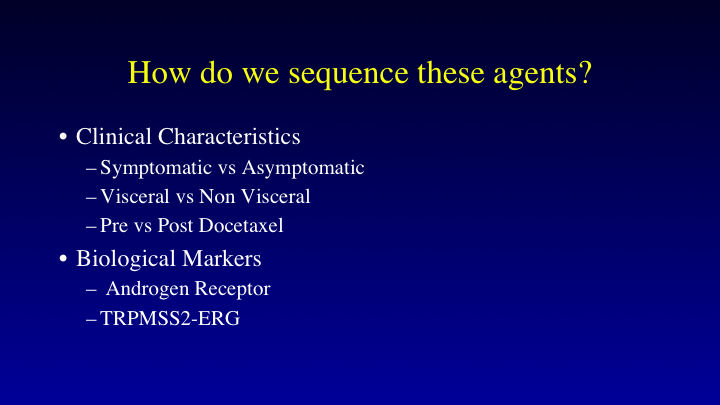
How do we sequence these agents?
What is going to happen now is sequencing, and this is where I think the big confusion is going to be. This is where we can use molecular markers. Right now, without having a molecular marker approved for this disease, I think of the patient in terms of symptomatic versus asymptomatic, visceral versus non-visceral, pre-docetaxel versus post-docetaxel. That is somewhat arbitrary, but we’re going to have biological markers in place. The androgen receptor, namely the ARV7, can be obtained outside of a clinical trial right now with several different organizations. I use it but not as strongly because there are other mechanisms of action or resistance with abiraterone and enzalutamide. TRPMSS2-ERG may mark different forms of the disease that may be responsive to hormone therapy, and then finally again as I mentioned before DNA repairing mutations, the PARP inhibitors, that is going to be big.
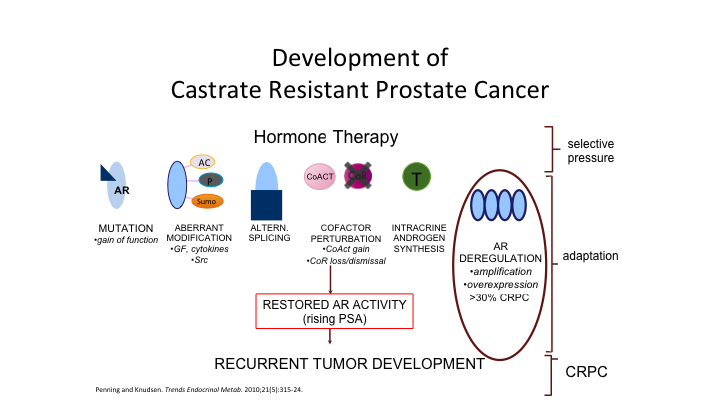
Development of Castrate Resistant Prostate Cancer
We’ve seen this throughout this meeting before. This is just the cartoon as to how patients become castration resistant. There are many roads to Rome, so this is not the same disease in everybody. We know also that there can be a neuro endocrine variant, and this is something that all providers must be looking out for at any given moment. It co-exists with the androgen sensitive form of the disease. So the androgen sensitive form makes PSA, tends to go to the bone. The neuroendocrine component also makes a little bit of PSA, not as much but it tends to go to visceral sites.
The other thing I forgot to mention that we now have to look out for, and there is an FDA approved drug, it’s the first drug that is approved for a pan tumor treatment. That is something called MSI, or microsatellite instability. Every prostate cancer patient should be checked for this. Unfortunately, it’s only 2% of patients in the United States that have this, but this marks for sensitivity to a checkpoint inhibitor called pembrolizumab. And I’ve actually picked up three patients in the last two years who are MSI high. Two of the three patients responded to pembrolizumab. The third patient was very interesting from the standpoint that he progressed initially on pembro, and I put him on oral cytoxan because I thought that would knock off some of his T suppressor cells, and now he has had a beautiful response. Disease predominantly in the liver as well as in the peritoneum. But this is also something that all providers should be looking out for every minute, because you can impact a significant difference in survival if you look for this. So again prostate cancer is a heterogeneous disease. All providers should be aware of that, and you can get to Rome by many different roads.
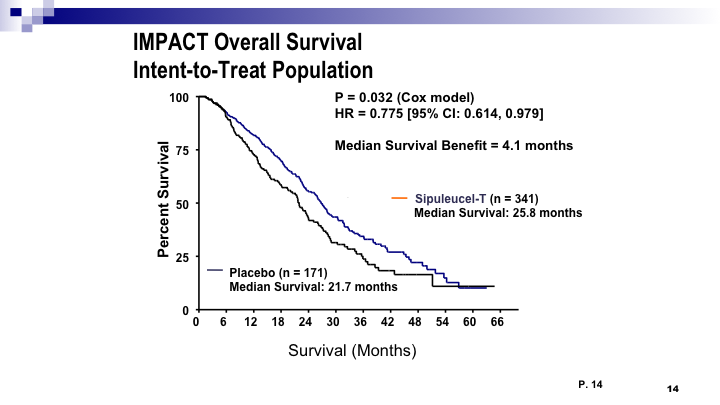
IMPACT Overall Survival Intent-To-Treat Population
So this is the sipuleucel T data that we’ve talked about already before. We know that, from the IMPACT trial, there is a difference in survival, a median of about four months. and the important thing is we should be using this early.
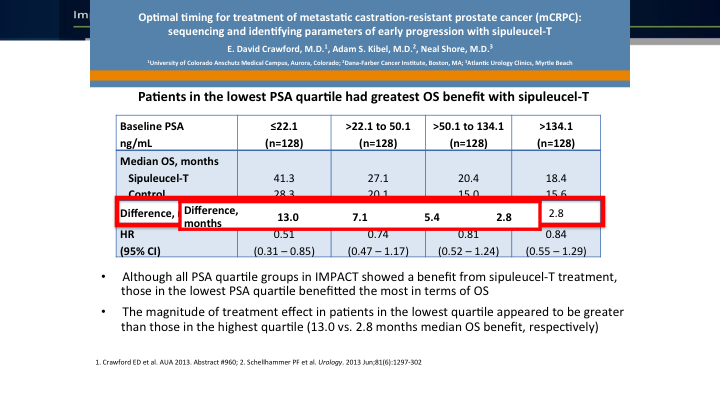
Patients in the lowest PSA quartile had greatest SO benefit with sipuleucel T
The important thing is we should be using this early. I give it right up front because of the fact that the data that Dr. Crawford was involved in shows that if your PSA quartile of less than 22, that is where you get the biggest survival difference. It’s a 13-month difference in median. And again, we see this trend of using drugs earlier where we have the difference. So, I like using it early, and then that also lends to the fact that if you’ve got activated T cells, they may actually be chewing up damaged cells later on.
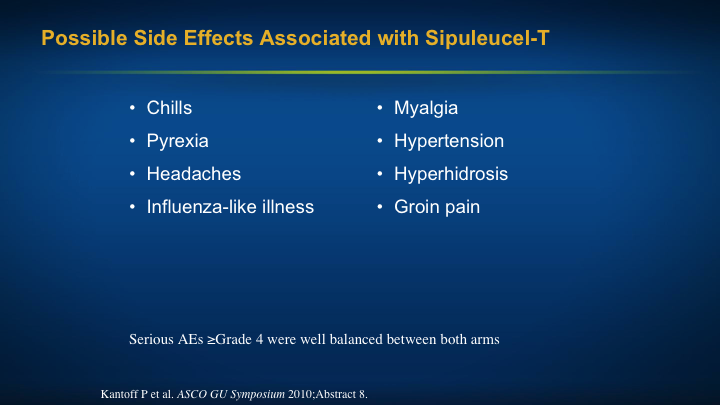
Possible Side Effects Associated with sipuleucel T
There is something called the Abscopal effect that we do know about with patients who are being irradiated. You irradiate one spot, you give immune therapy, and then the other areas respond. That is because you are causing cell death and releasing antigens. Sipuleucel T very easy to manage the side effects. Tylenol for the fevers, or in the worst cases a narcotic, but chills, pyrexia, headaches, those are the big things, very easy to give, and over in a month.
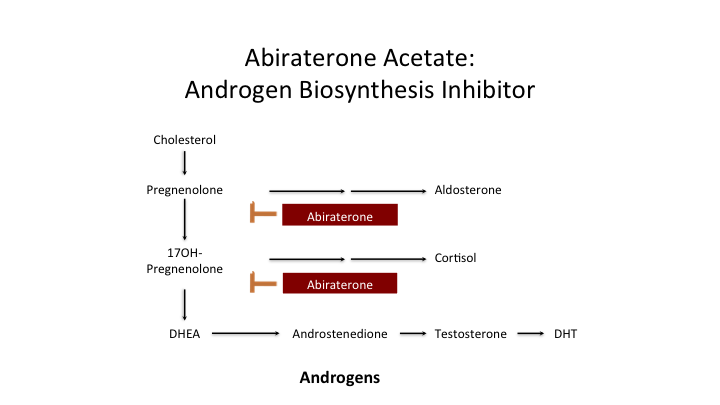
Abiraterone Acetate: Androgen Biosynthesis Inhibitor
We’ve talked a lot about abiraterone, the androgen biosynthesis inhibitor.
COU 301: Overall Survival
The COUGAR trial, the guys from COUGAR opened up another company. They called it PUMA, which I think was kind of funny. They actually have a signal transduction inhibitor, but we see a survival benefit.
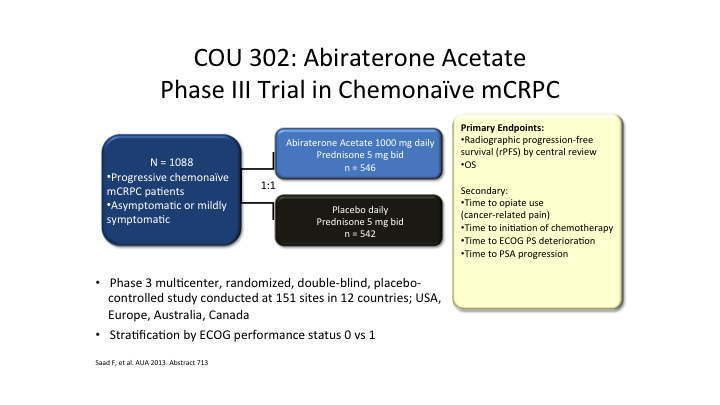
COU 302: Abiraterone Acetate Phase III Trial in Chemonaive mCRPC
Again, you want to use this drug early, as early as possible right at the beginning of androgen blockade. People ask me how do I select chemotherapy versus the next generation hormones? Well, some patients can’t afford it. Other patients just want to get it over with, so those patients will—we still have some patients treated with docetaxel in the early situation, but this is leading to another issue.
So this is the COUGAR 302 trial, which was for early Zytiga. So what is going to happen when these patients progress? How are the care providers going to manage these patients in this situation? We generally see that if you go on one next generation androgen blocker and switch to the other, you’re not going to respond. So what do you do right up front? Do you go on docetaxel, do you go on cabazitaxel? We really don’t know the answers so the disease is going to change, and it’s going to get more complex, as we move these drugs up earlier because you are changing the biology. Are you going to see more neuroendocrine develop later on because you’re treating these patients earlier.
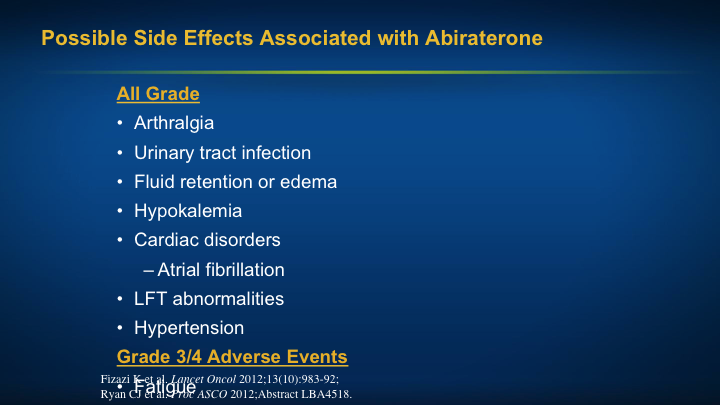
Possible Side Effects Associated with Abiraterone
So the internist, the medical oncologist, the neurologist has to look out for these particular side effects. Again, communication is important. Arthralgias, yep, I see it, not a big deal, but the big things I have to look out for liver function abnormalities, which can be severe in some patients, about 2 to 3%. Cardiac disorders, fluid retention, atrial fibrillation, and then monitoring their blood pressure. That is the big thing. I have everybody go home with a home blood pressure monitor. They get their own cuffs, or they go to CVS or Rite Aid to check themselves once a week, but we do monitor that, and then we work with the internist to be sure that they are properly taken care of in this situation.
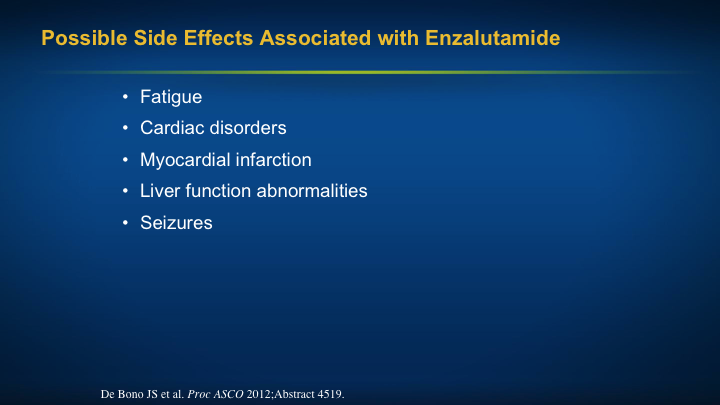
Possible Side Effects Associated with Enzalutamide
Enzalutamide, again, very similar survival benefit, but different side effect patterns, fatigue, cardiac disorders, myocardial infarction, liver function abnormalities. The seizures has been downplayed. There has been a paper that has actually put that to rest. My big problem with this drug has been the fatigue and I’ve been trying to overcome this by having the patients take the drug at nighttime. It may be that some of the other agents that are used for ADD can be helpful. We’re not really sure about that, but generally, if somebody is frail, they are not going to do well with this drug. Same thing if they’ve got diabetic—this is not the drug of choice in my mind in a diabetic, you don’t need the prednisone. Again, you don’t look at the one thing. You look at the whole patient in this situation.
Conclusions
So in conclusion, the optimal sequence of these agents has yet to be determined, and it’s going to change because of the early use of abiraterone as well as docetaxel. And again, also enzalutamide, if that drug gets approved for the M0 state, what are you going to then do subsequently when they progress with bone metastases. We should offer either docetaxel or Zytiga for those high-risk patients at the initiation of hormone therapy, and then again, I like giving my immune therapy early, and it’s again, we have to coordinate between all of the care providers and ensure good communication that the patients are taken care of properly. So I’ll stop there and answer any questions you may have.
ABOUT THE AUTHOR
Daniel P. Petrylak, MD, leads the genitourinary cancers medical oncology team at Smilow Cancer Hospital as director of the genitourinary cancer research group, professor, and co-director of the Cancer Signaling Network program. Dr. Petrylak joined Yale from Herbert Irving Cancer Center at Columbia University Medical Center with New York-Presbyterian Hospital, where he served as Professor of Medicine (Medical Oncology) and Urology and began his appointment in September of 2012. After serving for more than 20 years as the advanced bladder chair for SWOG, Dr. Petrylak is now the Vice Chair of the Genitourinary Committee.