Current Challenges in Upper Tract Urothelial Cancer
Raoul S. Concepcion, MD, FACS presented “Current Challenges in Upper Tract Urothelial Cancer” during the 19th Annual Future Directions in Urology Symposium on August 11, 2018 in Colorado Springs, Colorado.
How to cite: Concepcion, Raoul S. “Current Challenges in Upper Tract Urothelial Cancer” August 11, 2018. Accessed [date today]. https://grandroundsinurology.com/updates-on-upper-tract-urothelial-cancer/
Current Challenges in Upper Tract Urothelial Cancer – Summary:
Raoul S. Concepcion, MD, FACS, provides a brief overview of the background, incidence, and epidemiology of upper tract urothelial carcinoma (UTUC). He then discusses indications for nephroureterectomy with bladder cuff excision and possible methods for management that would be less invasive for low-grade UTUC patients.
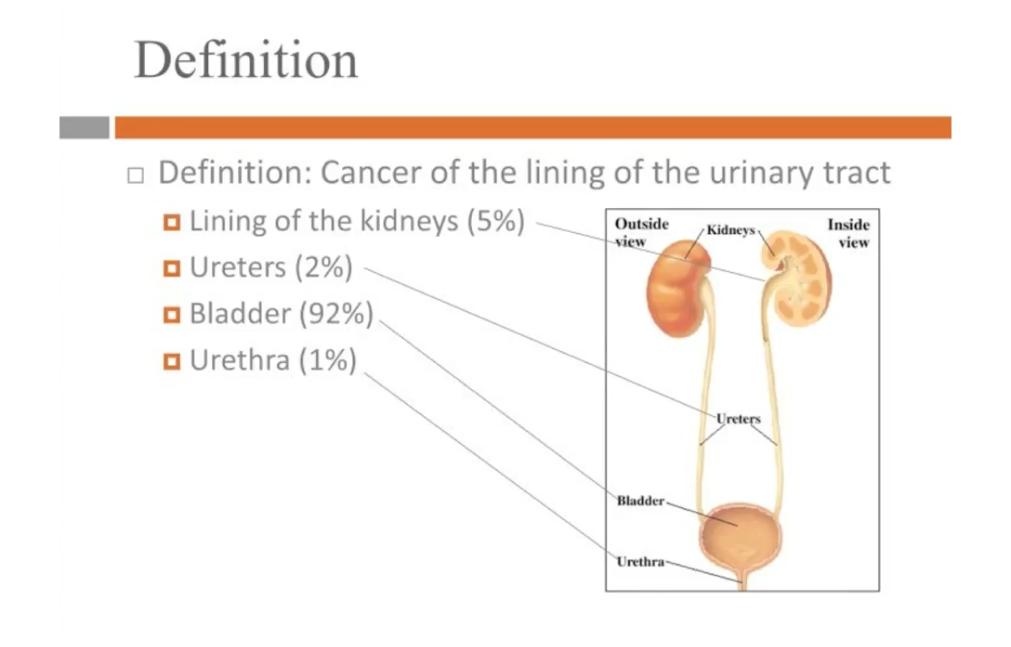
Background of Urothelial Cancers
Urothelial carcinoma refers to cancer in the lining of the urinary tract, which extends to the kidney, ureter, bladder, proximal urethra, and sometimes into the prostatic ducts. The incidence of urothelial tumors, in general, is 79,000 new cases each year. Bladder cancer accounts for 92% of these case. Furthermore, tumors on the lining of the kidney accounts for 5% of these cases, tumors in the ureter account for 2%, and tumors in the urethra account for 1%.
The mean age of patients with UTUC is 73 years, affecting men at a higher rate than it does women. The disease occurs in both upper tracts 3% of the time, and concurrently with bladder cancer 17% of the time. Bladder tumors ascend and develop into UTUC 2%-4% of the time. Patients with carcinoma in situ (CIS), ascend and develop into UTUC in 20-25% of the time at 10 years. Conversely, UTUC will descend into the bladder 22%-47% of the time. Also, up to 21% of UTUC cases may be associated with Lynch Syndrome, which is the most common inherited cancer syndrome. Therefore, physicians need to be aware of family history when assessing patients for UTUC.
Although UTUC is morphologically similar to bladder cancer, these two malignancies are phenotypically and phenotypically different. UTUC show more microsatellite instability and hypomethylation than bladder cancer does. UTUC also presents with muscle invasive disease 60% or the time, while bladder cancer presents with muscle invasive disease 15%-20% of the time.
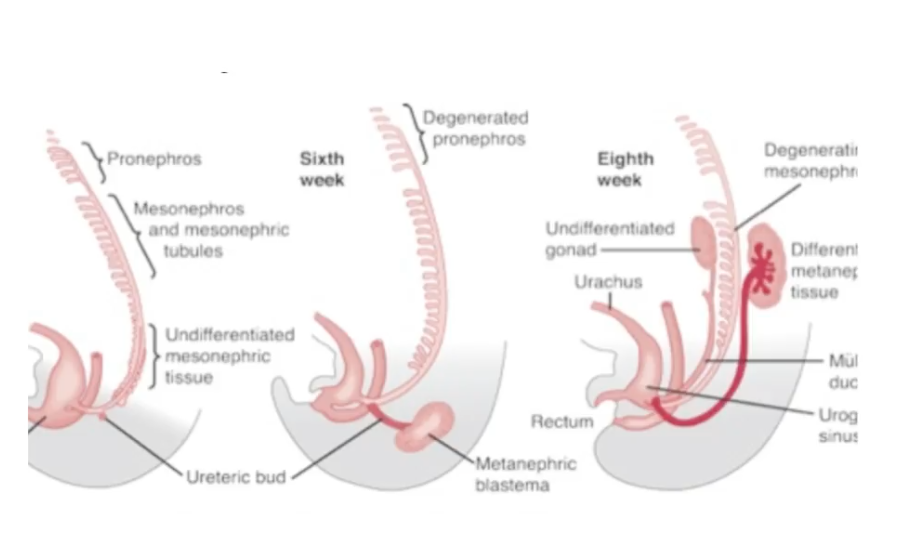
One explanation for the similarities, yet slight differences between bladder cancer and UTUC could be due to the embryologic differentiation of the upper tract through the formation of the ureteric bud and metanephric blastema.
Mechanical Challenges in Imaging and Accessing Ureter Tumors
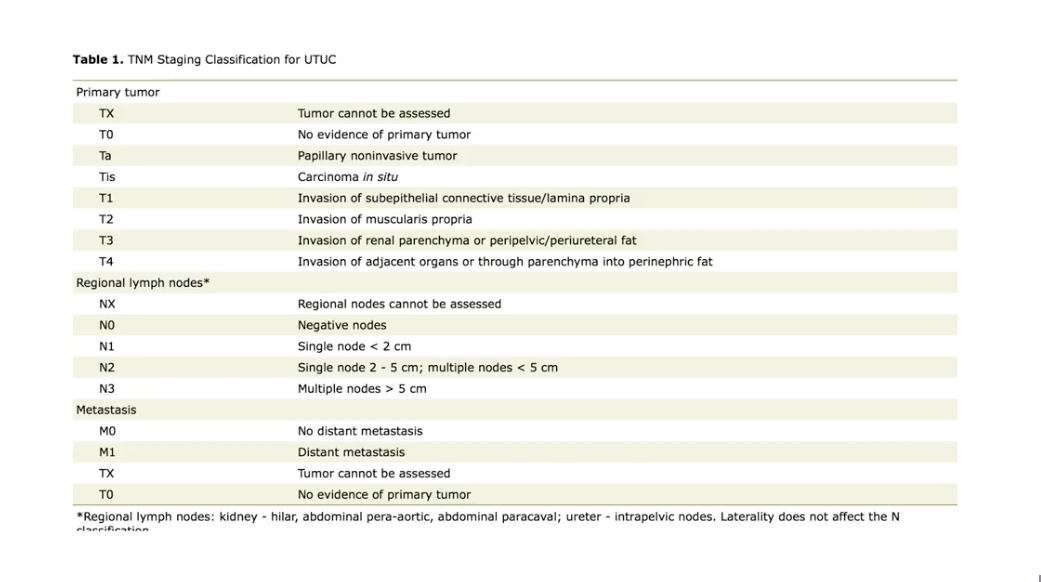
The figure to the left lists the TNM staging classifications for UTUC. Accurately staging these tumors can be difficult due to the anatomy of the ureters. The ureters are a pliable, narrow conduits with little muscle, making them a difficult area for physicians to access. The anatomy of the renal pelvis poses accessibility challenges, as well.
Traditionally, physicians have found UTUC through large filling defects in the upper tract using intravenous (IV) urography. The current method for identifying these large filling defects is utilizing computed tomography (CT) scans. Additionally, in the past, physicians dilated the ureters with balloons to access tumors. However, this method damaged the mucosa of the ureters. The advent of fiber optics and flexible ureteroscopes has greatly improved UTUC imaging techniques. Unfortunately, the practical application of flexible ureteroscopy is challenging. Moreover, while this method may allow a physician to see a tumor, it may not provide access enough for a physician to properly manage the tumor.
Nephroureterectomy with a Cuff of Bladder
The 2018 National Comprehensive Cancer Network (NCCN) guidelines for both UTUC of the ureters and renal pelvis tumors indicate nephroureterectomy with bladder cuff excision for all grades of tumors, even low-grade. This surgery includes a cuff of bladder due to the high recurrence rate of these cancers, which is about 30% in high-grade tumors. However, this procedure is rather invasive for low-grade tumors.
Neoadjuvant Platinum-based Chemotherapy Preceding Nephroureterectomy
A small, retrospective trial by Kobayashi et al. analyzed 55 patients with UTUC clinically involving regional lymph nodes. Out of these patients, 24 received neoadjuvant chemotherapy (NAC) followed by radical nephroureterectomy (RNU), while 31 received RNU alone. The 5-year overall survival rate was 44% in the NAC plus RNU group and 29% in the RNU alone group.
Non-surgical Management of Low-grade UTUC – The OLYMPUS Trial
Due to the challenges and recurrence rates associated with endoscopic resection and ablation of low-grade UTUC, and the invasiveness of RNU, the prospective, phase III OLYMPUS trial is investigating chemical ablation of low-grade UTUC with mitomycin (brand name MitoGel™). This trial is still accruing, but of the current participants, 9 had unreachable tumors at baseline. The included patients must be treatment naive or recurrent with at least one measurable tumor. Patients receive doses of MitoGel™ via retrograde catheter under fluoroscopy. The primary endpoint of this trial is percentage of patients with complete response, with a clinically meaningful outcome defined as around 20%. The OLYMPUS Interim Analysis Conclusions show that this therapy method seems to be safe, feasible, associated with an acceptable adverse event profile. Preliminary efficacy data suggests that primary chemoablation may be possible, but this trial needs further follow up to assess durability of complete response.
In the future, utilizing this drug as an intravesical therapy may be a possibility for low-grade UTUC, as well.
ABOUT THE AUTHOR
Raoul S. Concepcion, MD, FACS, is the Chief Science Officer of U.S. Urology Partners in Nolensville, Tennessee. He was a resident in General Surgery and Urology at Vanderbilt University from 1984-1990, and later served as a Clinical Associate Professor of Urology there.
Dr. Concepcion’s clinical interests revolve around advanced prostate and bladder cancer management. He is a past President of LUGPA. Along with two other urologists, he founded CUSP, a urologic research consortium in the United States. Additionally, he is an advisor and/or speaker for many companies, including Dendreon, Pfizer, Astellas, Amgen, Cellay, and Janssen, and has served as editor for Urologists in Cancer Care.